Abstract
Objective
The purpose of the study was to evaluate the utility of MR texture analysis for differentiating tumor deposits from mesorectal nodes in rectal cancer.
Materials and methods
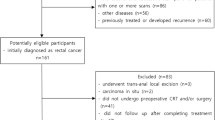
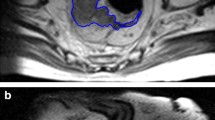
Pretreatment MRI of 40 patients performed between 2006 and 2018 with pathologically proven tumor deposits and/or malignant nodes in the setting of rectal cancer were retrospectively reviewed. In total, 25 tumor deposits (TDs) and 71 positive lymph nodes (LNs) were analyzed for morphological and first-order texture analysis features on T2-weighted axial images. MR morphological features (lesion shape, size, signal heterogeneity, contrast enhancement) were analyzed and agreed in consensus by two experienced radiologists followed by assessment with Fisher’s exact test. Texture analysis of the lesions was performed using TexRAD, a proprietary software algorithm. First-order texture analysis features (mean, standard deviation, skewness, entropy, kurtosis, MPP) were obtained after applying spatial scaling filters (SSF; 0, 2, 3, 4, 5, 6). Univariate analysis was performed with non-parametric Mann–Whitney U test. The results of univariate analysis were reassessed with generalized estimating equations followed by multivariate analysis. Using histopathology as a gold standard, diagnostic accuracy was assessed by obtaining area under the receiver operating curve.
Results
MR morphological parameter, lesion shape was a strong discriminator between TDs and LNs with a p value of 0.02 (AUC: 0.76, 95% CI of 0.66 to 0.84, SE: 0.06) and sensitivity, specificity of 90% and 68%, respectively. Skewness extracted at fine filter (SSF-2) was the only significant texture analysis parameter for distinguishing TDs from LNs with p value of 0.03 (AUC: 0.70, 95% CI of 0.59 to 0.79, SE: 0.06) and sensitivity, specificity of 70% and 72%, respectively. When lesion shape and skewness-2 were combined into a single model, the diagnostic accuracy was improved with AUC of 0.82 (SE: 0.05, 95% CI of 0.72 to 0.88 with p value of < 0.01). This model also showed a high sensitivity of 91% with specificity of 68%.
Conclusion
Lesion shape on MR can be a useful predictor for distinguishing TDs from positive LNs in rectal cancer patients. When interpreted along with MR texture parameter of skewness, accuracy is further improved.



Similar content being viewed by others
Abbreviations
- EMVI:
-
Extramural vascular invasion
- TDs:
-
Tumor deposits
- LNs:
-
Lymph nodes
- SSF:
-
Spatial scaling filter
References
Prabhudesai A, Arif S, Finlayson CJ, Kumar D (2003) Impact of microscopic extranodal tumor deposits on the outcome of patients with rectal cancer. Diseases of the colon and Rectum 46:1531–1537. https://doi.org/10.1007/s10350-004-6809-5
Maguire A, Sheahan K (2014) Controversies in the pathological assessment of colorectal cancer. World J Gastroenterol WJG 20:9850–9861. https://doi.org/10.3748/wjg.v20.i29.9850
Wei X, Qiu M, Zhou Y, He M, Luo H, Wang F, Zhang D, Li Y, Xu R (2016) The clinicopathologic relevance and prognostic value of tumor deposits and the applicability of N1c category in rectal cancer with preoperative radiotherapy. Oncotarget 7:75094–75103. https://doi.org/10.18632/oncotarget.12058
Mirkin KA, Kulaylat AS, Hollenbeak CS, Messaris E (2018) Prognostic Significance of Tumor Deposits in Stage III Colon Cancer. Ann Surg Oncol 25:3179–3184. https://doi.org/10.1245/s10434-018-6661-9
Wong-Chong N, Motl J, Hwang G, Nassif GJJ, Albert MR, Monson JRT, Lee L (2018) Impact of Tumor Deposits on Oncologic Outcomes in Stage III Colon Cancer. Dis Colon Rectum 61:1043. https://doi.org/10.1097/DCR.0000000000001152
Zheng, K., Zheng, N., Xin, C., Zhou, L., Sun, G., Wen, R., Zhang, H., Yu, G., Bai, C., & Zhang, W. (2020). The Prognostic Significance of Tumor Deposit Count for Colorectal Cancer Patients after Radical Surgery. Gastroenterology research and practice, 2020, 2052561. https://doi.org/10.1155/2020/2052561
Basnet, S., Lou, Q. F., Liu, N., Rana, R., Shah, A., Khadka, M., Warrier, H., Sigdel, S., Dhakal, S., Devkota, A., Mishra, R., Sapkota, G., Zheng, L., & Ge, H. Y. (2018). Tumor deposit is an independent prognostic indicator in patients who underwent radical resection for colorectal cancer. Journal of Cancer, 9(21), 3979–3985. https://doi.org/10.7150/jca.27475
Nagayoshi, K., Ueki, T., Nishioka, Y., Manabe, T., Mizuuchi, Y., Hirahashi, M., Oda, Y., & Tanaka, M. (2014). Tumor deposit is a poor prognostic indicator for patients who have stage II and III colorectal cancer with fewer than 4 lymph node metastases but not for those with 4 or more. Diseases of the colon and rectum, 57(4), 467–474. https://doi.org/10.1097/DCR.0000000000000059
Lord A, D’Souza N, Shaw A, Day N, Brown G (2019) The Current Status of Nodal Staging in Rectal Cancer. Curr Colorectal Cancer Rep 15:143–148. https://doi.org/10.1007/s11888-019-00441-3
Horvat N, Carlos Tavares Rocha C, Clemente Oliveira B, Petkovska I, Gollub MJ (2019) MRI of Rectal Cancer: Tumor Staging, Imaging Techniques, and Management. RadioGraphics 39:367–387. https://doi.org/10.1148/rg.2019180114
Varghese BA, Cen SY, Hwang DH, Duddalwar VA (2019) Texture Analysis of Imaging: What Radiologists Need to Know. AJR Am J Roentgenol 212:520–528. https://doi.org/10.2214/AJR.18.20624
Frood R, Palkhi E, Barnfield M, Prestwich R, Vaidyanathan S, Scarsbrook A (2018) Can MR textural analysis improve the prediction of extracapsular nodal spread in patients with oral cavity cancer? Eur Radiol 28:5010–5018. https://doi.org/10.1007/s00330-018-5524-x
Shu Z, Fang S, Ding Z, Mao D, Pang P, Gong X (2018) Application value of texture analysis of magnetic resonance images in prediction of neoadjuvant chemoradiotherapy efficacy for rectal cance]. Zhonghua Wei Chang Wai Ke Za Zhi Chin J Gastrointest Surg 21:1051–1058
Zhang H, Li W, Hu F, Sun Y, Hu T, Tong T (2019) MR texture analysis: potential imaging biomarker for predicting the chemotherapeutic response of patients with colorectal liver metastases. Abdom Radiol 44:65–71 .https://doi.org/10.1007/s00261-018-1682-1
Liu L, Liu Y, Xu L, Li Z, Lv H, Dong N, Li W, Yang Z, Wang Z, Jin E (2017) Application of texture analysis based on apparent diffusion coefficient maps in discriminating different stages of rectal cancer. J Magn Reson Imaging JMRI 45:1798–1808. https://doi.org/10.1002/jmri.25460
Cancer (UK) NCC for (2011) Summary of the 5th edition of the TNM staging system for colorectal cancer and comparison with Dukes’ stage. National Collaborating Centre for Cancer (UK)
Jin M, Roth R, Rock JB, Washington MK, Lehman A, Frankel WL (2015) The Impact of Tumor Deposits on Colonic Adenocarcinoma AJCC TNM Staging and Outcome. Am J Surg Pathol 39:109–115. https://doi.org/10.1097/PAS.0000000000000320
Weiser M. R. (2018). AJCC 8th Edition: Colorectal Cancer. Annals of surgical oncology, 25(6), 1454–1455. https://doi.org/10.1245/s10434-018-6462-1
Huang Y, Liang C, He L, Tian J, Liang C, Chen X, Ma Z, Liu Z (2016) Development and Validation of a Radiomics Nomogram for Preoperative Prediction of Lymph Node Metastasis in Colorectal Cancer. J Clin Oncol 34:2157–2164. https://doi.org/10.1200/JCO.2015.65.9128
Fleshman JW, Smallwood N (2015) Current Concepts in Rectal Cancer. Clin Colon Rectal Surg 28:5–11. https://doi.org/10.1055/s-0035-1545064
Vermeer TA, Orsini RG, Rutten HJT (2014) Surgery for rectal cancer-what is on the horizon? Curr Oncol Rep 16:372. https://doi.org/10.1007/s11912-013-0372-y
Zhang L-N, Xiao W-W, Xi S-Y, OuYang P-Y, You K-Y, Zeng Z-F, Ding P-R, Zhang H-Z, Pan Z-Z, Xu R-H, Gao Y-H (2015) Tumor deposits: markers of poor prognosis in patients with locally advanced rectal cancer following neoadjuvant chemoradiotherapy. Oncotarget 7:6335–6344. https://doi.org/10.18632/oncotarget.6656
Tong L, Gao P, Wang Z, Song Y, Xu Y, Sun Z, Xing C, Xu H (2012) Is the seventh edition of the UICC/AJCC TNM staging system reasonable for patients with tumor deposits in colorectal cancer? Ann Surg 255:208–213. https://doi.org/10.1097/SLA.0b013e31821ad8a2
Goldstein NS, Turner JR (2000) Pericolonic tumor deposits in patients with T3N+MO colon adenocarcinomas: markers of reduced disease-free survival and intra-abdominal metastases and their implications for TNM classification. Cancer 88:2228–2238
Nagtegaal ID, Knijn N, Hugen N, Marshall HC, Sugihara K, Tot T, Ueno H, Quirke P (2017) Tumor Deposits in Colorectal Cancer: Improving the Value of Modern Staging-A Systematic Review and Meta-Analysis. J Clin Oncol Off J Am Soc Clin Oncol 35:1119–1127. https://doi.org/10.1200/JCO.2016.68.9091
Yamano T, Semba S, Noda M, Yoshimura M, Kobayashi M, Hamanaka M, Beppu N, Yano A, Tsukamoto K, Matsubara N, Tomita N (2015) Prognostic significance of classified extramural tumor deposits and extracapsular lymph node invasion in T3–4 colorectal cancer:a retrospective single-center study. BMC Cancer 15:https://doi.org/10.1186/s12885-015-1885-6
Funding
No funding was received for this research study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Atre, I.D., Eurboonyanun, K., Noda, Y. et al. Utility of texture analysis on T2-weighted MR for differentiating tumor deposits from mesorectal nodes in rectal cancer patients, in a retrospective cohort. Abdom Radiol 46, 459–468 (2021). https://doi.org/10.1007/s00261-020-02653-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02653-w