Abstract
Purpose
The objective of this study was to evaluate the potential of PEGylated 64Cu-liposomes in clinical diagnostic positron emission tomography (PET) imaging and PEGylated 177Lu-liposomes in internal tumor radiotherapy through in vivo characterization and dosimetric analysis in a human xenograft mouse model.
Methods
Liposomes with 5 and 10 mol% PEG were characterized with respect to size, charge, and 64Cu- and 177Lu-loading efficiency. The tumor imaging potential of 64Cu-loaded liposomes was evaluated in terms of in vivo biodistribution, tumor accumulation and tumor-to-muscle (T/M) ratios, using PET imaging. The potential of PEGylated liposomes for diagnostic and therapeutic applications was further evaluated through dosimetry analysis using OLINDA/EXM software. The 64Cu-liposomes were used as biological surrogates to estimate the organ and tumor kinetics of 177Lu-liposomes.
Results
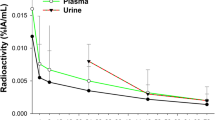
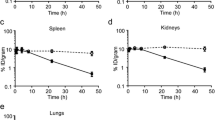
High remote loading efficiency (>95 %) was obtained for both 64Cu and 177Lu radionuclides with PEGylated liposomes, and essentially no leakage of the encapsulated radionuclide was observed upon storage and after serum incubation for 24 h at 37 °C. The 10 mol% PEG liposomes showed higher tumor accumulation (6.2 ± 0.2 %ID/g) than the 5 mol% PEG liposomes, as evaluated by PET imaging. The dosimetry analysis of the 64Cu-liposomes estimated an acceptable total effective dose of 3.3·10−2 mSv/MBq for diagnostic imaging in patients. A high absorbed tumor dose (114 mGy/MBq) was estimated for the potential radiotherapeutic 177Lu-liposomes.
Conclusion
The overall preclinical profile of PEGylated 64Cu-liposomes showed high potential as a new PET theranostic tracer for imaging in humans. Dosimetry results predicted that initial administered activity of 200 MBq of 64Cu-liposomes should be acceptable in patients. Work is in progress to validate the utility of PEGylated 64Cu-liposomes in a clinical research programme. The high absorbed tumor dose (114 mGy/MBq) estimated for 177Lu-liposomes and the preliminary dosimetric studies justify further therapeutic and dosimetry investigation of 177Lu-liposomes in animals before potential testing in man.





Similar content being viewed by others
References
Binderup T, Knigge U, Loft A, Federspiel B, Kjaer A. 18F-fluorodeoxyglucose positron emission tomography predicts survival of patients with neuroendocrine tumors. Clin Cancer Res. 2010;16:978–85.
Hellwig D, Gröschel A, Graeter TP, Hellwig AP, Nestle U, Schafers HJ, et al. Diagnostic performance and prognostic impact of FDG-PET in suspected recurrence of surgically treated non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2006;33:13–21.
Hutchings M, Loft A, Hansen M, Pedersen LM, Buhl T, Jurlander J, et al. FDG-PET after two cycles of chemotherapy predicts treatment failure and progression-free survival in Hodgkin lymphoma. Blood. 2006;107:52–9.
Hutchings M, Loft A, Hansen M, Berthelsen AK, Specht L. Clinical impact of FDG-PET/CT in the planning of radiotherapy for early-stage Hodgkin lymphoma. Eur J Haematol. 2007;78:206–12.
Torizuka T, Tanizaki Y, Kanno T, Futatsubashi M, Naitou K, Ueda Y, et al. Prognostic value of 18F-FDG PET in patients with head and neck squamous cell cancer. AJR Am J Roentgenol. 2009;192:W156–60.
Adams S, Baum R, Rink T, Schumm-Dräger PM, Usadel KH, Hör G. Limited value of fluorine-18 fluorodeoxyglucose positron emission tomography for the imaging of neuroendocrine tumours. Eur J Nucl Med. 1998;25:79–83.
Binderup T, Knigge U, Loft A, Mortensen J, Pfeifer A, Federspiel B, et al. Functional imaging of neuroendocrine tumors: a head-to-head comparison of somatostatin receptor scintigraphy, 123I-MIBG scintigraphy, and 18F-FDG PET. J Nucl Med. 2010;51:704–12.
Miele E, Spinelli GP, Tomao F, Zullo A, De Marinis F, Pasciuti G, et al. Positron emission tomography (PET) radiotracers in oncology – utility of 18F-Fluoro-deoxy-glucose (FDG)-PET in the management of patients with non-small-cell lung cancer (NSCLC). J Exp Clin Cancer Res. 2008;27:52–61.
Ravindra V, Botkin C, Yost P, Osman M. Incidental diagnosis of prostate cancer in FDG PET/CT: An initial experience. J Nucl Med. 2007;48:474P.
Schöder H, Larson SM. Positron emission tomography for prostate, bladder, and renal cancer. Semin Nucl Med. 2004;34:274–92.
Wadas TJ, Wong EH, Weisman GR, Anderson CJ. Coordinating radiometals of copper, gallium, indium, yttrium and zirconium for PET and SPECT imaging of disease. Chem Rev. 2010;110:2858–902.
Shokeen M, Anderson CJ. Molecular imaging of cancer with copper-64 radiopharmaceuticals and positron emission tomography (PET). Acc Chem Res. 2009;42:832–41.
Connett JM, Anderson CJ, Guo LW, Schwarz SW, Zinn KR, Rogers BE, et al. Radioimmunotherapy with a 64Cu-labeled monoclonal antibody: a comparison with 67Cu. Proc Natl Acad Sci U S A. 1996;93:6814–8.
Binderup T, Knigge U, Mogensen AM, Hansen CP, Kjaer A. Quantitative gene expression of somatostatin receptors and noradrenaline transporter underlying scintigraphic results in patients with neuroendocrine tumors. Neuroendocrinology. 2008;87:223–32.
Pfeifer AK, Gregersen T, Grønbæk H, Hansen CP, Muller-Brand J, Herskind BK, et al. Peptide receptor radionuclide therapy with Y-DOTATOC and (177)Lu-DOTATOC in advanced neuroendocrine tumors: results from a Danish cohort treated in Switzerland. Neuroendocrinology. 2011;93:189–96.
Cwikla JB, Sankowski A, Seklecka N, Buscombe JR, Nasierowska-Guttmejer A, Jeziorski KG, et al. Efficacy of radionuclide treatment DOTATATE Y-90 in patients with progressive metastatic gastroenteropancreatic neuroendocrine carcinomas (GEP-NETs): a phase II study. Ann Oncol. 2010;21:787–94.
Kwekkeboom DJ, Bakker WH, Kam BL, Teunissen JJM, Kooij PPM, de Herder WW, et al. Treatment of patients with gastro-entero-pancreatic (GEP) tumours with the novel radiolabelled somatostatin analogue [177Lu-DOTA0, Tyr3] octreotate. Eur J Nucl Med. 2003;30:417–22.
Gabizon A, Papahadjopoulos D. Liposome formulations with prolonged circulation time in blood and enhanced uptake by tumors. Proc Natl Acad Sci U S A. 1988;85:6949–53.
Allen TM, Hansen C, Martin F, Redemann C, Yau-Young A. Liposomes containing synthetic lipid derivatives of poly(ethylene glycol) show prolonged circulation half-lives in vivo. Biochim Biophys Acta. 1991;1066:29–36.
Klibanov AL, Maruyama K, Torchilin VP, Huang L. Amphiphatic polyethyleneglycols effectively prolong the circulation time of liposomes. FEBS Lett. 1990;268:235–7.
Lee C-M, Choi Y, Huh EJ, Lee KY, Song H-C, Sun MJ, et al. Polyethylene glycol (PEG) modified 99mTc-HMPAO-liposome for improving blood circulation and biodistribution: The effect of the extent of PEGylation. Cancer Biother Radiopharm. 2005;20:620–8.
Chow T-H, Lin Y-Y, Hwang J-J, Wang H-E, Tseng Y-L, Pang VF, et al. Therapeutic efficacy evaluation of 111In-labeled PEGylated liposomal vinorelbine in murine colon carcinoma with multimodalities of molecular imaging. J Nucl Med. 2009;50:2073–81.
Drummond DC, Meyer O, Hong KL, Kirpotin DB, Papahadjopoulos D. Optimizing liposomes for delivery of chemotherapeutic agents to solid tumors. Pharmacol Rev. 1999;51:691–743.
Harrington KJ, Rowlinson-Busza G, Syrigos KN, Abra RM, Uster PS, Peters AM, et al. Influence of tumour size on uptake of 111In-DTPA-labelled pegylated liposomes in a human tumour xenograft model. Br J Cancer. 2000;83:684–8.
Petersen AL, Binderup T, Rasmussen P, Henriksen JR, Elema DR, Kjær A, et al. 64Cu loaded liposomes as positron emission tomography imaging agents. Biomaterials. 2011;32:2334–41.
Henriksen JR, Andresen TL. Thermodynamic profiling of peptide membranes interactions by isothermal titration calorimetry: a search for pores and micelles. Biophys J. 2011;101:100–9.
Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med. 2005;46:1023–7.
Harrington KJ, Mohammadtaghi S, Uster PS, Glass D, Peters AM, Vile RG, et al. Effective targeting of solid tumors in patients with locally advanced cancers by radiolabeled pegylated liposomes. Clin Can Res. 2001;7:243–54.
Gabizon A. Stealth liposomes and tumor targeting: one step further in the quest for the magic bullet. Clin Cancer Res. 2001;7:223–5.
Vallabhajosula S. Molecular imaging: radiopharmaceuticals for PET and SPECT. Berlin Heidelberg: Springer; 2009.
Tonkopi E, Ross AA, MacDonald A. CT dose for whole-body PET/CT examinations. AJR Am J Roentgenol. 2013;201:257–63.
Huang B, Law MW, Khong PL. Whole-body PET/CT scanning: estimation of radiation dose and cancer risk. Radiology. 2009;251:166–74.
Hamoudeh M, Kamleh MA, Diab R, Fessi H. Radionuclides delivery systems for nuclear imaging and radiotherapy of cancer. Adv Drug Deliv Rev. 2008;60:1329–46.
Wang H-E, Yu H-M, Lu Y-C, Heish N-N, Tseng Y-L, Huang K-L, et al. Internal radiotherapy and dosimetric study for 111In/177Lu-pegylated liposomes conjugates in tumor-bearing mice. Nucl Instrum Meth A. 2006;569:533–7.
Gritmon TF, Goedken MP, Choppin GR. The complexation of lanthanides by aminocarboxylate ligands – I. Stability constants. J Inorg Nucl Chem. 1977;39:2021–3.
Cacheris WP, Nickle SK, Sherry AD. Thermodynamic study of lanthanide complexes of 1,4,7-triazacyclononane-N,N′,N″,N‴-tetraacetic acid. Inorg Chem. 1987;26:958–60.
Wehrmann C, Senftleben S, Zachert C, Müller D, Baum RP. Results of individual patients dosimetry in peptide receptor radionuclide therapy with 177Lu DOTA-TATE and 177Lu DOTA-NOC. Cancer Biother Rad. 2007;22:406–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Financial support was kindly provided by the Danish Strategic Research Council (NABIIT; Ref. 2106-07-0033) and the Technical University of Denmark (DTU), the AP Møller Foundation, Danish National Advanced Technology Foundation, the Novo Nordisk Foundation, Rigshospitalets Research Council, Capital Region of Denmark and the Lundbeck Foundation.
Conflicts of interest
The authors declare no conflict of interest.
Ethical approval
All experimental procedures performed in this study involving animals were in accordance with the ethical standards and the guidelines set forth by the Danish Ministry of Justice. This article does not contain any studies with humans performed by any of the authors.
Appendices
Appendix A: Tables of absorbed radiation doses
Appendix B: Equations 1–6
The percentage of injected dose in blood (%IDblood) was calculated using:
where A b is the decay-corrected blood activity concentration at time t. The animal’s blood volume was calculated as 7.5 % of its body weight, m. D is the injected activity.
The percentage of injected dose in blood (%IDblood) between 1 and 48 h was fitted to the mono-exponential equation:
where β is the first-order disposition rate constant or the elimination rate constant, and B represents the fraction of the injected dose which is cleared from the blood at the disposition rate β. The fraction of the dose cleared initially can be estimated by 100 % -B. The terminal half-life (T ½β ) of the liposomes was determined using:
The available data did not permit accurate estimation of an initial half-life (T ½α ).
Accumulation in tumor and organs
Liposomal concentrations within each source organ as a function of time were determined from an ROI placed over the entire volume of the organ. The liposomal accumulation in the different organs was expressed as percentage of injected dose per gram (%ID/g) by using:
where A is the decay-corrected activity concentration in the tumor and normal organs, and ρ is the organ density and is assumed to be 1 g/cm3 for all organs and tumors.
The liposomal accumulation in the tumor was further parameterized by the standardized uptake value (SUV) and the tumor-to-muscle (T/M) ratio. The SUV values were calculated using:
where m is the animal's body weight and A is the decay-corrected activity concentration in the tumor. The PET data was not corrected for attenuation, which would give 5–15 % higher 64Cu concentrations than the values provided in this study, depending on the tissue in question.
For the 64Cu-liposome dosimetry study, activity concentration data, which were not corrected for 64Cu radioactive decay (Â), were used to construct activity concentration-time curves for each source organ. For dose calculations the the program OLINDA/EXM [27] were used. The residence time (T R ) from each source organ was used as input, and was calculated as:
where  is the activity concentration in the organ as a function of time, and V organ is the volume of the source organ. Integration was carried out using the trapezoidal method to obtain the area up to the last measured activity concentration ( ∗). An estimate of the long-term tail of the activity concentration-time curves for the different organs was made by fitting an exponential function ( ~ A ⋅ e − βt) to the two last measured points. The area beyond  ∗ was then estimated by  ∗/β. Since steady-state condition for the liposomal concentration within the measured tumor tissue was observed after 24 h (data not shown), the long-term tail of the activity concentration-time curves was assumed to be governed only by the radionuclide decay. The area beyond  ∗ was thus estimated by \( {\widehat{A}}^{\ast}\cdot \frac{T_{1/2}}{ln2} \), where T ½ is the half-life of the radionuclide.
In the OLINDA/EXM program, activity not assigned to a specific organ must be assigned to the remainder-of-body category. In our calculation, this was estimated as the full injected dose activity received by the body excluding the source organ doses. A separate T R was assigned to the remainder-of-body activity concentration-time curve.
For the 177Lu-liposome dosimetry study, 64Cu-liposomes were used as biological surrogates to study the biodistribution and estimate radiation dosimetry of 177Lu-liposomes. Thus, it was assumed that the 177Lu-liposomes follow virtually the same biodistribution and pharmacokinetics as the 64Cu-liposomes due to the encapsulation of the radionuclides inside the liposomes prohibiting the exchange of the radionuclides with the biological environment. 64Cu-liposome activity data for each source organ corrected for 64Cu radioactive decay were multiplied by the physical decay of 177Lu (\( {e}^{-\frac{ln2}{T_{1/2}}} \)) to obtain estimates for the 177Lu-liposome activity concentration in each source organ as a function of time. The T R from each source organ was calculated via equation S6.
Rights and permissions
About this article
Cite this article
Petersen, A.L., Henriksen, J.R., Binderup, T. et al. In vivo evaluation of PEGylated 64Cu-liposomes with theranostic and radiotherapeutic potential using micro PET/CT. Eur J Nucl Med Mol Imaging 43, 941–952 (2016). https://doi.org/10.1007/s00259-015-3272-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-015-3272-6