Abstract
Purpose
An accurate postoperative assessment is pivotal to inform postoperative 131I treatment in patients with differentiated thyroid cancer (DTC). We developed a predictive model for post-treatment whole-body scintigraphy (PT-WBS) results (as a proxy for persistent disease) by adopting a decision tree model.
Methods
Age, sex, histology, T stage, N stage, risk classes, remnant estimation, TSH, and Tg were identified as potential predictors and were put into regression algorithm (conditional inference tree, ctree) to develop a risk stratification model for predicting the presence of metastases in PT-WBS.
Results
The lymph node (N) stage identified a partition of the population into two subgroups (N-positive vs N-negative). Among N-positive patients, a Tg value > 23.3 ng/mL conferred a 83% probability to have metastatic disease compared to those with lower Tg values. Additionally, N-negative patients were further substratified in three subgroups with different risk rates according to their Tg values. The model remained stable and reproducible in the iterative process of cross validation.
Conclusions
We developed a simple and robust decision tree model able to provide reliable informations on the probability of persistent/metastatic DTC after surgery. These information may guide post-surgery 131I administration and select patients requiring curative rather than adjuvant 131I therapy schedules.
Similar content being viewed by others
Introduction
A trend towards de-escalating the role of iodine-131 (131I) in the treatment of differentiated thyroid cancer (DTC) emerged after the release of the 2015 edition of the American Thyroid Association (ATA) Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer [1]. Basically, a three-tiered postoperative risk assessment system, primarily based on pathology reports, was proposed to inform decisions on postoperative 131I administration (i.e., ATA risk classes). Such a system, however, cannot detect the presence of postoperative biochemical, structural, or functional persistent disease that require curative 131I administration. Moreover, different options (i.e., wait-and-see, remnant ablation, adjuvant 131I therapy) are available in patients with no evidence of persistent disease. ATA risk classes are relevant in assigning patients to different strategies but additional factors such as local resources and expertise as well as patient’ preferences should be incorporated and discussed, preferably in a multidisciplinary context (i.e., tumor board), in order to do justice to the modern concept of an individualized, targeted therapy [2]. The postoperative application of 131I, which encompasses the integration of diagnostics (i.e., post-treatment whole-body scintigraphy, PT-WBS) and therapeutics, served a long time as the gold standard for detecting persistent disease, assess its 131I avidity, and predict response to 131I, thus enabling personalized management of DTC patients. However, following current standards, the omission of 131I therapy in selected cases prevents the treating physician from obtaining such information; hence, alternative markers are warranted. Thyroglobulin (Tg) is a glycoprotein produced by the thyroid follicular cells roughly related to the amount of thyroid tissue present [3]. In DTC patients who undergo total thyroid ablation (i.e., thyroidectomy and 131I ablation), Tg is a powerful tumor marker and it is monitored to detect persistent or recurrent disease, evaluate disease progression, and provide prognostic informations, respectively [4]. Preablation Tg measurement can accurately determine the likelihood of achieving remission or having persistent or recurrent disease after the initial 131I therapy [5], and was also proposed to assess the postoperative status and guide 131I therapy selection with sparse results [6-8]. As a matter of fact, the predictive value of postoperative Tg is influenced by many factors. These include the time elapsed since surgery, the amount of thyroid remnant [9], the selected Tg cutoff level, and the TSH level at the time of Tg measurement [10-13]. Furthermore, the presence of Tg autoantibodies (TgAb), often “imported” by co-existing thyroid autoimmune diseases, significantly affects the measurable Tg values in up to 25% of DTC patients in the early postoperative period [3, 4, 14]. Accordingly, Tg reference intervals mathematically normalized to TSH levels and estimated amounts of thyroid remnants have been claimed to improve the reliability of postoperative Tg measurement [15, 16]. Moreover, the pre-test individual risk of loco-regional and distant metastases further complicates the issue. As a result, optimal Tg cutoff levels to distinguish normal residual thyroid tissue from persistent thyroid cancer requiring curative 131I administration are not yet available [1, 17, 18]. In the available literature, patients treated with 131I were predominantly grouped together as one cohort, irrespective of whether 131I was carried out in the context of remnant ablation, adjuvant therapy, or as therapy for known metastases. Considering new recommendations, however, early detection of patients with persistent disease after surgery is pivotal to optimize 131I treatment (i.e., patients’ preparation and administered 31I activities) to maximize the treatment effectiveness. First, metastatic DTC cells have lower density and poorer functionality of natrium iodine symporter (NIS) and the TSH elevation over time (i.e., area under the curve of TSH stimulation) is relevant to increase 131I uptake and retention [19]. Accordingly, thyroid hormone withdrawal (THW) is preferable to recombinant human TSH (rhTSH) in these cases (i.e., with the exception of patients who are either unable to elevate endogenous TSH during THW, or in whom THW is contraindicated for medical reason). Second, ablative and adjuvant treatments are performed with 131I activities ranging from 1.1 to 3.7 GBq while treatment of known disease is performed with higher activities ranging from 3.7 to 5.5 GBq for small-volume loco-regional disease and 5.6–7.4 GBq (150–200 mCi) or even more 131I for treatment of advanced locoregional disease and/or small-volume distant metastatic disease. Identification of iodine-avid diffuse metastatic disease may lead to escalation of prescribed therapeutic 131I activity with or without dosimetry calculations [20]. All in all, an accurate postoperative assessment is pivotal to inform our treatments and avoid suboptimal 131I administration (i.e., adjuvant instead of curative strategy). The present study was prompted to develop a predictive model for PT-WBS results (as a proxy for persistent disease) by adopting a decision tree model integrating postoperative TSH and Tg levels, thyroid remnant estimate, patients’ demographic and clinical data, and ATA risk classes, respectively, in a large series of 1317 TgAb-negative DTC patients.
Material and methods
Patients
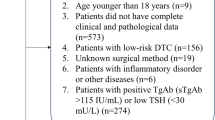
From institutional databases of participating centers, all patients 18 years and older with histologically proved DTC who underwent (near-)/total thyroidectomy and THW-assisted 131I therapy were included. Records without information on (i) TgAb levels; (ii) preablation TSH, Tg, and 24-h radioiodine uptake (RAIU) values within 1 week before 131I therapy; and (iii) post-treatment whole-body scintigraphy (PT-WBS) results were excluded from the present study.
Radioiodine treatment
Patients selected for 131I administration underwent THW and received a 131I activity determined at the discretion of the attending physician according to nuclear medicine guidelines and practice recommendations (median 2.4 GBq, range 1.1–4.5 GBq). Radioprotection issues were managed in strict adherence to national regulations [18, 21].
RAIU testing and post-treatment WBS
All RAIU testing and PT-WBS examinations were performed strictly following the EANM procedure guidelines in all participating centers. Single photon emission computed tomography/computed tomography (SPECT/CT) was performed in addition to PT-WBS at the judgment of attending physicians [22]. The PT-WBS was classified as negative (i.e., absent uptake within the thyroid bed and absent non-physiological uptakes in other regions); remnant only (i.e., uptake within the thyroid bed without non-physiological uptakes in other regions); or positive (pathological uptake outside the thyroid bed, with or without uptake within the thyroid bed).
Laboratory
Serum TSH levels were measured by 2nd or 3rd generation immunoassays on conventional automated analytical platforms. Assays employed to quantify serum Tg and TgAb are reported in Table 1.
Decision tree model
Age, sex, histology, T stage, N stage, ATA risk, RAIU, TSH, and Tg were identified as potential predictors and were put into regression algorithm (conditional inference tree, ctree) to develop a risk stratification model for predicting the presence of metastasis in PT-WBS. Conditional inference tree analysis provides a decision tree by performing recursive population splitting into subgroups according to the specified clinical endpoint. At each partition, the algorithm searches for the best predictor and corresponding cut-off value that split the cohort into two subsequent nodes such that the outcome is significantly different between the two nodes, respectively. The process is iterated for each node until the algorithm cannot find any predictor that leads to significantly different subclasses, thus creating an algorithm for predicting future outcomes within more homogeneous subgroups. The final sets of subpopulations are called terminal nodes. The ctree algorithm allows to include both continuous and categorical variables in the analysis. Additionally, it ranks the relevance of different variables instead of merely focusing on the outcome prediction with less attention to variables’ contribution. To minimize the overfitting, the dataset was divided into training and validation dataset through 200-fold cross validation after a preliminary choice of the most relevant variables. First, we evaluated the most frequently selected parameters by varying the dataset. To this end, the selection of patients to be included in the dataset was iterated 1000 times, maintaining the original proportion of variables and endpoint. The clinical parameters selected in at least the 95% of the iterations were used in the subsequent analysis. In a second step, these parameters were used to build the final model that was then validated by 200-fold cross-validation process applying a splitting ratio 70:30. The correct proportion of variables and events was maintained also in this case. For each iteration, the performance of the model was verified calculating accuracy, positive predictive value (PPV), and negative predictive value (NPV). Since for each iteration, the cutoff value of each node could slightly differ due to different patients; the median and interquartile range of threshold have been evaluated. Finally, the performance of the model was tested for each center to assess the impact of different Tg and TgAb assays.
Statistical analysis
To analyze differences between different groups, χ2 test and Kruskal-Wallis or Mann-Whitney U tests were used for categorical and continuous variables, respectively. Differences were considered statistically significant when P ≤ 0.05. Statistical analyses were carried out with R and the integrated development environment R Studio v 1.2.1335 (RStudio, Inc., Boston, MA, USA). For the conditional inference tree analysis, the ctree function of the party R package was used.
Results
Demographic, clinical, histopathological, and biochemical data included in our statistical model are summarized in Table 2 for the overall series and single series of different participating centers, respectively. Relevant between-center differences emerged for almost all parameters considered in our analysis (Table 2).
Decision tree model
The percentages of analytic cycles in which each variable was selected as predictive of persistent disease in PT-WBS was estimated. Variables selected in more than 95% of cycles were retained in the subsequent analysis. Accordingly, Tg values and N stage were the best predictive parameters in the first analytic round recurring in 100% and 97.4% of 1000 iterative cycles of analysis, respectively (Table 3). In the second step, the 200-fold cross-validation analysis was performed and the algorithm generated a conditional inference tree with five terminal nodes using Tg and N stage as predictive variables as depicted in Fig. 1. According to the decision tree model, in the first node, the N stage identifies a partition of the initial population into two subgroups according to the presence or absence of lymph node involvement. In case of lymph node involvement, patients with a value of Tg higher than 23.3 ng/mL carry a probability of 83% to have persistent/metastatic disease at PT-WBS compared to those with lower Tg values. On the other hand, patients without lymph node involvement are stratified in three risks subgroups according to their Tg values. Particularly, in the absence of lymph node involvement, Tg values exceeding 35 ng/mL predict a positive PT-WBS result in 56.3% of case, while the probability decreases to 15.2% and 5.8%, for Tg values lower than 35 and 7.1 ng/mL, respectively. Our model remained stable and reproducible in the iterative process of cross-validation just showing negligible variations in Tg threshold values selected according to the different patient groups considered by each iteration. The medians and interquartile ranges (IQR) of the Tg thresholds in different nodes are reported in the Table 4. In the training cohorts, the mean accuracy, PPV, and NPV of the generated predictive model were 88%, 68%, and 90%, respectively. Similar performance was also obtained in the validation sets, with accuracy of 88%, PPV of 60%, and NPV of 91% (Table 5). Finally, as summarized in Table 6, the accuracy, NPV, PPV, and AUC values are similar for each center with the exception of center 3 which has a lower PPV compared to other ones likely due to the use of the Roche Tg assay which produces higher results compared to Tg assays employed in other centers [23].
A graphical representation of classification tree: according to the decision tree model lymph node stage (N stage) subdivides the population into two subgroups. In case of lymph node involvement, patients with a value of Tg higher than 23.3 ng/mL carry a probability of 83% to have persistent/metastatic disease compared to those with lower Tg values. Patients without lymph node involvement are stratified in three-risk subgroups according to their Tg values: Tg values exceeding 35 ng/mL predict structural disease in 56.3% of case, while the probability decreases to 15.2% and 5.8%, for Tg values lower than 35 and 7.1 ng/mL, respectively
Discussion
We developed and validated an algorithm to predict whether viable tumor lesions after surgery will be visualized by PT-WBS. Notably, it should be intended as a tool to better select patients that will profit from a more intense treatment with curative intent rather than to “per se” exclude patients from 131I application. Currently, no definitive data exist to safely support the omission of 131I adjuvant treatment in low to intermediate risk DTC. Therefore, clinical decisions should include local factors, patients’ values, and preferences in addition to the conventional risk stratification. As the main result of our study, the combination of lymph node status and Tg values outperformed any other tested factor (i.e., age, sex, T, histology, ATA risk classes, TSH, and RAIU values) in predicting the presence of persistent disease after surgery. This highlights the drawback of ATA risk stratification system alone in predicting postoperative persistent disease and remarks the role of a more sophisticated postoperative assessment of DTC patients [2, 24]. Basing on our data, a decision tree is provided to guide the clinical decision-making dependent on the presence of lymph node involvement and, subsequently, on Tg levels in a different subset of patients. Notably, differences in patient selection, surgical skills, and related post-operative RAIU values (i.e., estimates of thyroid tissue remnant) and preablation TSH levels are common in clinical real life as well as the use of different Tg and TgAb assays in different centers. Overall, these factors represent a major limitation in selecting general thresholds and decision limits to inform postoperative clinical actions. Interestingly, however, neither RAIU values nor TSH levels were independently retained in our model and the impact of different Tg assays was negligible in our analysis. Accordingly, our Tg nodal thresholds were proved to be actionable even in different local populations that represent a relevant result of our study. Some limitations of our study must be mentioned. First, a potential drawback of our study is the lack of an external dataset for model validation. Rather, we performed an internal cross-validation procedure. On the other hand, this method reduces the risk of overfitting and provides a more robust estimate of model’s performance since all data are used for both training and validation. In addition, most analyzed parameters significantly varied between different centers supporting the use of an internal cross-validation instead of an external one. All in all, a more homogeneous population was obtained reflecting the real-life distribution of the parameters. Second, different Tg assays were employed in different centers and the PPV was lower in one center where a Tg assay was used which produces higher results compared to other assays [23]. However, the overall performance of the model remained good when retested in each subgroup. This is likely related to the good alignment of Tg assays employed in other participating centers. Additionally, Tg concentrations in our patients were significantly higher than those usually measured during the long term follow-up of cured DTC patients (i.e., 0.1–1 ng/mL), making the clinical impact of such analytical differences less relevant. Anyway, a careful evaluation of local Tg assay is advised, before adopting our decisional model in clinical practice [3, 4, 16, 23]. Third, our model included only patients treated after THW as most patients were treated with this preparation protocol in our centers. A significant positive correlation exists between Tg values measured under thyroxine, after rhTSH stimulation and after THW, respectively, with a basal/rhTSH-Tg and THW-Tg ratios of 1:5 and 1:10, respectively. Notwithstanding, our results cannot be directly translated to patients under thyroxine or those stimulated by rhTSH and further specific studies are warranted [16, 25, 26]. Finally, our model is explicitly intended as a tool to inform curative 131I administration in patients with high probability of persistent structural disease, independently by the initial risk stratification [27]. Notably, adjuvant therapy with 131I could still decrease the recurrence risk even in intermediate-risk patients with unstimulated Tg ≤ 1 ng/mL or stimulated Tg ≤ 10 ng/mL [28] making our system not actionable to rule out adjuvant 131I administration in low- and intermediate-risk DTC, respectively.
Conclusions
In conclusion, we developed a simple, accurate and reproducible decision tree model able to provide reliable information on the probability of persistent/metastatic DTC after surgery. The information provided by our model is highly relevant to refine the initial risk stratification and guide 131I administration with adjuvant or therapeutic basing on the probability of persistent and/or metastatic disease.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1–133.
Tuttle RM, Ahuja S, Avram AM, Bernet VJ, Bourguet P, Daniels GH, et al. Controversies, consensus, and collaboration in the use of 131I therapy in differentiated thyroid cancer: a joint statement from the American Thyroid Association, the European Association of Nuclear Medicine, the Society of Nuclear Medicine and Molecular Imaging, and the European Thyroid Association. Thyroid. 2019;29:461–70.
Giovanella L. Circulating biomarkers for the detection of tumor recurrence in the postsurgical follow-up of differentiated thyroid carcinoma. Curr Opin Oncol. 2020;32:7–12.
Knappe L, Giovanella L. Life after thyroid cancer: the role of thyroglobulin and thyroglobulin antibodies for postoperative follow-up. Exp Rev Endocrinol Metab. 2022. https://doi.org/10.1080/17446651.2021.1993060.
Webb RC, Howard RS, Stojadinovic A, Gaitonde DY, Wallace MK, Ahmed J, et al. The utility of serum thyroglobulin measurement at the time of remnant ablation for predicting disease-free status in patients with differentiated thyroid cancer: a meta-analysis involving 3947 patients. J Clin Endocrinol Metab. 2012;97:2754–63.
Vaisman A, Orlov S, Yip J, Hu C, Lim T, Dowar M, et al. Application of postsurgical stimulated thyroglobulin for radioiodine remnant ablation selection in low-risk papillary thyroid carcinoma. Head Neck. 2010;32:689–98.
Giovanella L, Ceriani L, Suriano S, Ghelfo A, Mffioli M. Thyroglobulin measurement before rhTSH-aided 131I ablation in detecting metastases from differentiated thyroid carcinoma. Clin Endocrinol. 2008;69:659–63.
Campennì A, Ruggeri RM, Siracusa M, Comis AD, Romano D, Vento A, et al. Early preablation rhTSH-stimulated thyroglobulin predicts outcome of differentiated thyroid cancer (DTC) patients. Eur J Nucl Med Molecular Imaging. 2021;48:2466–75.
Schneider DF, Ojomo KA, Chen H, Sippel RS. Remnant uptake as a postoperative oncologic quality indicator thyroid. Thyroid. 2013;23:1269–76.
Giovanella L. Thyroglobulin-guided (131)I ablation in low-risk differentiated thyroid carcinoma: is the yardstick accurate enough? Head Neck. 2011;33:1379–80.
Giovanella L, Cosma C, Plebani M. What is the role of serum thyroglobulin measurement in patients with differentiated thyroid cancer treated without radioactive iodine? J Clin Endocrinol Metab. 2017;102:2113–4.
Giovanella L, Ceriani L, Garo ML. Is thyroglobulin a reliable biomarker of differentiated thyroid cancer in patients treated by lobectomy? A systematic review and meta-analysis. Clin Chem Lab Med. 2022;60:1091–100.
Angell TE, Spencer CA, Rubino BD, Nicoloff JT, LoPresti JS. In search of an unstimulated thyroglobulin baseline value in low-risk papillary thyroid carcinoma patients not receiving radioactive iodine ablation. Thyroid. 2014;24:1127–33.
Görges R, Maniecki M, Jentzen W, N-Yi Sheu S, Mann K, Bockisch A, et al. Development and clinical impact of thyroglobulin antibodies in patients with differentiated thyroid carcinoma during the first 3 years after thyroidectomy. Eur J Endocrinol. 2005;153;49–55.
Grebe SK. Diagnosis and management of thyroid carcinoma: focus on serum thyroglobulin. Exp Rev Endocrinol Metab. 2009;4:25–43.
Giovanella L, Duntas LH. Management of endocrine disease: the role of rhTSH in the management of differentiated thyroid cancer: pros and cons. Eur J Endocrinol. 2019;181:133–45.
Giovanella L, Verburg FA. Ruling out 131I ablation in low-risk differentiated thyroid carcinoma basing on thyroglobulin measurement. Thyroid. 2011;21:809–10.
Avram AM, Giovanella L, Greenspan B, Lawson SA, Luster M, Van Nostrand D, et al. SNMMI procedure standard/EANM practice guideline for nuclear medicine evaluation and therapy of differentiated thyroid cancer: abbreviated version. J Nucl Med. 2022;63:15N-35N.
Freudenberg LS, Jentzen W, Petrich T, Frömke C, Marlowe RJ, Heusner T, et al. Lesion dose in differentiated thyroid carcinoma metastases after rhTSH or thyroid hormone withdrawal: 124I PET/CT dosimetric comparisons. Eur J Nucl Med Mol Imaging. 2010;37:2267–76.
Avram AM, Rosculet N, Esfandiari NH, Gauger PG, Miller BS, Cohen M, et al. Differentiated thyroid cancer outcomes after surgery and activity-adjusted 131I theragnostics. Clin Nucl Med. 2019;44:11–20.
Luster M, Clarke SE, Dietlein M, Lassmann M, Lind P, Oyen WJG, et al. Guidelines for radioiodine therapy of differentiated thyroid cancer. Eur J Nucl Med Mol Imaging. 2008;35:1941–59.
Giovanella L, Avram AM, Iakovou I, Kwak J, Lawson SA, Elizabeth Lulaj E, et al. EANM practice guideline/SNMMI procedure standard for RAIU and thyroid scintigraphy. Eur J Nucl Med Mol Imaging. 2019;46:2514–25.
Broecker-Preuss M, Mehnert I, Gilman E, Herrmann K, Weber M, Görges R. Evaluation of a new automated assay for high-sensitivity thyroglobulin measurement and comparison with two established high-sensitivity thyroglobulin assays. Pract Lab Med. 2921; 21: e00250.
Gulec SA, Ahuja S, Avram AM, Bernet VJ, Bourguet P, Draganescu C, et al. A joint statement from the American Thyroid Association, the European Association of Nuclear Medicine, the European Thyroid Association, the Society of Nuclear Medicine and Molecular Imaging on Current Diagnostic and Theranostic Approaches in the Management of Thyroid Cancer. Thyroid. 2021;31:1009–19.
Giovanella L, Ceriani L, Ghelfo A, Maffioli M, Keller F, Spriano G. Thyroglobulin assay during thyroxine treatment in low-risk differentiated thyroid cancer management: comparison with recombinant thyrotropin stimulated assay and imaging procedures. Clin Chem Lab Med. 2006;44:648–52.
Kowalska A, Pałyga I, Gąsior-Perczak D, Walczyk A, Trybek T, Słuszniak A, Mezyk R, Gozdz S. The cut-off level of recombinant human TSH-stimulated thyroglobulin in the follow-up of patients with differentiated thyroid cancer. PLoS ONE. 2015;10: e0133852.
Gao H, Huang J, Dai Q, Su J. Radioiodine (131I) treatment decision-making for low- and intermediate-risk differentiated thyroid cancer. Arch Endocrinol Metab. 2023;67/2. https://doi.org/10.20945/2359-3997000000538.
Tian T, Qi Y, Huang S, Wang H, Huang R. Radioactive iodine therapy decreases the recurrence of intermediate-risk PTC with low thyroglobulin levels. J Clin Endocrinol Metab. 2023; dgad045. https://doi.org/10.1210/clinem/dgad045.
Author information
Authors and Affiliations
Contributions
The study was conceived and designed by Luca Giovanella. Material preparation and data collection were performed by all authors. Data analysis was performed by Lisa Milan and Luca Ceriani. The first draft of the manuscript was written by Luca Giovanella and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This is an observational study. The Joint Research Ethics Committee of the Faculty of Medicine, University of Münster and the loco-regional Chamber of Physicians of Westfalen-Lippe, Germany, has confirmed that no ethical approval is required and informed consent was waived.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Theragnostic
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Giovanella, L., Milan, L., Roll, W. et al. Postoperative thyroglobulin as a yard-stick for radioiodine therapy: decision tree analysis in a European multicenter series of 1317 patients with differentiated thyroid cancer. Eur J Nucl Med Mol Imaging 50, 2767–2774 (2023). https://doi.org/10.1007/s00259-023-06239-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06239-8