Abstract
Purpose
To explore the value of tumor marker CA125 and CEA linked with conventional ultrasound (US) and contrast-enhanced ultrasound (CEUS) features in differentiating gastrointestinal stromal tumors liver metastases (GISTLM) from colorectal cancer liver metastases (CRCLM).
Materials and methods
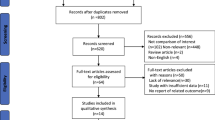
From December 2005 to February 2019, eighty patients with pathologically proven GISTLM together with 80 CRCLM patients were retrospectively evaluated with contrast-enhanced ultrasound (CEUS). Clinical characteristics such as CA125 and CEA were documented to compare the difference between GISTLM and CRCLM. Univariate analysis was performed to determine significant features in ultrasound and then these features were entered into multivariate logistic regression model to determine diagnostic criteria. By analyzing the tumor marker and imaging features, diagnostic performance was evaluated via receiver-operating characteristic (ROC) analysis. The sensitivity, specificity and accuracy were calculated for the diagnosis of GISTLM.
Results
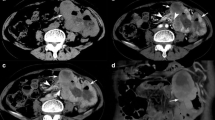
Multiple logistic regression analysis showed that increased CA125 and normal CEA were the independent variables of GISTLM. On conventional US, the features of hypo- or mix-echogenicity and anechoic area were associated with GISTLM. On CEUS, capsule enhancement, starting time of washout > 40 s and proportion of non-enhancement area > 20% were the features indicating GISTLM. All of the p values were < 0.05. When linking tumor marker with imaging features, the diagnostic sensitivity improved from 36.3–57.5% to 70.0%, and the area under the ROC (AUROC) curve improved from 0.681–0.750 to 0.838, with a specificity of 97.5%.
Conclusions
Combining the imaging features of conventional US and CEUS with serum tumor markers provides a potentially effective diagnostic method in differentiation of GISTLM and CRCLM.




Similar content being viewed by others
References
Sandrasegaran K, Rajesh A, Rushing DA, et al. (2005) Gastrointestinal stromal tumors: CT and MRI findings. Eur Radiol, 15(7):1407-1414. https://doi.org/10.1007/s00330-005-2647-7
Gaitanidis A, Alevizakos M, Tsaroucha A, et al. (2018) Incidence and predictors of synchronous liver metastases in patients with gastrointestinal stromal tumors (GISTs). Am J Surg, 216(3):492-497. https://doi.org/10.1016/j.amjsurg.2018.04.011
DeMatteo RP, Lewis JJ, Leung D, et al. (2018) Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg, 231(1):51-58. https://doi.org/10.1097/00000658-200001000-00008
Casali PG, Abecassis N, Bauer S, et al. (2018) Gastrointestinal stromal tumours: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol, 29:68-78. https://doi.org/10.1093/annonc/mdy095
Barrios CH, Blackstein ME, Blay JY, et al. (2015) The GOLD ReGISTry: a Global, Prospective, Observational Registry Collecting Longitudinal Data on Patients with Advanced and Localised Gastrointestinal Stromal Tumours. Eur J Cancer, 51(16):2423-2433. https://doi.org/10.1016/j.ejca.2015.07.010
Herzberg M, Beer M, Anupindi S, et al. (2018) Imaging pediatric gastrointestinal stromal tumor (GIST). J Pediatr Surg, 53(9):1862-1870. https://doi.org/10.1016/j.jpedsurg.2018.03.022
Choi YR, Kim SH, Kim SA, et al. (2014) Differentiation of large (>/= 5 cm) gastrointestinal stromal tumors from benign subepithelial tumors in the stomach: radiologists' performance using CT. Eur J Radiol, 83(2):250-260. https://doi.org/10.1016/j.ejrad.2013.10.028
Coleman JL, Navid F, Furman WL, et al. (2014) Safety of ultrasound contrast agents in the pediatric oncologic population: a single-institution experience. AJR Am J Roentgenol, 202(5):966-970. https://doi.org/10.2214/AJR.13.12010
Dietrich CF, Jenssen C, Hocke M, et al. (2012) Imaging of gastrointestinal stromal tumours with modern ultrasound techniques - a pictorial essay. Z Gastroenterol, 50(5):457-467. https://doi.org/10.1055/s-0031-1282076
Webb A, Scott-Mackie P, Cunningham D, et al. (1995) The prognostic value of CEA, beta HCG, AFP, CA125, CA19-9 and C-erb B-2, beta HCG immunohistochemistry in advanced colorectal cancer. Ann Oncol, 6(6):581-587. https://doi.org/10.1093/oxfordjournals.annonc.a059248
Gao YF, Wang JP, Zhou Y, et al. (2018) Evaluation of Serum CEA, CA19-9, CA72-4, CA125 and Ferritin as Diagnostic Markers and Factors of Clinical Parameters for Colorectal Cancer. Sci Rep, 8:2732. https://doi.org/10.1038/s41598-018-21048-y
Casali PG, Abecassis N, Aro HT, et al: (2018) Gastrointestinal stromal tumours: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol, 29(Suppl 4):iv68-iv78. https://doi.org/10.1093/annonc/mdy320
Glynne-Jones R, Wyrwicz L, Tiret E, et al: (2017) Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol, 28:22-40. https://doi.org/10.1093/annonc/mdx224
Labianca R, Nordlinger B, Beretta GD, et al: (2013) Early colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol, 24 Suppl 6:vi64-72. https://doi.org/10.1093/annonc/mdt354
Claudon M, Dietrich CF, Choi BI, et al. (2013) Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the Liver - Update 2012 A WFUMB-EFSUMB Initiative in Cooperation With Representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med, 34(1):11-29. https://doi.org/10.1055/s-0032-1325499
Hess KR, Varadhachary GR, Taylor SH, et al. (2006) Metastatic patterns in adenocarcinoma. Cancer, 106(7):1624-1633. https://doi.org/10.1002/cncr.21778
Vassos N, Agaimy A, Hohenberger W, et al. (2015) Management of liver metastases of gastrointestinal stromal tumors (GIST). Ann Hepatol, 14(4):531-539. https://doi.org/10.1016/S1665-2681(19)31175-5
Zhao H, Li H, Wang S (1998) The clinicopathological and immunophenotypical features of 162 cases of gastrointestinal stromal tumor. Zhonghua Zhong Liu Za Zhi, 20(4):313-315.
Maestranzi S, Przemioslo R, Mitchell H, et al. (1998) The effect of benign and malignant liver disease on the tumour markers CA19-9 and CEA. Ann Clin Biochem, 35 (Pt 1):99-103. https://doi.org/10.1177/000456329803500113
Zuckerman E, Lanir A, Sabo E, et al. (1999) Cancer antigen 125: A sensitive marker of ascites in patients with liver cirrhosis. Am J Gastroenterol, 94(6):1613-1618.
Epiney M, Bertossa C, Weil A, et al. (2000) CA125 production by the peritoneum: in-vitro and in-vivo studies. Hum Reprod, 15(6):1261-1265. https://doi.org/10.1093/humrep/15.6.1261
Basaran A, Tuncer SZ (2007) Ascites is the primary cause of cancer antigen-125 (CA-125) elevation in systemic lupus erythematosus (SLE) patients with nephrotic syndrome. Med Hypotheses, 68(1):197-201. https://doi.org/10.1016/j.mehy.2006.04.076
Wronski M, Cebulski W, Slodkowski M, et al. (2009) Gastrointestinal stromal tumors: ultrasonographic spectrum of the disease. J Ultrasound Med, 28(7):941-948. https://doi.org/10.7863/jum.2009.28.7.941
Lau S, Tam KF, Kam CK, et al. (2004) Imaging of gastrointestinal stromal tumour (GIST). Clin Radiol, 59(6):487-498. https://doi.org/10.1016/j.crad.2003.10.018
Baheti AD, Shinagare AB, O'Neill AC, et al. (2015) MDCT and clinicopathological features of small bowel gastrointestinal stromal tumours in 102 patients: a single institute experience. Br J Radiol. https://doi.org/10.1259/bjr.20150085
Fukuta N, Kitano M, Maekawa K, et al. (2005) Estimation of the malignant potential of gastrointestinal stromal tumors: the value of contrast-enhanced coded phase-inversion harmonics US. J Gastroenterol, 40(3):247-255. https://doi.org/10.1007/s00535-004-1531-6
Fernandez JA, Sanchez-Canovas ME, Parrilla P (2010) Controversies in the surgical treatment of primary gastrointestinal stromal tumours (GIST). Cir Esp, 88(2):69-80. https://doi.org/10.1016/j.ciresp.2010.01.007
Kong WT, Wang WP, Huang BJ, et al. (2014) Value of wash-in and wash-out time in the diagnosis between hepatocellular carcinoma and other hepatic nodules with similar vascular pattern on contrast-enhanced ultrasound. J Gastroenterol Hepatol, 29(3):576-580. https://doi.org/10.1111/jgh.12394
Murphy-Lavallee J, Jang Hj Fau - Kim TK, Kim Tk Fau - Burns PN, et al. (2007) Are metastases really hypovascular in the arterial phase? The perspective based on contrast-enhanced ultrasonography. J Ultrasound Med, 26(11):1545-1556. https://doi.org/10.7863/jum.2007.26.11.1545
Funding
This study was funded by National Natural Science Foundation of China, 81530055; Guangdong Basic and Applied Basic Research Foundation 2020A1515010653.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None for any of the authors.
Research involving human participants
All procedures performed in studies involving human participants complied with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. For this retrospective study, formal consent was waived.
Informed consent
A waiver of informed consent was obtained from all individual participants included in this retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, D., Zhuang, B., Wang, W. et al. Differential diagnosis of liver metastases of gastrointestinal stromal tumors from colorectal cancer based on combined tumor biomarker with features of conventional ultrasound and contrast-enhanced ultrasound. Abdom Radiol 45, 2717–2725 (2020). https://doi.org/10.1007/s00261-020-02592-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02592-6