Abstract
Purpose
This study retrospectively determined magnetic resonance (MR), MR cholangiopancreatography (MRCP) and secretin-MRCP findings in patients with autoimmune pancreatitis (AIP).
Materials and methods
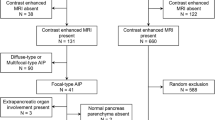
The MR examinations of 28 patients with histopathologically proven AIP were reviewed. In 14 cases, secretin-enhanced MRCP was performed. The observers evaluated pancreatic parenchymal enlargement, signal intensity abnormalities, enhancement, vascular involvement, bile-duct diameter and main pancreatic duct (MPD) narrowing (diffuse/focal/segmental). After secretin administration, the presence of the “duct-penetrating” sign was evaluated.
Results
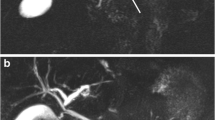
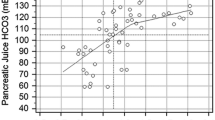
MR imaging showed diffuse pancreatic enlargement in 8/28(29%) cases, focal pancreatic enlargement in 16/28 (57%) cases and no enlargement in 4/28 (14%) cases. The alteration of pancreatic signal intensity was diffuse in 8/28 (29%) cases (eight diffuse AIP) and focal in 20/28 (71%) cases (20 focal AIP). Delayed pancreatic enhancement was present in all AIP, with peripheral rim of enhancement in 8/28 (29%) AIP (1/8 diffuse, 7/20 focal); vascular encasement was present in 7/28 (25%) AIP (1/8 diffuse, 6/20 focal); distal common bile duct narrowing was present in 12/28(43%) AIP (5/8 diffuse, 7/20 focal). MRCP showed MPD narrowing in 17/28 (61%) AIP (4/8 diffuse, 15/20 focal), MPD dilation in 8/28(29%) AIP (3/8 diffuse, 5/20 focal) and normal MPD in1/8 diffuse AIP. Secretin-MRCP showed the duct-penetrating sign in 6/14(43%) AIP (one diffuse AIP with MPD segmental narrowing, five focal AIP with MPD focal narrowing), demonstrating integrity of the MPD.
Conclusions
Delayed enhancement and MPD stenosis are suggestive for AIP on MR and MRCP imaging. Secretin-enhanced MRCP is a problem-solving tool in the differential diagnosis between focal AIP and ductal adenocarcinoma.
Riassunto
Obiettivo
Scopo di questo lavoro è stato valutare i rilievi di pancreatite autoimmune (AIP) nella revisione retrospettiva delle immagini di risonanza magnetica (RM), colangiopancreatografia-RM (CPRM) e CPRM con secretina.
Materiali e metodi
È stata valutata l’indagine RM di 28 pazienti con diagnosi patologica di AIP; in 14 casi è stato espletato l’esame CPRM con somministrazione di secretina. Le immagini sono state analizzate considerando i seguenti parametri: volume del pancreas, alterazioni dell’intensità di segnale del parenchima, impregnazione del pancreas, coinvolgimento vascolare, calibro delle vie biliari e restringimento (diffuso/focale/segmentale) del dotto pancreatico principale (DPP). Dopo somministrazione di secretina, è stata verificata la presenza del segno del “dotto penetrante”.
Risultati
L’esame RM ha evidenziato un incremento dimensionale diffuso del pancreas in 8/28 (29%) casi, un ingrandimento di una parte del pancreas - focale - in 16/28 (57%) casi e pancreas di regolare dimensione in 4/28 (14%) casi. L’alterazione dell’intensità di segnale del pancreas era diffusa in 8/28 (29%) casi (8 AIP di tipo diffuso) e focale in 20/28 (71%) casi (20 AIP di tipo focale). Impregnazione pancreatica tardiva con “cercine” periferico iperintenso si è rilevata in 8/28 (29%) AIP (1/8 AIP di tipo diffuso, 7/20 AIP di tipo focale); “encasement” vascolare è stato dimostrato in 7/28 (25%) AIP (1/8 AIP di tipo diffuso, 6/20 AIP di tipo focale); restringimento del dotto biliare comune è stato rilevato in 12/28 (43%) AIP (5/8 AIP di tipo diffuso, 7/20 AIP di tipo focale). L’esame CPRM ha mostrato restringimento del DPP in 17/28 (61%) AIP (4/8 AIP di tipo diffuso, 15/20 AIP di tipo focale), dilatazione del DPP in 8/28 (29%) AIP (3/8 AIP di tipo diffuso, 5/20 AIP di tipo focale), e DPP normale in 1 AIP di tipo diffuso. L’esame CPRM con secretina ha fatto rilevare il segno del “dotto penetrante” in 6/14 (43%) AIP (1 caso di AIP diffusa con restringimento segmentale del DPP, 5 casi di AIP focale con restringimento focale del DPP) dimostrano l’integrità del DPP.
Conclusioni
All’indagine RM e CPRM, il pattern di impregnazione tardivo e l’assotigliamento del DPP sono reperti suggestivi di AIP. La somministrazione di secretina durante l’esame CPRM è uno strumento utile nella diagnosi differenziale tra AIP di tipo focale e adenocarcinoma duttale.
Similar content being viewed by others
References/Bibliografia
Cavallini G (1993) Is chronic pancreatitis a primary disease of the pancreatic ducts? A new pathogenetic hypothesis. Ital J Gastroenterol 25:391–396
Pearson RK, Longnecker DS, Chari ST et al (2003) Controversies in clinical pancreatology: autoimmune pancreatitis: does it exist? Pancreas 27:1–13
Okazaki K, Chiba T (2002) Autoimmune related pancreatitis. Gut 51:1–4
Kim KP, Kim MH, Song MH et al (2004) Autoimmune chronic pancreatitis. Am J Gastroenterol 99:1605–1616
Ito K, Koike S, Matsunaga N (2001) MR imaging of pancreatic diseases. Eur J Radiol 38:78–93
Sahani DV, Kalva SP, Farrell J et al (2004) Autoimmune pancreatitis: imaging features. Radiology 233:345–352
To’o KJ, Raman SS, Yu NC et al (2005) Pancreatic and peripancreatic diseases mimicking primary pancreatic neoplasia. Radiographics 25:949–965
Morana G, Tapparelli M, Faccioli N et al (2005) Autoimmune pancreatitis: instrumental diagnosis. JOP 6[1 Suppl]:102–107
Notohara K, Burgart LJ, Yadav D et al (2003) Idiopathic chronic pancreatitis with periductal lymphoplasmacytic infiltration: clinicopathologic features of 35 cases. Am J Surg Pathol 27:1119–1127
Kloppel G, Luttges J, Lohr M et al (2003) Autoimmune pancreatitis: pathological, clinical, and immunological features. Pancreas 27:14–19
Wakabayashi T, Kawaura Y, Satomura Y et al (2003) Clinical and imaging features of autoimmune pancreatitis with focal pancreatic swelling or mass formation: comparison with so-called tumor-forming pancreatitis and pancreatic carcinoma. Am J Gastroenterol 98:2679–2687
Kamisawa T, Egawa N, Nakajima H et al (2003) Clinical difficulties in the differentiation of autoimmune pancreatitis and pancreatic carcinoma. Am J Gastroenterol 98:2694–2699
Manfredi R, Graziani R, Cicero C et al (2008) Autoimmune pancreatitis: CT patterns and their changes after steroid treatment. Radiology 247:435–443
Kamisawa T, Chen PY, Tu Y et al (2006) CPRM and MRI findings in 9 patients with autoimmune pancreatitis. World J Gastroenterol 12:2919–2922
Ichikawa T, Sou H, Araki T et al (2001) Duct-penetrating sign at CPRM: usefulness for differentiating inflammatory pancreatic mass from pancreatic carcinomas. Radiology 221:107–116
Cappeliez O, Delhaye M, Deviere J et al (2000) Chronic pancreatitis: evaluation of pancreatic exocrine function with MR pancreatography after secretin stimulation. Radiology 215:358–364
Yoshida K, Toki F, Takeuchi T et al (1995) Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci 40:1561–1568
Uchida K, Okazaki K, Asada M et al (2003) Case of chronic pancreatitis involving an autoimmune mechanism that extended to retroperitoneal fibrosis. Pancreas 26:92–94
Wakabayashi T, Kawaura Y, Satomura Y et al (2002) Clinical study of chronic pancreatitis with focal irregular narrowing of the main pancreatic duct and mass formation: comparison with chronic pancreatitis showing diffuse irregular narrowing of the main pancreatic duct. Pancreas 25:283–289
Kamisawa T, Funata N, Hayashi Y et al (2003) Close relationship between autoimmune pancreatitis and multifocal fibrosclerosis. Gut 52:683–687
Yang DH, Kim KW, Kim TK et al (2006) Autoimmune pancreatitis: radiologic findings in 20 patients. Abdom Imaging 31:94–102
Horiuchi A, Kawa S, Hamano H et al (2002) ERCP features in 27 patients with autoimmune pancreatitis. Gastrointest Endosc 55:494–499
Irie H, Honda H, Baba S et al (1998) Autoimmune pancreatitis: CT and MR characteristics. AJR Am J Roentgenol 170:1323–1327
Koga Y, Yamaguchi K, Sugitani A et al (2002) Autoimmune pancreatitis starting as a localized form. J Gastroenterol 37:133–137
Zamboni G, Luttges J, Capelli P et al (2004) Histopathological features of diagnostic and clinical relevance in autoimmune pancreatitis: a study on 53 resection specimens and 9 biopsy specimens. Virchows Arch 445:552–563
Weber SM, Cubukeu-Dimopulo O, Palesty JA et al (2003) Lymphoplasmacytic sclerosing pancreatitis: inflammatory mimic of pancreatic carcinoma. J Gastrointest Surg 7:129–137
Procacci C, Carbognin G, Biasiutti C et al (2001) Autoimmune pancreatitis: possibilities of CT characterization. Pancreatology 1:246–253
Johnson PT, Outwater EK (1999) Pancreatic carcinoma versus chronic pancreatitis: dynamic MR imaging. Radiology 212:213–218
Pezzilli R, Casadei R, Calculli L et al (2004) Autoimmune pancreatitis. A case mimicking carcinoma. JOP 5:527–530
Leyendecker JR, Elsayes KM, Gratz BI et al (2002) MR cholangiopancreatography: spectrum of pancreatic duct abnormalities. AJR Am J Roentgenol 179:1465–1471
Matos C, Cappeliez O, Winant C et al (2002) MR imaging of the pancreas: a pictorial tour. Radiographics 22:e2
Matos C, Metens T, Deviere J et al (1997) Pancreatic duct: morphologic and functional evaluation with dynamic MR pancreatography after secretin stimulation. Radiology 203:435–441
Manfredi R, Costamagna G, Brizi MG et al (2000) Severe chronic pancreatitis versus suspected pancreatic disease: dynamic MR cholangiopancreatography after secretin stimulation. Radiology 214:849–855
Fukukura Y, Fujiyoshi F, Sasaki M et al (2002) Pancreatic duct: morphologic evaluation with MR cholangiopancreatography after secretin stimulation. Radiology 222:674–680
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carbognin, G., Girardi, V., Biasiutti, C. et al. Autoimmune pancreatitis: imaging findings on contrast-enhanced MR, MRCP and dynamic secretin-enhanced MRCP. Radiol med 114, 1214–1231 (2009). https://doi.org/10.1007/s11547-009-0452-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-009-0452-0