Abstract
Purpose
[18F]AlF-RESCA was introduced as a core particularly useful for 18F-labeling of heat-sensitive biomolecules. However, no translational studies have been reported up to now. Herein, we reported the first-in-human evaluation of an 18F-labeled anti-HER2 nanobody MIRC213 as a PET radiotracer for imaging HER2-positive cancers.
Methods
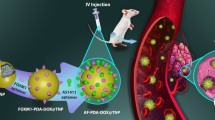
MIRC213 was produced by E. coli and conjugated with ( ±)-H3RESCA-Mal. [18F]AlF-RESCA-MIRC213 was prepared at room temperature. Its radiochemical purity and stability of were determined by radio-HPLC with the size-exclusion chromatographic column. Cell uptake was performed in NCI-N87 (HER2 +) and MCF-7 (HER2-) cells and the cell-binding affinity was verified in SK-OV-3 (HER2 +) cells. Small-animal PET/CT was performed using SK-OV-3, NCI-N87, and MCF-7 tumor-bearing mice at 30 min, 1 h, and 2 h post-injection. For blocking experiment, excess MIRC213 was co-injected with radiotracer. Biodistribution were performed on SKOV-3 and MCF-7 tumor-bearing mice at 2 h post-injection. For clinical study, PET/CT images were acquired at 2 h and 4 h after injection of [18F]AlF-RESCA-MIRC213 (1.85–3.7 MBq/kg) in six breast cancer patients (3 HER2-positive and 3 HER2-negative). All patients underwent [18F]-FDG PET/CT within a week for tissue selection purpose. Distribution and dosimetry were calculated. Standardized uptake values (SUV) were measured in tumors and normal organs.
Results
MIRC213 was produced with > 95% purity and modified with RESCA to obtain RESCA-MIRC213. [18F]AlF-RESCA-MIRC213 was prepared within 20 min at room temperature with the radiochemical yield of 50.48 ± 7.6% and radiochemical purity of > 98% (n > 10), and remained stable in both PBS (88%) and 5% HSA (92%) after 6 h. The 2 h cellular uptake of [18F]AlF-RESCA-MIRC213 in NCI-N87 cells was 11.22 ± 0.60 AD%/105 cells. Its binding affinity Kd value was determined to be 1.23 ± 0.58 nM. Small-animal PET/CT with [18F]AlF-RESCA-MIRC213 can clearly differentiate SK-OV-3 and NCI-N87 tumors from MCF-7 tumors and background with a high uptake of 4.73 ± 1.18 ID%/g and substantially reduced to 1.70 ± 0.13 ID%/g for the blocking group (p < 0.05) in SK-OV-3 tumors at 2 h post-injection. No significant bone radioactivity was seen in the tumor-bearing animals. In all six breast cancer patients, there was no adverse reaction during study. The uptake of [18F]AlF-RESCA-MIRC213 was mainly in lacrimal gland, parotid gland, submandibular gland, thyroid gland, gallbladder, kidneys, liver, and intestines. There was no significant bone radioactivity accumulation in cancer patients. [18F]AlF-RESCA-MIRC213 had significantly higher tumor uptake in lesions from HER2-positive patients than that lesions from HER2-negative patients (SUVmax of 3.62 ± 1.56 vs. 1.41 ± 0.41, p = 0.0012) at 2 h post-injection. The kidneys received the highest radiation dose of 2.42 × 10−1 mGy/MBq, and the effective dose was 1.56 × 10−2 mSv/MBq.
Conclusions
[18F]AlF-RESCA-MIRC213 could be prepared with high radiolabeling yield under mild conditions. [18F]AlF-RESCA-MIRC213 has relatively high stability both in vitro and in vivo. The results from clinical transformation suggest that [18F]AlF-RESCA-MIRC213 PET/CT is a safe procedure with favorable pharmacokinetics and dosimetry profile, and it is a promising new PET radiotracer for noninvasive diagnosis of HER2-positive cancers.






Similar content being viewed by others
Abbreviations
- HER2:
-
Human epidermal receptor type 2
- IHC:
-
Immunohistochemical staining
- FISH:
-
Fluorescence in situ hybridization
- SUV:
-
Standardized uptake values
- PET:
-
Positron emission tomography
- RT:
-
Room temperature
- FBS:
-
Fetal bovine serum
- HSA:
-
Human serum albumins
- PBS:
-
Phosphate-buffered saline buffer
- RCP:
-
Radiochemical purity
- BFC:
-
Bifunctional chelators
References
Cai Y, Wang J, Zhang L, et al. Expressions of fatty acid synthase and HER2 are correlated with poor prognosis of ovarian cancer. Med Oncol. 2015;32(1):391.
Schluter B, Gerhards R, Strumberg D, et al. Combined detection of HER2/neu gene amplification and protein overexpression in effusions from patients with breast and ovarian cancer. J Cancer Res Clin Oncol. 2010;136(9):1389–400.
Ménard S, Casalini P, Campiglio M, et al. HER2 overexpression in various tumor types, focusing on its relationship to the development of invasive breast cancer. Ann Oncol. 2001;12:S15–9.
Scholl S, Beuzeboc P, Pouillart P. Targeting HER2 in other tumor types. Ann Oncol. 2001;12:S81–7.
Buonaguro FM, Lewis GK, Pelicci P. Introducing infectious agents and cancer. Infect Agent Cancer. 2006;1(1):1.
Hede K. Gastric cancer: trastuzumab trial results spur search for other targets. J Natl Cancer Inst. 2009;101(19):1306–7.
Minot DM, Voss J, Rademacher S, et al. Image analysis of HER2 immunohistochemical staining. Reproducibility and concordance with fluorescence in situ hybridization of a laboratory-validated scoring technique. Am J Clin Pathol. 2012;137(2):270–6.
Zidan J, Dashkovsky I, Stayerman C, et al. Comparison of HER2 overexpression in primary breast cancer and metastatic sites and its effect on biological targeting therapy of metastatic disease. Br J Cancer. 2005;93(5):552–6.
Fabi A, Di Benedetto A, Metro G, et al. HER2 protein and gene variation between primary and metastatic breast cancer: significance and impact on patient care. J Clin Cancer Res. 2011;17(7):2055–64.
Sapino A, Goia M, Recupero D, et al. Current challenges for HER2 testing in diagnostic pathology: state of the art and controversial issues. Front Oncol. 2013;3:129.
Cardoso F, Costa A, Norton L, et al. ESO-ESMO 2nd international consensus guidelines for advanced breast cancer (ABC2). Breast. 2014;23(5):489–92.
Hicks DG, Kulkarni S. HER2+ breast cancer: review of biologic relevance and optimal use of diagnostic tools. Am J Clin Pathol. 2008;129(2):263–73.
Tolmachev V. Imaging of HER2 overexpression in tumors for guiding therapy. Curr Pharm Des. 2008;14(28):2999–3019.
Gambhir SS. Molecular imaging of cancer with positron emission tomography. Nat Rev Cancer. 2002;2(9):683–93.
Lebars D. Fluorine-18 and medical imaging: radiopharmaceuticals for positron emission tomography. J Fluorine Chem. 2006;127(11):1488–93.
Sanchez-Crespo A. Comparison of gallium-68 and fluorine-18 imaging characteristics in positron emission tomography. Appl Radia Isot. 2013;76:55–62.
McBride WJ, D’Souza CA, Sharkey RM, et al. The radiolabeling of proteins by the [18F]AlF method. Appl Radiat Isot. 2012;70(1):200–4.
McBride WJ, Sharkey RM, Karacay H, et al. A novel method of 18F radiolabeling for PET. J Nucl Med. 2009;50(6):99–108.
Wan W, Guo N, Pan D, et al. First experience of 18F-alfatide in lung cancer patients using a new lyophilized kit for rapid radiofluorination. J Nucl Med. 2013;54(5):691–8.
Cleeren F, Lecina J, Billaud EM, et al. New chelators for low temperature Al18F-labeling of biomolecules. Bioconjugate Chem. 2016;27(3):790–8.
Cleeren F, Lecina J, Ahamed M, et al. Al18F-labeling of heat-sensitive biomolecules for positron emission tomography imaging. Theranostics. 2017;7:2924–39.
Gainkam LO, Keyaerts M, Caveliers V, et al. Correlation between epidermal growth factor receptor-specific nanobody uptake and tumor burden: a tool for noninvasive monitoring of tumor response to therapy. Mol Imaging Biol. 2011;13(5):940–8.
Vaneycken I, D’Huyvetter M, Hernot S, et al. Immuno-imaging using nanobodies. Curr Opin Biotechnol. 2011;22(6):877–81.
Hu B, Liu T, Li L, et al. IgG-Binding nanobody capable of prolonging nanobody-based radiotracer plasma half-life and enhancing the efficacy of tumor-targeted radionuclide therapy. Bioconjug Chem. 2022;33(7):1328–39.
Li L, Liu T, Shi L, et al. HER2-targeted dual radiotracer approach with clinical potential for noninvasive imaging of trastuzumab-resistance caused by epitope masking. Theranostics. 2022;12(12):5551–63.
Speer TW. Dissociation constant (Kd). In: Brady LW, Yaeger TE, editors. Encyclopedia of Radiation Oncology. Springer, Berlin: Heidelberg; 2013. p. 157–8.
Wolff AC, Hammond MEH, Allison KH, et al. Human epidermal growth factor receptor 2 testing in Breast Cancer: American society of clinical oncology/college of American pathologists clinical practice guideline focused update. J Clin Oncol. 2018;36(20):2105–22.
Chen Q, Ma Q, Chen M, et al. An exploratory study on 99mTc-RGD-BBN peptide scint-imammography in the assessment of breast malignant lesions compared to 99mTc3P4-RGD2. PLoS One. 2015;10(4):e0123401.
van der Veen EL, Suurs FV, Cleeren F, et al. Development and evaluation of Interleukin-2-derived radiotracers for PET imaging of T cells in mice. J Nucl Med. 2020;61(9):1355–60.
Liu T, Liu C, Xu X, et al. Preclinical evaluation and pilot clinical study of Al18F-PSMA-BCH for prostate cancer PET imaging. J Nucl Med. 2019;60(9):1284–92.
Xie Q, Liu T, Ding J, et al. Synthesis, preclinical evaluation, and a pilot clinical imaging study of [18F]AlF-NOTA-JR11 for neuroendocrine neoplasms compared with [68Ga]Ga-DOTA-TATE. Eur J Nucl Med Mol Imaging. 2021;48(10):3129–40.
Chakravarty R, Goel S, Cai W. Nanobody: the “magic bullet” for molecular imaging. Theranostics. 2014;4(4):386–98.
Pruszynski M, Koumarianou E, Vaidyanathan G, et al. Improved tumor targeting of anti-HER2 nanobody through N-succinimidyl 4-guanidinomethyl-3-iodobenzoate radiolabeling. J Nucl Med. 2014;55(4):650–6.
Vaneycken I, Devoogdt N, Van Gassen N, et al. Preclinical screening of anti-HER2 nanobodies for molecular imaging of breast cancer. FASEB J. 2011;25(7):2433–46.
D’Huyvetter M, Aerts A, Xavier C, et al. Development of 177Lu-nanobodies for radioimmunotherapy of HER2-positive breast cancer: evaluation of different bifunctional chelators. Contrast Media Mol Imaging. 2012;7(2):254–64.
Xavier C, Vaneycken I, D'huyvetter M, et al. Synthesis, preclinical validation, dosimetry, and toxicity of 68Ga-NOTA-anti-HER2 nanobodies for iPET imaging of HER2 receptor expression in cancer. J Nucl Med. 2013;54(5):776–84.
D’Huyvetter M, Vincke C, Xavier C, et al. Targeted radionuclide therapy with A 177Lu-labeled anti-HER2 nanobody. Theranostics. 2014;4(7):708–20.
Keyaerts M, Xavier C, Heemskerk J, et al. Phase I study of 68Ga-HER2-nanobody for PET/CT assessment of HER2 expression in breast carcinoma. J Nucl Med. 2016;57(1):27–33.
Xavier C, Blykers A, Vaneycken I, et al. 18F-nanobody for PET imaging of HER2 overexpressing tumors. Nucl Med Biol. 2016;43(4):247–52.
D’Huyvetter M, De Vos J, Xavier C, et al. 131I-labeled Anti-HER2 Camelid sdAb as a theranostic tool in cancer treatment. Clin Cancer Res. 2017;23(21):6616–28.
Dekempeneer Y, Bäck T, Aneheim E, et al. Labeling of anti-HER2 nanobodies with astatine-211: optimization and the effect of different coupling reagents on their in vivo behavior. Mol Pharmaceutics. 2019;16(8):3524–33.
Ge S, Li J, Yu Y, et al. Review: radionuclide molecular imaging targeting HER2 in breast cancer with a focus on molecular probes into clinical trials and small peptides. Molecules. 2021;26(21):6482.
Altunay B, Morgenroth A, Beheshti M, et al. HER2-directed antibodies, affibodies and nanobodies as drug-delivery vehicles in breast cancer with a specific focus on radioimmunotherapy and radioimmunoimaging. Eur J Nucl Med Mol Imaging. 2021;48(5):1371–89.
Xing Y, Chand G, Liu C, et al. Early phase I study of a 99mTc-labeled anti–programmed death ligand-1 (PD-L1) single-domain antibody in SPECT/CT assessment of PD-L1 expression in non–small cell lung cancer. J Nucl Med. 2019;60(9):1213–20.
D’Huyvetter M, Vos JD, Caveliers V, et al. Phase I trial of 131I-GMIB-Anti-HER2-VHH1, a new promising candidate for HER2-targeted radionuclide therapy in breast cancer patients. J Nucl Med. 2021;62:1097–105.
Vaidyanathan G, McDougald D, Choi J, et al. Preclinical evaluation of 18F-labeled anti-HER2 nanobody conjugates for imaging HER2 ceceptor expression by immuno-PET. J Nucl Med. 2016;57(6):967–73.
Gainkam LO, Caveliers V, Devoogdt N, et al. Localization, mechanism and reduction of renal retention of technetium-99m labeled epidermal growth factor receptor-specific nanobody in mice. Contrast Media Mol Imaging. 2011;6(2):85–92.
McBride WJ, Sharkey RM, Goldenberg DM. Radiofluorination using aluminum-fluoride (Al18F). EJNMMI Res. 2013;3(1):36.
Sandström M, Velikyan I, Garske-Roman U, et al. Comparative biodistribution and radiation dosimetry of 68Ga-DOTATOC and 68Ga-DOTATATE in patients with neuroendocrine tumors. J Nucl Med. 2013;54(10):1755–9.
Afshar-Oromieh A, Malcher A, Eder M, et al. Reply to Reske. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40(6):971–2.
Sörensen J, Sandberg D, Sandstrom M, et al. First-in-human molecular imaging of HER2 expression in breast cancer metastases using the 111In-ABY-025 affibody molecule. J Nucl Med. 2014;55(5):730–5.
Chomet M, van Dongen GAMS, Vugts DJ. State of the art in radiolabeling of antibodies with common and uncommon radiometals for preclinical and clinical immuno-PET. Bioconjug Chem. 2021;32(7):1315–30.
Cohen JA, Weiner DB, More KF, et al. Expression pattern of the neu (NGL) gene-encoded growth factor receptor protein (p185neu) in normal and transformed epithelial tissues of the digestive tract. Oncogene. 1989;4(1):81–8.
Shetty D, Choi SY, Jeong JM, et al. Stable aluminium fluoride chelates with triazacyclononane derivatives proved by X-ray crystallography and 18F-labeling study. Chem Commun. 2011;47(34):9732–4.
Bridoux J, Neyt S, Debie P, et al. Improved detection of molecular markers of atherosclerotic plaques using sub-millimeter PET imaging. Molecules. 2020;25(8):1838.
Cleeren F, Lecina J, Bridoux J, et al. Direct fluorine-18 labeling of heat-sensitive biomolecules for positron emission tomography imaging using the Al18F-RESCA method. Nat Protoc. 2018;13(10):2330–47.
Funding
This research was supported by grants from the National Natural Science Foundation of China (NSFC) (projects 81871416, 82172006); Capital’s Funds for Health Improvement and Research (No.2022-2Z-2154 and 2022-2Z-2155); Beijing Hospitals Authority Deng feng Project (DFL20191102); The Pilot Project (4 th Round) to Reform Public Development of Beijing Municipal Medical Research Institute (2021–1); Beijing Municipal Administration of Hospitals-Yang fan Project (ZYLX201816), Science Foundation of Peking University Cancer Hospital (No.2021–4).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by Ethics Committee of Beijing Cancer Hospital and Institute (no. 2021KT108). Informed consent was obtained from all individual participants included in the study.
Informed consent
Informed consent was obtained from the 6 individual participants included in this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Translational research.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qin, X., Guo, X., Liu, T. et al. High in-vivo stability in preclinical and first-in-human experiments with [18F]AlF-RESCA-MIRC213: a 18F-labeled nanobody as PET radiotracer for diagnosis of HER2-positive cancers. Eur J Nucl Med Mol Imaging 50, 302–313 (2023). https://doi.org/10.1007/s00259-022-05967-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-022-05967-7