Abstract
Liver fibrosis features excessive protein accumulation in the liver interstitial space resulting from repeated tissue injury due to chronic liver disease. Liver fibrosis eventually proceeds to cirrhosis and associated complications. So, early diagnosis and staging of liver fibrosis are of vital importance for clinical treatment. Liver biopsy remains the gold standard for the diagnosing and staging of fibrosis, but it is suboptimal due to various limitations. Recently, efforts have been made to migrate toward noninvasive techniques for assessing liver fibrosis. CT is relatively easy to perform, relatively standardized for different scanners, and does not require additional hardware in liver fibrosis staging. MRI is frequently performed to characterize indeterminate liver lesions. Because it does not use ionizing radiation and features high image contrast, its role has increased in the staging of liver fibrosis. More recently, several studies on liver fibrosis staging using deep learning algorithms in CT or MRI have been proposed and have shown meaningful results. In this review, we summarize the basic concept, diagnostic performance, and advantages and limitations of each technique to noninvasively stage liver fibrosis.



Similar content being viewed by others
Data availability
Available.
Change history
27 August 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00261-021-03252-z
References
Bataller R, Brenner DA (2005) Liver fibrosis. J Clin Invest 115 (2):209-218. https://doi.org/10.1172/JCI24282
Asrani SK, Devarbhavi H, Eaton J, Kamath PS (2019) Burden of liver diseases in the world. J Hepatol 70 (1):151-171. https://doi.org/10.1016/j.jhep.2018.09.014
Stepanova M, De Avila L, Afendy M, Younossi I, Pham H, Cable R, Younossi ZM (2017) Direct and Indirect Economic Burden of Chronic Liver Disease in the United States. Clin Gastroenterol Hepatol 15 (5):759–766 e755. https://doi.org/10.1016/j.cgh.2016.07.020
Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24 (2):289-293. https://doi.org/10.1002/hep.510240201
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD, American Association for the Study of Liver D (2009) Liver biopsy. Hepatology 49 (3):1017-1044. https://doi.org/10.1002/hep.22742
Bedossa P, Carrat F (2009) Liver biopsy: the best, not the gold standard. J Hepatol 50 (1):1-3. https://doi.org/10.1016/j.jhep.2008.10.014
Zhang YN, Fowler KJ, Ozturk A, Potu CK, Louie AL, Montes V, Henderson WC, Wang K, Andre MP, Samir AE, Sirlin CB (2020) Liver fibrosis imaging: A clinical review of ultrasound and magnetic resonance elastography. J Magn Reson Imaging 51 (1):25-42. https://doi.org/10.1002/jmri.26716
Lubner MG, Pickhardt PJ (2018) Multidetector Computed Tomography for Retrospective, Noninvasive Staging of Liver Fibrosis. Gastroenterol Clin North Am 47 (3):569-584. https://doi.org/10.1016/j.gtc.2018.04.012
Smith AD, Porter KK, Elkassem AA, Sanyal R, Lockhart ME (2019) Current Imaging Techniques for Noninvasive Staging of Hepatic Fibrosis. AJR Am J Roentgenol 213 (1):77-89. https://doi.org/10.2214/AJR.19.21144
Wu L, Shen Y, Li F (2020) Non-invasive diagnosis of liver fibrosis: A review of current imaging modalities. Gastroenterol Hepatol 43 (4):211-221. https://doi.org/10.1016/j.gastrohep.2019.11.009
Yu JS, Shim JH, Chung JJ, Kim JH, Kim KW (2010) Double contrast-enhanced MRI of viral hepatitis-induced cirrhosis: correlation of gross morphological signs with hepatic fibrosis. Br J Radiol 83 (987):212-217. https://doi.org/10.1259/bjr/70974553
Dodd GD, 3rd, Baron RL, Oliver JH, 3rd, Federle MP (1999) Spectrum of imaging findings of the liver in end-stage cirrhosis: part I, gross morphology and diffuse abnormalities. AJR Am J Roentgenol 173 (4):1031-1036. https://doi.org/10.2214/ajr.173.4.10511173
Ito K, Mitchell DG, Gabata T, Hussain SM (1999) Expanded gallbladder fossa: simple MR imaging sign of cirrhosis. Radiology 211 (3):723-726. https://doi.org/10.1148/radiology.211.3.r99ma31723
Torres WE, Whitmire LF, Gedgaudas-McClees K, Bernardino ME (1986) Computed tomography of hepatic morphologic changes in cirrhosis of the liver. J Comput Assist Tomogr 10 (1):47-50. https://doi.org/10.1097/00004728-198601000-00009
Harbin WP, Robert NJ, Ferrucci JT, Jr. (1980) Diagnosis of cirrhosis based on regional changes in hepatic morphology: a radiological and pathological analysis. Radiology 135 (2):273-283. https://doi.org/10.1148/radiology.135.2.7367613
Furusato Hunt OM, Lubner MG, Ziemlewicz TJ, Munoz Del Rio A, Pickhardt PJ (2016) The Liver Segmental Volume Ratio for Noninvasive Detection of Cirrhosis: Comparison With Established Linear and Volumetric Measures. J Comput Assist Tomogr 40 (3):478-484. https://doi.org/10.1097/RCT.0000000000000389
Pickhardt PJ, Malecki K, Hunt OF, Beaumont C, Kloke J, Ziemlewicz TJ, Lubner MG (2017) Hepatosplenic volumetric assessment at MDCT for staging liver fibrosis. Eur Radiol 27 (7):3060-3068. https://doi.org/10.1007/s00330-016-4648-0
Son JH, Lee SS, Lee Y, Kang BK, Sung YS, Jo S, Yu E (2020) Assessment of liver fibrosis severity using computed tomography-based liver and spleen volumetric indices in patients with chronic liver disease. Eur Radiol 30 (6):3486-3496. https://doi.org/10.1007/s00330-020-06665-4
Smith AD, Branch CR, Zand K, Subramony C, Zhang H, Thaggard K, Hosch R, Bryan J, Vasanji A, Griswold M, Zhang X (2016) Liver Surface Nodularity Quantification from Routine CT Images as a Biomarker for Detection and Evaluation of Cirrhosis. Radiology 280 (3):771-781. https://doi.org/10.1148/radiol.2016151542
Smith A, Varney E, Zand K, Lewis T, Sirous R, York J, Florez E, Abou Elkassem A, Howard-Claudio CM, Roda M, Parker E, Scortegagna E, Joyner D, Sandlin D, Newsome A, Brewster P, Lirette ST, Griswold M (2018) Precision analysis of a quantitative CT liver surface nodularity score. Abdom Radiol (NY) 43 (12):3307-3316. https://doi.org/10.1007/s00261-018-1617-x
Smith AD, Zand KA, Florez E, Sirous R, Shlapak D, Souza F, Roda M, Bryan J, Vasanji A, Griswold M, Lirette ST (2017) Liver Surface Nodularity Score Allows Prediction of Cirrhosis Decompensation and Death. Radiology 283 (3):711-722. https://doi.org/10.1148/radiol.2016160799
Pickhardt PJ, Malecki K, Kloke J, Lubner MG (2016) Accuracy of Liver Surface Nodularity Quantification on MDCT as a Noninvasive Biomarker for Staging Hepatic Fibrosis. AJR Am J Roentgenol 207 (6):1194-1199. https://doi.org/10.2214/AJR.16.16514
Catania R, Furlan A, Smith AD, Behari J, Tublin ME, Borhani AA (2021) Diagnostic value of MRI-derived liver surface nodularity score for the non-invasive quantification of hepatic fibrosis in non-alcoholic fatty liver disease. Eur Radiol 31 (1):256-263. https://doi.org/10.1007/s00330-020-07114-y
Kim SW, Kim YR, Choi KH, Cho EY, Song JS, Kim JE, Kim TH, Lee YH, Yoon KH (2020) Staging of Liver Fibrosis by Means of Semiautomatic Measurement of Liver Surface Nodularity in MRI. AJR Am J Roentgenol 215 (3):624-630. https://doi.org/10.2214/AJR.19.22041
Pickhardt PJ, Graffy PM, Said A, Jones D, Welsh B, Zea R, Lubner MG (2019) Multiparametric CT for Noninvasive Staging of Hepatitis C Virus-Related Liver Fibrosis: Correlation With the Histopathologic Fibrosis Score. AJR Am J Roentgenol 212 (3):547-553. https://doi.org/10.2214/AJR.18.20284
Lubner MG, Jones D, Said A, Kloke J, Lee S, Pickhardt PJ (2018) Accuracy of liver surface nodularity quantification on MDCT for staging hepatic fibrosis in patients with hepatitis C virus. Abdom Radiol (NY) 43 (11):2980-2986. https://doi.org/10.1007/s00261-018-1572-6
Lo GC, Besa C, King MJ, Kang M, Stueck A, Thung S, Wagner M, Smith AD, Taouli B (2017) Feasibility and reproducibility of liver surface nodularity quantification for the assessment of liver cirrhosis using CT and MRI. Eur J Radiol Open 4:95-100. https://doi.org/10.1016/j.ejro.2017.07.001
Ronot M, Leporq B, Van Beers BE, Vilgrain V (2020) CT and MR perfusion techniques to assess diffuse liver disease. Abdom Radiol (NY) 45 (11):3496-3506. https://doi.org/10.1007/s00261-019-02338-z
Wm T, L S, C K, K E, T H, H B, T K, K N, M H, S K (2019) Quantification of Hemodynamic Changes in Chronic Liver Disease: Correlation of Perfusion-CT Data with Histopathologic Staging of Fibrosis. Acad Radiol 26 (9):1174-1180. https://doi.org/10.1016/j.acra.2018.11.009
Bonekamp D, Bonekamp S, Geiger B, Kamel IR (2012) An elevated arterial enhancement fraction is associated with clinical and imaging indices of liver fibrosis and cirrhosis. J Comput Assist Tomogr 36 (6):681-689. https://doi.org/10.1097/RCT.0b013e3182702ee3
Van Beers BE, Leconte I, Materne R, Smith AM, Jamart J, Horsmans Y (2001) Hepatic perfusion parameters in chronic liver disease: dynamic CT measurements correlated with disease severity. AJR Am J Roentgenol 176 (3):667-673. https://doi.org/10.2214/ajr.176.3.1760667
Ronot M, Asselah T, Paradis V, Michoux N, Dorvillius M, Baron G, Marcellin P, Van Beers BE, Vilgrain V (2010) Liver fibrosis in chronic hepatitis C virus infection: differentiating minimal from intermediate fibrosis with perfusion CT. Radiology 256 (1):135-142. https://doi.org/10.1148/radiol.10091295
Heye T, Davenport MS, Horvath JJ, Feuerlein S, Breault SR, Bashir MR, Merkle EM, Boll DT (2013) Reproducibility of dynamic contrast-enhanced MR imaging. Part I. Perfusion characteristics in the female pelvis by using multiple computer-aided diagnosis perfusion analysis solutions. Radiology 266 (3):801–811. https://doi.org/10.1148/radiol.12120278
Heye T, Merkle EM, Reiner CS, Davenport MS, Horvath JJ, Feuerlein S, Breault SR, Gall P, Bashir MR, Dale BM, Kiraly AP, Boll DT (2013) Reproducibility of dynamic contrast-enhanced MR imaging. Part II. Comparison of intra- and interobserver variability with manual region of interest placement versus semiautomatic lesion segmentation and histogram analysis. Radiology 266 (3):812–821. https://doi.org/10.1148/radiol.12120255
Bahl G, Cruite I, Wolfson T, Gamst AC, Collins JM, Chavez AD, Barakat F, Hassanein T, Sirlin CB (2012) Noninvasive classification of hepatic fibrosis based on texture parameters from double contrast-enhanced magnetic resonance images. J Magn Reson Imaging 36 (5):1154-1161. https://doi.org/10.1002/jmri.23759
Lubner MG, Smith AD, Sandrasegaran K, Sahani DV, Pickhardt PJ (2017) CT Texture Analysis: Definitions, Applications, Biologic Correlates, and Challenges. Radiographics 37 (5):1483-1503. https://doi.org/10.1148/rg.2017170056
Lubner MG, Jones D, Kloke J, Said A, Pickhardt PJ (2019) CT texture analysis of the liver for assessing hepatic fibrosis in patients with hepatitis C virus. Br J Radiol 92 (1093):20180153. https://doi.org/10.1259/bjr.20180153
Lubner MG, Malecki K, Kloke J, Ganeshan B, Pickhardt PJ (2017) Texture analysis of the liver at MDCT for assessing hepatic fibrosis. Abdom Radiol (NY) 42 (8):2069-2078. https://doi.org/10.1007/s00261-017-1096-5
Budai BK, Toth A, Borsos P, Frank VG, Shariati S, Fejer B, Folhoffer A, Szalay F, Berczi V, Kaposi PN (2020) Three-dimensional CT texture analysis of anatomic liver segments can differentiate between low-grade and high-grade fibrosis. BMC Med Imaging 20 (1):108. https://doi.org/10.1186/s12880-020-00508-w
Yoon JH, Lee JM, Klotz E, Jeon JH, Lee KB, Han JK, Choi BI (2015) Estimation of hepatic extracellular volume fraction using multiphasic liver computed tomography for hepatic fibrosis grading. Invest Radiol 50 (4):290-296. https://doi.org/10.1097/RLI.0000000000000123
Zissen MH, Wang ZJ, Yee J, Aslam R, Monto A, Yeh BM (2013) Contrast-enhanced CT quantification of the hepatic fractional extracellular space: correlation with diffuse liver disease severity. AJR Am J Roentgenol 201 (6):1204-1210. https://doi.org/10.2214/AJR.12.10039
Ito E, Sato K, Yamamoto R, Sakamoto K, Urakawa H, Yoshimitsu K (2020) Usefulness of iodine-blood material density images in estimating degree of liver fibrosis by calculating extracellular volume fraction obtained from routine dual-energy liver CT protocol equilibrium phase data: preliminary experience. Jpn J Radiol 38 (4):365-373. https://doi.org/10.1007/s11604-019-00918-z
Shinagawa Y, Sakamoto K, Sato K, Ito E, Urakawa H, Yoshimitsu K (2018) Usefulness of new subtraction algorithm in estimating degree of liver fibrosis by calculating extracellular volume fraction obtained from routine liver CT protocol equilibrium phase data: Preliminary experience. Eur J Radiol 103:99-104. https://doi.org/10.1016/j.ejrad.2018.04.012
Petitclerc L, Sebastiani G, Gilbert G, Cloutier G, Tang A (2017) Liver fibrosis: Review of current imaging and MRI quantification techniques. J Magn Reson Imaging 45 (5):1276-1295. https://doi.org/10.1002/jmri.25550
Kim YS, Jang YN, Song JS (2018) Comparison of gradient-recalled echo and spin-echo echo-planar imaging MR elastography in staging liver fibrosis: a meta-analysis. Eur Radiol 28 (4):1709-1718. https://doi.org/10.1007/s00330-017-5149-5
Xiao G, Zhu S, Xiao X, Yan L, Yang J, Wu G (2017) Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: A meta-analysis. Hepatology 66 (5):1486-1501. https://doi.org/10.1002/hep.29302
Han MAT, Vipani A, Noureddin N, Ramirez K, Gornbein J, Saouaf R, Baniesh N, Cummings-John O, Okubote T, Setiawan VW, Rotman Y, Loomba R, Alkhouri N, Noureddin M (2020) MR elastography-based liver fibrosis correlates with liver events in nonalcoholic fatty liver patients: A multicenter study. Liver Int 40 (9):2242-2251. https://doi.org/10.1111/liv.14593
Shi Y, Xia F, Li QJ, Li JH, Yu B, Li Y, An H, Glaser KJ, Tao S, Ehman RL, Guo QY (2016) Magnetic Resonance Elastography for the Evaluation of Liver Fibrosis in Chronic Hepatitis B and C by Using Both Gradient-Recalled Echo and Spin-Echo Echo Planar Imaging: A Prospective Study. Am J Gastroenterol 111 (6):823-833. https://doi.org/10.1038/ajg.2016.56
Yasar TK, Wagner M, Bane O, Besa C, Babb JS, Kannengiesser S, Fung M, Ehman RL, Taouli B (2016) Interplatform reproducibility of liver and spleen stiffness measured with MR elastography. J Magn Reson Imaging 43 (5):1064-1072. https://doi.org/10.1002/jmri.25077
Shire NJ, Yin M, Chen J, Railkar RA, Fox-Bosetti S, Johnson SM, Beals CR, Dardzinski BJ, Sanderson SO, Talwalkar JA, Ehman RL (2011) Test-retest repeatability of MR elastography for noninvasive liver fibrosis assessment in hepatitis C. J Magn Reson Imaging 34 (4):947-955. https://doi.org/10.1002/jmri.22716
Kim DW, Kim SY, Yoon HM, Kim KW, Byun JH (2020) Comparison of technical failure of MR elastography for measuring liver stiffness between gradient-recalled echo and spin-echo echo-planar imaging: A systematic review and meta-analysis. J Magn Reson Imaging 51 (4):1086-1102. https://doi.org/10.1002/jmri.26918
Kennedy P, Wagner M, Castera L, Hong CW, Johnson CL, Sirlin CB, Taouli B (2018) Quantitative Elastography Methods in Liver Disease: Current Evidence and Future Directions. Radiology 286 (3):738-763. https://doi.org/10.1148/radiol.2018170601
Iima M, Le Bihan D (2016) Clinical Intravoxel Incoherent Motion and Diffusion MR Imaging: Past, Present, and Future. Radiology 278 (1):13-32. https://doi.org/10.1148/radiol.2015150244
Cece H, Ercan A, Yildiz S, Karakas E, Karakas O, Boyaci FN, Aydogan T, Karakas EY, Cullu N, Ulas T (2013) The use of DWI to assess spleen and liver quantitative ADC changes in the detection of liver fibrosis stages in chronic viral hepatitis. Eur J Radiol 82 (8):e307-312. https://doi.org/10.1016/j.ejrad.2013.02.022
Bonekamp S, Torbenson MS, Kamel IR (2011) Diffusion-weighted magnetic resonance imaging for the staging of liver fibrosis. J Clin Gastroenterol 45 (10):885-892. https://doi.org/10.1097/MCG.0b013e318223bd2c
Wang QB, Zhu H, Liu HL, Zhang B (2012) Performance of magnetic resonance elastography and diffusion-weighted imaging for the staging of hepatic fibrosis: A meta-analysis. Hepatology 56 (1):239-247. https://doi.org/10.1002/hep.25610
Luciani A, Vignaud A, Cavet M, Nhieu JT, Mallat A, Ruel L, Laurent A, Deux JF, Brugieres P, Rahmouni A (2008) Liver cirrhosis: intravoxel incoherent motion MR imaging--pilot study. Radiology 249 (3):891-899. https://doi.org/10.1148/radiol.2493080080
Yoon JH, Lee JM, Baek JH, Shin CI, Kiefer B, Han JK, Choi BI (2014) Evaluation of hepatic fibrosis using intravoxel incoherent motion in diffusion-weighted liver MRI. J Comput Assist Tomogr 38 (1):110-116. https://doi.org/10.1097/RCT.0b013e3182a589be
Jiang H, Chen J, Gao R, Huang Z, Wu M, Song B (2017) Liver fibrosis staging with diffusion-weighted imaging: a systematic review and meta-analysis. Abdom Radiol (NY) 42 (2):490-501. https://doi.org/10.1007/s00261-016-0913-6
Ren H, Liu Y, Lu J, An W, Wang W, Yan T, Li Y, Dong J, Cai J (2020) Evaluating the clinical value of MRI multi-model diffusion-weighted imaging on liver fibrosis in chronic hepatitis B patients. Abdom Radiol (NY). https://doi.org/10.1007/s00261-020-02806-x
Seo N, Chung YE, Park YN, Kim E, Hwang J, Kim MJ (2018) Liver fibrosis: stretched exponential model outperforms mono-exponential and bi-exponential models of diffusion-weighted MRI. Eur Radiol 28 (7):2812-2822. https://doi.org/10.1007/s00330-017-5292-z
Xie S, Li Q, Cheng Y, Zhou L, Xia S, Li J, Shen W (2020) Differentiating mild and substantial hepatic fibrosis from healthy controls: a comparison of diffusion kurtosis imaging and conventional diffusion-weighted imaging. Acta Radiol 61 (8):1012-1020. https://doi.org/10.1177/0284185119889566
Shin MK, Song JS, Hwang SB, Hwang HP, Kim YJ, Moon WS (2019) Liver Fibrosis Assessment with Diffusion-Weighted Imaging: Value of Liver Apparent Diffusion Coefficient Normalization Using the Spleen as a Reference Organ. Diagnostics (Basel) 9 (3). https://doi.org/10.3390/diagnostics9030107
Leonhardt M, Keiser M, Oswald S, Kuhn J, Jia J, Grube M, Kroemer HK, Siegmund W, Weitschies W (2010) Hepatic uptake of the magnetic resonance imaging contrast agent Gd-EOB-DTPA: role of human organic anion transporters. Drug Metab Dispos 38 (7):1024-1028. https://doi.org/10.1124/dmd.110.032862
Annet L, Materne R, Danse E, Jamart J, Horsmans Y, Van Beers BE (2003) Hepatic flow parameters measured with MR imaging and Doppler US: correlations with degree of cirrhosis and portal hypertension. Radiology 229 (2):409-414. https://doi.org/10.1148/radiol.2292021128
Hagiwara M, Rusinek H, Lee VS, Losada M, Bannan MA, Krinsky GA, Taouli B (2008) Advanced liver fibrosis: diagnosis with 3D whole-liver perfusion MR imaging--initial experience. Radiology 246 (3):926-934. https://doi.org/10.1148/radiol.2463070077
Ou HY, Bonekamp S, Bonekamp D, Corona-Villalobos CP, Torbenson MS, Geiger B, Kamel IR (2013) MRI arterial enhancement fraction in hepatic fibrosis and cirrhosis. AJR Am J Roentgenol 201 (4):W596-602. https://doi.org/10.2214/AJR.12.10048
Giraudeau C, Leporq B, Doblas S, Lagadec M, Pastor CM, Daire JL, Van Beers BE (2017) Gadoxetate-enhanced MR imaging and compartmental modelling to assess hepatocyte bidirectional transport function in rats with advanced liver fibrosis. Eur Radiol 27 (5):1804-1811. https://doi.org/10.1007/s00330-016-4536-7
Lagadec M, Doblas S, Giraudeau C, Ronot M, Lambert SA, Fasseu M, Paradis V, Moreau R, Pastor CM, Vilgrain V, Daire JL, Van Beers BE (2015) Advanced fibrosis: Correlation between pharmacokinetic parameters at dynamic gadoxetate-enhanced MR imaging and hepatocyte organic anion transporter expression in rat liver. Radiology 274 (2):379-386. https://doi.org/10.1148/radiol.14140313
Leporq B, Daire JL, Pastor CM, Deltenre P, Sempoux C, Schmidt S, Van Beers BE (2018) Quantification of hepatic perfusion and hepatocyte function with dynamic gadoxetic acid-enhanced MRI in patients with chronic liver disease. Clin Sci (Lond) 132 (7):813-824. https://doi.org/10.1042/CS20171131
Yang L, Ding Y, Rao S, Chen C, Wu L, Sheng R, Fu C, Zeng M (2017) Staging liver fibrosis in chronic hepatitis B with T1 relaxation time index on gadoxetic acid-enhanced MRI: Comparison with aspartate aminotransferase-to-platelet ratio index and FIB-4. J Magn Reson Imaging 45 (4):1186-1194. https://doi.org/10.1002/jmri.25440
Kim KA, Park MS, Kim IS, Kiefer B, Chung WS, Kim MJ, Kim KW (2012) Quantitative evaluation of liver cirrhosis using T1 relaxation time with 3 tesla MRI before and after oxygen inhalation. J Magn Reson Imaging 36 (2):405-410. https://doi.org/10.1002/jmri.23620
Hoad CL, Palaniyappan N, Kaye P, Chernova Y, James MW, Costigan C, Austin A, Marciani L, Gowland PA, Guha IN, Francis ST, Aithal GP (2015) A study of T(1) relaxation time as a measure of liver fibrosis and the influence of confounding histological factors. NMR Biomed 28 (6):706-714. https://doi.org/10.1002/nbm.3299
Cassinotto C, Feldis M, Vergniol J, Mouries A, Cochet H, Lapuyade B, Hocquelet A, Juanola E, Foucher J, Laurent F, De Ledinghen V (2015) MR relaxometry in chronic liver diseases: Comparison of T1 mapping, T2 mapping, and diffusion-weighted imaging for assessing cirrhosis diagnosis and severity. Eur J Radiol 84 (8):1459-1465. https://doi.org/10.1016/j.ejrad.2015.05.019
Banerjee R, Pavlides M, Tunnicliffe EM, Piechnik SK, Sarania N, Philips R, Collier JD, Booth JC, Schneider JE, Wang LM, Delaney DW, Fleming KA, Robson MD, Barnes E, Neubauer S (2014) Multiparametric magnetic resonance for the non-invasive diagnosis of liver disease. J Hepatol 60 (1):69-77. https://doi.org/10.1016/j.jhep.2013.09.002
Haimerl M, Utpatel K, Verloh N, Zeman F, Fellner C, Nickel D, Teufel A, Fichtner-Feigl S, Evert M, Stroszczynski C, Wiggermann P (2017) Gd-EOB-DTPA-enhanced MR relaxometry for the detection and staging of liver fibrosis. Sci Rep 7:41429. https://doi.org/10.1038/srep41429
Zhou ZP, Long LL, Qiu WJ, Cheng G, Huang LJ, Yang TF, Huang ZK (2017) Evaluating segmental liver function using T1 mapping on Gd-EOB-DTPA-enhanced MRI with a 3.0 Tesla. BMC Med Imaging 17 (1):20. https://doi.org/10.1186/s12880-017-0192-x
Yoon JH, Lee JM, Kang HJ, Ahn SJ, Yang H, Kim E, Okuaki T, Han JK (2019) Quantitative Assessment of Liver Function by Using Gadoxetic Acid-enhanced MRI: Hepatocyte Uptake Ratio. Radiology 290 (1):125-133. https://doi.org/10.1148/radiol.2018180753
Cui E, Li Q, Wu J, Mei Y, Yu J, Long W, Li Z, Lan Y, Lin F (2020) Combination of hepatocyte fraction and diffusion-weighted imaging as a predictor in quantitative hepatic fibrosis evaluation. Abdom Radiol (NY) 45 (11):3681-3689. https://doi.org/10.1007/s00261-020-02520-8
Wang HQ, Jin KP, Zeng MS, Chen CZ, Rao SX, Ji Y, Fu CX, Sheng RF (2019) Assessing liver fibrosis in chronic hepatitis B using MR extracellular volume measurements: Comparison with serum fibrosis indices. Magn Reson Imaging 59:39-45. https://doi.org/10.1016/j.mri.2019.03.002
Pan S, Wang XQ, Guo QY (2018) Quantitative assessment of hepatic fibrosis in chronic hepatitis B and C: T1 mapping on Gd-EOB-DTPA-enhanced liver magnetic resonance imaging. World J Gastroenterol 24 (18):2024-2035. https://doi.org/10.3748/wjg.v24.i18.2024
Lefebvre T, Petitclerc L, Hebert M, Bilodeau L, Sebastiani G, Olivie D, Gao ZH, Sylvestre MP, Cloutier G, Nguyen BN, Gilbert G, Tang A (2020) MRI cine-tagging of cardiac-induced motion for noninvasive staging of liver fibrosis. J Magn Reson Imaging 51 (5):1570-1580. https://doi.org/10.1002/jmri.26935
House MJ, Bangma SJ, Thomas M, Gan EK, Ayonrinde OT, Adams LA, Olynyk JK, St Pierre TG (2015) Texture-based classification of liver fibrosis using MRI. J Magn Reson Imaging 41 (2):322-328. https://doi.org/10.1002/jmri.24536
Cannella R, Borhani AA, Tublin M, Behari J, Furlan A (2019) Diagnostic value of MR-based texture analysis for the assessment of hepatic fibrosis in patients with nonalcoholic fatty liver disease (NAFLD). Abdom Radiol (NY) 44 (5):1816-1824. https://doi.org/10.1007/s00261-019-01931-6
Feier D, Balassy C, Bastati N, Stift J, Badea R, Ba-Ssalamah A (2013) Liver fibrosis: histopathologic and biochemical influences on diagnostic efficacy of hepatobiliary contrast-enhanced MR imaging in staging. Radiology 269 (2):460-468. https://doi.org/10.1148/radiol.13122482
Li X, Liu H, Wang R, Yang J, Zhang Y, Li C (2020) Gadoxetate-disodium-enhanced magnetic resonance imaging for liver fibrosis staging: a systematic review and meta-analysis. Clin Radiol 75 (4):319 e311–319 e319. https://doi.org/10.1016/j.crad.2019.11.001
Rauscher I, Eiber M, Ganter C, Martirosian P, Safi W, Umgelter A, Rummeny EJ, Holzapfel K (2014) Evaluation of T1rho as a potential MR biomarker for liver cirrhosis: comparison of healthy control subjects and patients with liver cirrhosis. Eur J Radiol 83 (6):900-904. https://doi.org/10.1016/j.ejrad.2014.02.017
Allkemper T, Sagmeister F, Cicinnati V, Beckebaum S, Kooijman H, Kanthak C, Stehling C, Heindel W (2014) Evaluation of fibrotic liver disease with whole-liver T1rho MR imaging: a feasibility study at 1.5 T. Radiology 271 (2):408–415. https://doi.org/10.1148/radiol.13130342
Li RK, Ren XP, Yan FH, Qiang JW, Lin HM, Tao W, Zhao HF, Chen WB (2018) Liver fibrosis detection and staging: a comparative study of T1rho MR imaging and 2D real-time shear-wave elastography. Abdom Radiol (NY) 43 (7):1713-1722. https://doi.org/10.1007/s00261-017-1381-3
Li S, Sun X, Chen M, Ying Z, Wan Y, Pi L, Ren B, Cao Q (2019) Liver Fibrosis Conventional and Molecular Imaging Diagnosis Update. J Liver 8 (1)
Yasaka K, Akai H, Kunimatsu A, Abe O, Kiryu S (2018) Deep learning for staging liver fibrosis on CT: a pilot study. Eur Radiol 28 (11):4578-4585. https://doi.org/10.1007/s00330-018-5499-7
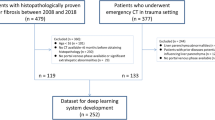
Choi KJ, Jang JK, Lee SS, Sung YS, Shim WH, Kim HS, Yun J, Choi JY, Lee Y, Kang BK, Kim JH, Kim SY, Yu ES (2018) Development and Validation of a Deep Learning System for Staging Liver Fibrosis by Using Contrast Agent-enhanced CT Images in the Liver. Radiology 289 (3):688-697. https://doi.org/10.1148/radiol.2018180763
Ahn Y, Yoon JS, Lee SS, Suk HI, Son JH, Sung YS, Lee Y, Kang BK, Kim HS (2020) Deep Learning Algorithm for Automated Segmentation and Volume Measurement of the Liver and Spleen Using Portal Venous Phase Computed Tomography Images. Korean J Radiol 21 (8):987-997. https://doi.org/10.3348/kjr.2020.0237
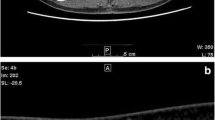
Yasaka K, Akai H, Kunimatsu A, Abe O, Kiryu S (2018) Liver Fibrosis: Deep Convolutional Neural Network for Staging by Using Gadoxetic Acid-enhanced Hepatobiliary Phase MR Images. Radiology 287 (1):146-155. https://doi.org/10.1148/radiol.2017171928
Hectors SJ, Kennedy P, Huang KH, Stocker D, Carbonell G, Greenspan H, Friedman S, Taouli B (2020) Fully automated prediction of liver fibrosis using deep learning analysis of gadoxetic acid-enhanced MRI. Eur Radiol. https://doi.org/10.1007/s00330-020-07475-4
Ahmed Y, Hussein RS, Basha TA, Khalifa AM, Ibrahim AS, Abdelmoaty AS, Abdella HM, Fahmy AS (2020) Detecting liver fibrosis using a machine learning-based approach to the quantification of the heart-induced deformation in tagged MR images. NMR Biomed 33 (1):e4215. https://doi.org/10.1002/nbm.4215
He L, Li H, Dudley JA, Maloney TC, Brady SL, Somasundaram E, Trout AT, Dillman JR (2019) Machine Learning Prediction of Liver Stiffness Using Clinical and T2-Weighted MRI Radiomic Data. AJR Am J Roentgenol 213 (3):592-601. https://doi.org/10.2214/AJR.19.21082
Schawkat K, Ciritsis A, von Ulmenstein S, Honcharova-Biletska H, Jungst C, Weber A, Gubler C, Mertens J, Reiner CS (2020) Diagnostic accuracy of texture analysis and machine learning for quantification of liver fibrosis in MRI: correlation with MR elastography and histopathology. Eur Radiol 30 (8):4675-4685. https://doi.org/10.1007/s00330-020-06831-8
Acknowledgements
This research was supported by “Research Base Construction Fund Support Program” funded by Jeonbuk National University in 2021.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional Review Board approval was not required for this review article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The following sections: Acknowledgment, funding, data availability, conflict of interest and ethical approval were inadvertently missed out in the article while processing the article. However, these sections are included now.
Rights and permissions
About this article
Cite this article
Im, W.H., Song, J.S. & Jang, W. Noninvasive staging of liver fibrosis: review of current quantitative CT and MRI-based techniques. Abdom Radiol 47, 3051–3067 (2022). https://doi.org/10.1007/s00261-021-03181-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03181-x