Abstract
Background
The diagnostic accuracy of imaging modalities in colorectal cancer liver metastases (CRLM) has improved in recent years, therefore the role of current imaging techniques needs to be defined.
Objective
The aim of this study was to assess the diagnostic performance of magnetic resonance imaging, preoperative imaging (magnetic resonance imaging or computed tomography), intraoperative ultrasound, and contrast-enhanced intraoperative ultrasound in the detection of CRLM.
Materials and methods
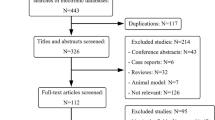
Eligible trials published before 30 March 2020 were identified from the EMBASE, PubMed, Web of Science, and Cochrane Library databases, and descriptive and quantitative data were extracted. Study quality was evaluated for the identified studies and a random-effects model was used to determine the integrated diagnosis estimation. Meta-regression was implemented to explore the possible contributors to heterogeneity.
Results
Overall, 13 studies were included for analysis, comprising 682 patients with a total of 2303 liver lesions. The pooled sensitivity, specificity, and diagnostic odds ratio of contrast-enhanced intraoperative ultrasound were 0.94 (95% confidence interval [CI] 0.89–0.97), 0.83 (95% CI 0.67–0.92), and 79 (95% CI 32–196), respectively. The overall weighted area under the curve was 0.96 (95% CI 0.94–0.97). In univariate meta-regression analysis, disappearing liver metastasis, contrast agent, and Kupffer phase were the potent sources of heterogeneity; however, in multivariate meta-regression, no definite variable was the source of the study heterogeneity.
Conclusion
Contrast-enhanced intraoperative ultrasound demonstrated a high sensitivity and specificity for screening CRLM.





Similar content being viewed by others
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. Mar 2015;65(2):87-108.
Imai K, Allard MA, Benitez CC, et al. Early recurrence after hepatectomy for colorectal liver metastases: what optimal definition and what predictive factors? Oncologist. Jul 2016;21(7):887-894.
Adams RB, Aloia TA, Loyer E, et al. Selection for hepatic resection of colorectal liver metastases: expert consensus statement. HPB. 2013;15(2):91-103.
Mao Y, Chen B, Wang H, et al. Diagnostic performance of magnetic resonance imaging for colorectal liver metastasis: a systematic review and meta-analysis. Sci Rep. 2020;10(1):1969.
Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529-536.
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58(10):982-990.
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol. 2003;56(11):1129-1135.
Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58(9):882-893.
Arita J, Ono Y, Takahashi M, Inoue Y, Takahashi Y, Saiura A. Usefulness of contrast-enhanced intraoperative ultrasound in identifying disappearing liver metastases from colorectal carcinoma after chemotherapy. Ann Surg Oncol. 2014;21 Suppl 3:S390-397.
Arita J, Ono Y, Takahashi M, et al. Routine preoperative liver-specific magnetic resonance imaging does not exclude the necessity of contrast-enhanced intraoperative ultrasound in hepatic resection for colorectal liver metastasis. Ann Surg. 2015;262(6):1086-1091.
Desolneux G, Isambert M, Mathoulin-Pelissier S, et al. Contrast-enhanced intra-operative ultrasound as a clinical decision making tool during surgery for colorectal liver metastases: The ULIIS study. Eur J Surg Oncol. 2019;45(7):1212-1218.
Fioole B, de Haas RJ, Wicherts DA, et al. Additional value of contrast enhanced intraoperative ultrasound for colorectal liver metastases. Eur J Radiol. 2008;67(1):169-176.
Hoareau J, Venara A, Lebigot J, et al. Intraoperative contrast-enhanced ultrasound in colorectal liver metastasis surgery improves the identification and characterization of nodules. World J Surg. 2016;40(1):190-197.
Kartalis N, Brismar TB, Mihocsa L, Isaksson B, Albiin N. The added value of contrast-enhanced ultrasound in patients with colorectal cancer undergoing preoperative evaluation with extensive gadobenate dimeglumine liver MRI. Eur Radiol. 2011;21(10):2067-2073.
Leen E, Ceccotti P, Moug SJ, et al. Potential value of contrast-enhanced intraoperative ultrasonography during partial hepatectomy for metastases: an essential investigation before resection? Ann Surg. 2006;243(2):236-240.
Oba A, Mise Y, Ito H, et al. Clinical implications of disappearing colorectal liver metastases have changed in the era of hepatocyte-specific MRI and contrast-enhanced intraoperative ultrasonography. HPB. Aug 2018;20(8):708-714.
Ruzzenente A, Conci S, Iacono C, et al. Usefulness of contrast-enhanced intraoperative ultrasonography (CE-IOUS) in patients with colorectal liver metastases after preoperative chemotherapy. J Gastrointest Surg. 2013;17(2):281-287.
Takahashi M, Hasegawa K, Arita J, et al. Contrast-enhanced intraoperative ultrasonography using perfluorobutane microbubbles for the enumeration of colorectal liver metastases. Br J Surg. 2012;99(9):1271-1277.
Tani K, Shindoh J, Akamatsu N, et al. Management of disappearing lesions after chemotherapy for colorectal liver metastases: Relation between detectability and residual tumors. J Surg Oncol. 2018;117(2):191-197.
Torzilli G, Del Fabbro D, Palmisano A, et al. Contrast-enhanced intraoperative ultrasonography during hepatectomies for colorectal cancer liver metastases. J Gastrointest Surg. 2005;9(8):1148-1153
Torzilli G, Botea F, Donadon M, et al. Criteria for the selective use of contrast-enhanced intra-operative ultrasound during surgery for colorectal liver metastases. HPB. 2014;16(11):994-1001.
Choi SH, Kim SY, Park SH, et al. Diagnostic performance of CT, gadoxetate disodium-enhanced MRI, and PET/CT for the diagnosis of colorectal liver metastasis: systematic review and meta-analysis. J Magn Reson Imaging. 2018;47(5):1237-1250.
Granata V, Fusco R, di Castelguidone ED, et al. Diagnostic performance of gadoxetic acid-enhanced liver MRI versus multidetector CT in the assessment of colorectal liver metastases compared to hepatic resection. BMC Gastroenterol, 2019; 19(1): 129
Chaubal N, Joshi M, Bam A, Chaubal R. Contrast-enhanced ultrasound of focal liver lesions. Semin Roentgenol. 2016;51(4):334-357.
Hata S, Imamura H, Aoki T, et al. Value of visual inspection, bimanual palpation, and intraoperative ultrasonography during hepatic resection for liver metastases of colorectal carcinoma. World J Surg. 2011;35(12):2779-2787.
Wiering B, Ruers TJ, Krabbe PF, Dekker HM, Oyen WJ. Comparison of multiphase CT, FDG-PET and intra-operative ultrasound in patients with colorectal liver metastases selected for surgery. Ann Surg Oncol. 2007;14(2): 818-826.
Torzilli G, Makuuchi M. Intraoperative ultrasonography in liver cancer. Surg Oncol Clin N Am. 2003;12(1): 91-103.
Tsilimigras DI, Ntanasis-Stathopoulos I, Paredes AZ, et al. Disappearing liver metastases: a systematic review of the current evidence. Surg Oncol. 2019;29:7-13.
Forsberg F, Piccoli CW, Liu JB, et al. Hepatic tumor detection: MR imaging and conventional US versus pulse-inversion harmonic US of NC100100 during its reticuloendothelial system-specific phase. Radiology. 2002; 222(3):824-829.
Hagen EK, Forsberg F, Aksnes AK, et al. Enhanced detection of blood flow in the normal canine prostate using an ultrasound contrast agent. Invest Radiol. 2000;35(2):118-124.
Yanagisawa K, Moriyasu F, Miyahara T, Yuki M, Iijima H. Phagocytosis of ultrasound contrast agent microbubbles by Kupffer cells. Ultrasound Med Biol. 2007;33(2):318-325.
Acknowledgment
No preregistration exists for the reported studies reported in this article. The authors would like to acknowledge Kun Wang, who contributed to the study by making substantial contributions to the acquisition of the data, and Hong-Wei Wang, who made substantial contributions to the analysis and interpretation of the data. Both Kun Wang and Hong-Wei Wang were involved in drafting of the manuscript but do not meet the criteria for authorship.
Funding
This study was supported by grants from the National Nature Science Foundation of China (umbers 81874143 and 31971192), the Beijing Natural Science Foundation (number 7192035), and Capital’s Funds for Health Improvement and Research (number 2020-2-2152).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Potential Conflict of interestThis manuscript has not been previously submitted as a podium or poster presentation. Wei Liu, Zhong-Yi Zhang, Shan-Shan Yin, Kun Yan, and Bao-Cai Xing declare they have no financial or personal relationships with other people or organizations that can inappropriately influence this work, and there are no professional or other personal interests of any nature or kind, for any product, service, and/or company, in relation to this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, W., Zhang, ZY., Yin, SS. et al. Contrast-Enhanced Intraoperative Ultrasound Improved Sensitivity and Positive Predictive Value in Colorectal Liver Metastasis: a Systematic Review and Meta-Analysis. Ann Surg Oncol 28, 3763–3773 (2021). https://doi.org/10.1245/s10434-020-09365-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09365-x