Abstract
Purpose
Autoimmune liver diseases (AILD), including primary sclerosing cholangitis (PSC), autoimmune sclerosing cholangitis (ASC), and autoimmune hepatitis (AIH), have overlapping clinical features but distinct management strategies and outcomes. The purpose of this study was to assess the diagnostic performance of quantitative magnetic resonance cholangiopancreatography (MRCP) parameters for distinguishing PSC/ASC from AIH in children and young adults.
Materials and methods
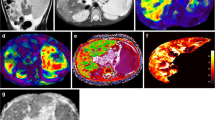
This IRB-approved, cross-sectional study included participants from an institutional AILD registry that underwent baseline serum liver biochemistry testing and 3D fast spin-echo MRCP. The biliary tree was extracted and modeled from MRCP images using novel proprietary software (MRCP+ ™; Perspectum Diagnostics; Oxford, United Kingdom), and quantitative parameters were generated (e.g., biliary tree volume; number and length of bile ducts, strictures, and dilations; bile duct median/maximum diameters). Mann–Whitney U tests were performed to compare laboratory values and MRCP metrics between patient cohorts (clinical diagnosis of PSC/ASC versus AIH). Receiver operating characteristic (ROC) curves and multivariable logistic regression were used to assess diagnostic performance of serum biochemistry values and MRCP parameters for discriminating PSC/ASC from AIH.
Results
Thirty percent (14/47) of MRCP exams failed post-processing due to motion artifact. The remaining 33 patients included 20 males and 13 females, with a mean age of 15.1 ± 3.9 years. Eighteen patients were assigned the clinical diagnosis of PSC or ASC and 15 of AIH. All but one quantitative MRCP parameter were significantly different between cohorts (p < 0.05) and predictive of diagnosis (ROC p < 0.05), including numbers of bile duct strictures (area under curve [AUC] = 0.86, p < 0.0001) and dilations (AUC = 0.87, p < 0.0001) and total length of dilated ducts (AUC = 0.89, p < 0.0001). Laboratory values were not significantly different between cohorts (p > 0.05). The best multivariable model for distinguishing PSC/ASC from AIH included total length of dilated ducts (odds ratio [OR], 1.08; 95% CI 1.02–1.14) and maximum left hepatic duct diameter (OR, 1.21; 95% CI 0.57–2.56) [AUC = 0.92].
Conclusion
Quantitative MRCP parameters provide good discrimination of PSC/ASC from AIH.




Similar content being viewed by others
References
Deneau M, Jensen MK, Holmen J, Williams MS, Book LS, Guthery SL (2013) Primary sclerosing cholangitis, autoimmune hepatitis, and overlap in Utah children: epidemiology and natural history. Hepatology 58 (4):1392-1400. https://doi.org/10.1002/hep.26454
Singh H, Balouch F, Noble C, Lewindon P (2018) Evolving Practice and Changing Phenotype in Pediatric Autoimmune Liver Disease: Outcomes From an Australian Center. J Pediatr Gastroenterol Nutr 67 (1):80-85. https://doi.org/10.1097/mpg.0000000000001927
Gregorio GV, Portmann B, Karani J, Harrison P, Donaldson PT, Vergani D, Mieli-Vergani G (2001) Autoimmune hepatitis/sclerosing cholangitis overlap syndrome in childhood: a 16-year prospective study. Hepatology 33 (3):544-553. https://doi.org/10.1053/jhep.2001.22131
Wilschanski M, Chait P, Wade JA, Davis L, Corey M, St Louis P, Griffiths AM, Blendis LM, Moroz SP, Scully L, et al. (1995) Primary sclerosing cholangitis in 32 children: clinical, laboratory, and radiographic features, with survival analysis. Hepatology 22 (5):1415-1422
Della Corte C, Sartorelli MR, Sindoni CD, Girolami E, Giovannelli L, Comparcola D, Nobili V (2012) Autoimmune hepatitis in children: an overview of the disease focusing on current therapies. Eur J Gastroenterol Hepatol 24 (7):739-746. https://doi.org/10.1097/meg.0b013e328353750c
Manns MP, Czaja AJ, Gorham JD, Krawitt EL, Mieli-Vergani G, Vergani D, Vierling JM, American Association for the Study of Liver D (2010) Diagnosis and management of autoimmune hepatitis. Hepatology 51 (6):2193-2213. https://doi.org/10.1002/hep.23584
Angulo P, Batts KP, Jorgensen RA, LaRusso NA, Lindor KD (2000) Oral budesonide in the treatment of primary sclerosing cholangitis. Am J Gastroenterol 95 (9):2333-2337. https://doi.org/10.1111/j.1572-0241.2000.02323.x
Tischendorf JJ, Hecker H, Kruger M, Manns MP, Meier PN (2007) Characterization, outcome, and prognosis in 273 patients with primary sclerosing cholangitis: A single center study. Am J Gastroenterol 102 (1):107-114. https://doi.org/10.1111/j.1572-0241.2006.00872.x
Wiesner RH, Grambsch PM, Dickson ER, Ludwig J, MacCarty RL, Hunter EB, Fleming TR, Fisher LD, Beaver SJ, LaRusso NF (1989) Primary sclerosing cholangitis: natural history, prognostic factors and survival analysis. Hepatology 10 (4):430-436
Chavhan GB, Roberts E, Moineddin R, Babyn PS, Manson DE (2008) Primary sclerosing cholangitis in children: utility of magnetic resonance cholangiopancreatography. Pediatr Radiol 38 (8):868-873. https://doi.org/10.1007/s00247-008-0918-6
Dave M, Elmunzer BJ, Dwamena BA, Higgins PD (2010) Primary sclerosing cholangitis: meta-analysis of diagnostic performance of MR cholangiopancreatography. Radiology 256 (2):387-396. https://doi.org/10.1148/radiol.10091953
Vitellas KM, El-Dieb A, Vaswani KK, Bennett WF, Tzalonikou M, Mabee C, Kirkpatrick R, Bova JG (2002) MR cholangiopancreatography in patients with primary sclerosing cholangitis: interobserver variability and comparison with endoscopic retrograde cholangiopancreatography. AJR Am J Roentgenol 179 (2):399-407. https://doi.org/10.2214/ajr.179.2.1790399
Zenouzi R, Liwinski T, Yamamura J, Weiler-Normann C, Sebode M, Keller S, Lohse AW, Schramm C, IPSCSG IPSG (2018) Follow-up magnetic resonance imaging/3D-magnetic resonance cholangiopancreatography in patients with primary sclerosing cholangitis: challenging for experts to interpret. Aliment Pharm Ther 48 (2):169-178. https://doi.org/10.1111/apt.14797
Frangi AF, Niessen WJ, Vincken KL, Viergever MA (1998) Multiscale vessel enhancement filtering. Lect Notes Comput Sc 1496 (1496):130-137
Perona P MJ (1990) Scale-space and edge detection using anisotropic diffusion IEEE Transactions on Pattern Analysis and Machine Intelligence 12 (7):629-639
Otsu N (1979) A threshold selection method from gray-level histograms. IEEE Transactions on Systems, Man and Cybernetics 9 (1):62-66
Xu C, Prince JL (1998) Snakes, shapes, and gradient vector flow. IEEE Trans Image Process 7 (3):359-369. https://doi.org/10.1109/83.661186
Chapman R, Fevery J, Kalloo A, Nagorney DM, Boberg KM, Shneider B, Gores GJ, American Association for the Study of Liver D (2010) Diagnosis and management of primary sclerosing cholangitis. Hepatology 51 (2):660-678. https://doi.org/10.1002/hep.23294
Mileti E, Rosenthal P, Peters MG (2012) Validation and modification of simplified diagnostic criteria for autoimmune hepatitis in children. Clin Gastroenterol Hepatol 10 (4):417-421 e411-412. https://doi.org/10.1016/j.cgh.2011.11.030
Schisterman EF, Perkins NJ, Liu A, Bondell H (2005) Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiology 16 (1):73-81
Vitellas KM, Keogan MT, Freed KS, Enns RA, Spritzer CE, Baillie JM, Nelson RC (2000) Radiologic manifestations of sclerosing cholangitis with emphasis on MR cholangiopancreatography. Radiographics 20 (4):959-975; quiz 1108-1109, 1112. https://doi.org/10.1148/radiographics.20.4.g00jl04959
Lindor KD (1997) Ursodiol for primary sclerosing cholangitis. Mayo Primary Sclerosing Cholangitis-Ursodeoxycholic Acid Study Group. N Engl J Med 336 (10):691-695. https://doi.org/10.1056/nejm199703063361003
Acknowledgements
Perspectum diagnostics provided in-kind research support in the form of image analysis for this study. The study was funded by intramural grants from the Center for Translational Fibrosis Research (CTFR) and by the Center for Autoimmune Liver Disease (CALD) at Cincinnati Children’s Hospital Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jonathan Dillman, MD, MSc and Andrew Trout, MD receive authorship royalties from Reed Elsevier and Wolters Kluwer. Andrew Trout, MD is on the speakers bureau for iiCME and Applied Radiology. The remaining authors have no disclosures to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gilligan, L.A., Trout, A.T., Lam, S. et al. Differentiating pediatric autoimmune liver diseases by quantitative magnetic resonance cholangiopancreatography. Abdom Radiol 45, 168–176 (2020). https://doi.org/10.1007/s00261-019-02184-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02184-z