Abstract
Background
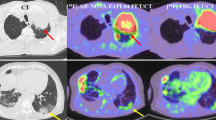
Fibrosis and inflammation are major pathological changes of Crohn’s disease (CD). Early detection and accurate severity evaluation of CD are critical for patient’s prognosis. Endoscopy is widely used to evaluate CD progression. Herein, we evaluated the efficacy of [68Ga]Ga-FAPI-04 PET/CT to identify lesions and assess the progression of CD.
Methods
All CD patients received computed tomography enterography (CTE), [68Ga]Ga-FAPI-04 PET/CT examination, and ileocolonoscopy within 1 week. Two independent gastroenterologists computed the Crohn’s disease activity index (CDAI) of all patients. Two radiology physicians assessed the CTE images separately, and the CTE scores were calculated. Lastly, two nuclear medicine physicians independently examined the [68Ga]Ga-FAPI-04 PET/CT images. Once the FAPI uptake of the intestinal segment was equal or higher relative to the liver (considered FAPI-positive), the target-to-background ratio (TBR) and global FAPI PET/CT score were computed, representing the independent intestinal activity and activity of all intestinal segments, respectively. Levels of fecal calprotectin (FCP) and C-reactive protein (CRP) were determined before the endoscopy. The Crohn’s disease endoscopy index of severity (CDEIS) and the simple endoscopic score for Crohn’s disease (SES-CD) were calculated during the endoscopy. Finally, all data were obtained and analyzed.
Results
There were 74 intestinal segments in 16 patients were assessed. [68Ga]Ga-FAPI-04 PET/CT identified 42 of 45 endoscopically lesioned segments (endoscopic lesions detection sensitivity: 93.3%), while CTE identified 39 of them (endoscopic lesions detection sensitivity: 86.7%). According to the receiver operating characteristic (ROC) analysis, [68Ga]Ga-FAPI-04 PET/CT showed better performance in the detection of endoscopic lesions compared with CTE (P < 0.05). The TBR was significantly associated with the CTE score (r = 0.81; (95% CI): 0.736–0.869; P < 0.0001) and SES-CD values (r = 0.86; (95% CI): 0.776–0.908; P < 0.0001). In addition, the global FAPI PET/CT score was significantly correlated with FCP (r = 0.52; 95% CI, 0.02–0.81; P = 0.039), CRP (r = 0.60; 95% CI, 0.13–0.85; P = 0.014), CDEIS (r = 0.55; 95% CI, 0.06–0.83; P = 0.028), and CDAI (r = 0.81; 95% CI, 0.50–0.93; P < 0.0001).
Conclusion
In summary, [68Ga]Ga-FAPI-04 PET/CT correlated well with endoscopic, CTE, clinical, and biomarkers of CD. It was also highly sensitive in the detection of different classes of lesions in all intestinal segments, and unlike other examinations, this technique required no patient fasting or bowel preparation. Therefore, [68Ga]Ga-FAPI-04 PET/CT may be a promising method for assessing the activity of CD.






Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Crohn BB, Ginzburg L, Oppenheimer GD. Landmark article Oct 15, 1932. Regional ileitis. A pathological and clinical entity. By Burril B. Crohn, Leon Ginzburg, and Gordon D. Oppenheimer. Jama. 1984;251:73–9. https://doi.org/10.1001/jama.251.1.73.
Rosen MJ, Dhawan A, Saeed SA. Inflammatory bowel disease in children and adolescents. JAMA Pediatr. 2015;169:1053–60. https://doi.org/10.1001/jamapediatrics.2015.1982.
Bousvaros A, Antonioli DA, Colletti RB, Dubinsky MC, Glickman JN, Gold BD, et al. Differentiating ulcerative colitis from Crohn disease in children and young adults: report of a working group of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the Crohn’s and Colitis Foundation of America. J Pediatr Gastroenterol Nutr. 2007;44:653–74. https://doi.org/10.1097/MPG.0b013e31805563f3.
D’Alessio S, Ungaro F, Noviello D, Lovisa S, Peyrin-Biroulet L, Danese S. Revisiting fibrosis in inflammatory bowel disease: the gut thickens. Nat Rev Gastroenterol Hepatol. 2022;19:169–84. https://doi.org/10.1038/s41575-021-00543-0.
Cosnes J, Cattan S, Blain A, Beaugerie L, Carbonnel F, Parc R, et al. Long-term evolution of disease behavior of Crohn’s disease. Inflamm Bowel Dis. 2002;8:244–50. https://doi.org/10.1097/00054725-200207000-00002.
Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn’s disease. Lancet. 2017;389:1741–55. https://doi.org/10.1016/s0140-6736(16)31711-1.
Li C, Kuemmerle JF. Mechanisms that mediate the development of fibrosis in patients with Crohn’s disease. Inflamm Bowel Dis. 2014;20:1250–8. https://doi.org/10.1097/mib.0000000000000043.
Nijhuis A, Biancheri P, Lewis A, Bishop CL, Giuffrida P, Chan C, et al. In Crohn's disease fibrosis-reduced expression of the miR-29 family enhances collagen expression in intestinal fibroblasts. Clinical science (London, England : 1979). 2014;127:341–50. https://doi.org/10.1042/cs20140048.
Acharya PS, Zukas A, Chandan V, Katzenstein AL, Puré E. Fibroblast activation protein: a serine protease expressed at the remodeling interface in idiopathic pulmonary fibrosis. Hum Pathol. 2006;37:352–60. https://doi.org/10.1016/j.humpath.2005.11.020.
Luo Y, Pan Q, Zhang W, Li F. Intense FAPI uptake in inflammation may mask the tumor activity of pancreatic cancer in 68Ga-FAPI PET/CT. Clin Nucl Med. 2020;45:310–1. https://doi.org/10.1097/rlu.0000000000002914.
Tang W, Wu J, Yang S, Wang Q, Chen Y. Organizing pneumonia with intense 68Ga-FAPI uptake mimicking lung cancer on 68Ga-FAPI PET/CT. Clin Nucl Med. 2022;47:223–5. https://doi.org/10.1097/RLU.0000000000003855.
Annese V, Daperno M, Rutter MD, Amiot A, Bossuyt P, East J, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013;7:982–1018. https://doi.org/10.1016/j.crohns.2013.09.016.
Arai T, Takeuchi K, Miyamura M, Ishikawa R, Yamada A, Katsumata M, et al. Level of fecal calprotectin correlates with severity of small bowel Crohn’s disease, measured by balloon-assisted enteroscopy and computed tomography enterography. Clin Gastroenterol Hepatol. 2017;15:56–62. https://doi.org/10.1016/j.cgh.2016.08.015.
Lee SS, Ha HK, Yang SK, Kim AY, Kim TK, Kim PN, et al. CT of prominent pericolic or perienteric vasculature in patients with Crohn’s disease: correlation with clinical disease activity and findings on barium studies. AJR Am J Roentgenol. 2002;179:1029–36. https://doi.org/10.2214/ajr.179.4.1791029.
Park EK, Han NY, Park BJ, Sung DJ, Cho SB, Jeen YT, et al. Value of computerized tomography enterography in predicting Crohn’s disease activity: correlation with Crohn’s disease activity index and c-reactive protein. Iran J Radiol. 2016;13:e34301. https://doi.org/10.5812/iranjradiol.34301.
Zhou Y, Yang X, Liu H, Luo W, Liu H, Lv T, et al. Value of [(68)Ga]Ga-FAPI-04 imaging in the diagnosis of renal fibrosis. Eur J Nucl Med Mol Imaging. 2021;48:3493–501. https://doi.org/10.1007/s00259-021-05343-x.
Wang S, Zhou X, Xu X, Ding J, Liu T, Jiang J, et al. Dynamic PET/CT imaging of (68)Ga-FAPI-04 in Chinese subjects. Front Oncol. 2021;11:651005. https://doi.org/10.3389/fonc.2021.651005.
Louis E, Ancion G, Colard A, Spote V, Belaiche J, Hustinx R. Noninvasive assessment of Crohn’s disease intestinal lesions with (18)F-FDG PET/CT. J Nucl Med. 2007;48:1053–9. https://doi.org/10.2967/jnumed.107.040436.
Yiğit B, Sezgin O, Yorulmaz E, Ertürk M, Erdem U, Yanç U, et al. Effectiveness and power of abdominal ultrasonography in the assessment of Crohn’s disease activity: comparison with clinical, endoscopic, and CT enterography findings. The Turkish journal of gastroenterology : the official journal of Turkish Society of Gastroenterology. 2022;33:294–303. https://doi.org/10.5152/tjg.2022.201157.
Napolitano M, Munari AM, Di Leo G, Panarisi NAR, Zuin G, Fava G, et al. MR enterography grading of pediatric ileocolonic Crohn disease activity based on a single bowel segment. Radiol Med (Torino). 2021;126:1396–406. https://doi.org/10.1007/s11547-021-01409-w.
Lopes S, Andrade P, Afonso J, Cunha R, Rodrigues-Pinto E, Ramos I, et al. Monitoring Crohn’s disease activity: endoscopy, fecal markers and computed tomography enterography. Ther Adv Gastroenterol. 2018;11:1756284818769075. https://doi.org/10.1177/1756284818769075.
Benitez JM, Meuwis MA, Reenaers C, Van Kemseke C, Meunier P, Louis E. Role of endoscopy, cross-sectional imaging and biomarkers in Crohn’s disease monitoring. Gut. 2013;62:1806–16. https://doi.org/10.1136/gutjnl-2012-303957.
Li Y, Langhorst J, Koch AK, Demircioglu A, Schaarschmidt B, Theysohn JM, et al. Comparison of acceptance of PET/MR enterography and ileocolonoscopy in patients with inflammatory bowel diseases. Clin Imaging. 2020;64:11–7. https://doi.org/10.1016/j.clinimag.2020.03.001.
Mary J, Lemann M, Colombel F. Endoscopic remission and response in Crohn’s disease: an objective definition using the CDEIS. Gut. 2006;37.
Gale HI, Sharatz SM, Taphey M, Bradley WF, Nimkin K, Gee MS. Comparison of CT enterography and MR enterography imaging features of active Crohn disease in children and adolescents. Pediatr Radiol. 2017;47:1321–8. https://doi.org/10.1007/s00247-017-3876-z.
Ma L, Shen X, Chen YJ, Zhang Q, Li B, Zhang W. Computed tomography enterography for Crohn’s disease: correlation between the imaging findings and histopathologic scoring system. Abdom Radiol (NY). 2021;46:4121–9. https://doi.org/10.1007/s00261-021-03112-w.
Cheng J, Xie H, Yang H, Wang K, Xu G, Wu G. Computed tomography enterography: quantitative evaluation on Crohn’s disease activity. Gastroenterol Res Pract. 2018;2018:7351936. https://doi.org/10.1155/2018/7351936.
Tong JL, Feng Q, Shen J, Qiao YQ, Zheng Q, Gu Y, et al. Computed tomography enterography versus balloon-assisted enteroscopy for evaluation of small bowel lesions in Crohn’s disease. J Gastroenterol Hepatol. 2013;28:1180–6. https://doi.org/10.1111/jgh.12231.
Roda G, Chien Ng S, Kotze PG, Argollo M, Panaccione R, Spinelli A, et al. Crohn’s disease Nat Rev Dis Primers. 2020;6:22. https://doi.org/10.1038/s41572-020-0156-2.
Naganuma M, Hisamatsu T, Matsuoka K, Kiyohara H, Arai M, Sugimoto S, et al. Endoscopic severity predicts long-term prognosis in Crohn’s disease patients with clinical remission. Digestion. 2016;93:66–71. https://doi.org/10.1159/000441767.
Higgins PD, Fletcher JG. Characterization of inflammation and fibrosis in Crohn’s disease lesions by magnetic resonance imaging. Am J Gastroenterol. 2015;110:441–3. https://doi.org/10.1038/ajg.2015.26.
Zidar N, Langner C, Jerala M, Bostjancic E, Drobne D, Tomazic A. Pathology of fibrosis in Crohn’s disease-contribution to understanding its pathogenesis. Front Med (Lausanne). 2020;7:167. https://doi.org/10.3389/fmed.2020.00167.
Lay AJ, Zhang HE, McCaughan GW, Gorrell MD. Fibroblast activation protein in liver fibrosis. Frontiers in bioscience (Landmark edition). 2019;24:1–17. https://doi.org/10.2741/4706.
Golovics PA, Mandel MD, Lovasz BD, Lakatos PL. Inflammatory bowel disease course in Crohn’s disease: is the natural history changing? World J Gastroenterol. 2014;20:3198–207. https://doi.org/10.3748/wjg.v20.i12.3198.
Kuwert T, Schmidkonz C, Prante O, Schett G, Ramming A. FAPI PET opens a new window to understanding immune-mediated inflammatory diseases. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2022;63:1136–7. https://doi.org/10.2967/jnumed.122.263922.
Rieder F, Zimmermann EM, Remzi FH, Sandborn WJ. Crohn’s disease complicated by strictures: a systematic review. Gut. 2013;62:1072–84. https://doi.org/10.1136/gutjnl-2012-304353.
Schmidkonz C, Rauber S, Atzinger A, Agarwal R, Götz TI, Soare A, et al. Disentangling inflammatory from fibrotic disease activity by fibroblast activation protein imaging. Ann Rheum Dis. 2020;79:1485–91. https://doi.org/10.1136/annrheumdis-2020-217408.
Shyn PB. 18F-FDG positron emission tomography: potential utility in the assessment of Crohn’s disease. Abdom Imaging. 2012;37:377–86. https://doi.org/10.1007/s00261-011-9793-y.
Lovinfosse P, Hustinx R. The role of PET imaging in inflammatory bowel diseases: state-of-the-art review. The quarterly journal of nuclear medicine and molecular imaging : official publication of the Italian Association of Nuclear Medicine (AIMN) [and] the International Association of Radiopharmacology (IAR), [and] Section of the So. 2022;66:206–17. https://doi.org/10.23736/s1824-4785.22.03467-7.
Giesel FL, Kratochwil C, Lindner T, Marschalek MM, Loktev A, Lehnert W, et al. (68)Ga-FAPI PET/CT: biodistribution and preliminary dosimetry estimate of 2 DOTA-containing FAP-targeting agents in patients with various cancers. J Nucl Med. 2019;60:386–92. https://doi.org/10.2967/jnumed.118.215913.
Thomas H. IBD: Inflammatory biomarkers improve management of Crohn’s disease. Nat Rev Gastroenterol Hepatol. 2018;15:4–5. https://doi.org/10.1038/nrgastro.2017.164.
Meuwis MA, Vernier-Massouille G, Grimaud JC, Bouhnik Y, Laharie D, Piver E, et al. Serum calprotectin as a biomarker for Crohn’s disease. J Crohns Colitis. 2013;7:e678–83. https://doi.org/10.1016/j.crohns.2013.06.008.
Funding
The Luzhou Science and Technology Bureau (Grant No. 2021LZXNYD-J09) and the National Outstanding Youth Science Fund Project of the National Natural Science Foundation of China (Grant No. 82100632) provided financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study procedures were approved by the collaborating institution and carefully followed the guidelines of the 1964 Helsinki Declaration. This study did not include any animal trials.
Consent to participate
Before being included in the study, each participant was required to sign an informed consent form.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Infection and inflammation.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, L., Zhong, X., Li, L. et al. [68Ga]Ga-FAPI-04 PET/CT on assessing Crohn’s disease intestinal lesions. Eur J Nucl Med Mol Imaging 50, 1360–1370 (2023). https://doi.org/10.1007/s00259-023-06107-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06107-5