Abstract
Objectives
To evaluate the type and prevalence of associated injuries by using magnetic resonance imaging (MRI) in patients with anterior cruciate ligament (ACL) tears.
Methods
Data from the Natural Corollaries and Recovery after ACL injury multicenter longitudinal cohort study were analyzed. Between May 2016 and October 2018, patients aged between 15 and 40 years, who had experienced an ACL tear within the last 6 weeks and sought medical attention at one of seven healthcare clinics in Sweden, were invited to participate. The mean time from injury to MRI was 19.6 ± 15.2 days. An orthopedic knee surgeon and a musculoskeletal radiologist reviewed all the MRI scans. The following structures were assessed: posterior cruciate ligament (PCL), medial collateral ligament (MCL) complex, lateral collateral ligament (LCL), popliteus tendon, medial meniscus (MM), lateral meniscus (LM), and cartilage. In addition, the presence of bone bruising, impaction fractures in the lateral femoral condyle (LFC) or posterolateral tibia (PLT), and Segond fractures were also assessed.
Results
A total of 254 patients (48.4% males) with a mean age of 25.4 ± 7.1 years were included. The prevalence of associated injuries was as follows: PCL (0.4%), MCL {41.3% [superficial MCL and deep MCL (dMCL) 16.5%; isolated dMCL 24.8%]}, LCL (2.4%), MM (57.4%), LM (25.2%), cartilage (15.0%), bone bruising (92.9%), impaction fracture in the LFC (45.7%) and PLT (4.7%), and Segond fracture (7.5%).
Conclusions
The prevalence of associated injuries in patients with ACL tears was high. The findings reported in this study may serve as a reference tool for orthopedic surgeons and radiologists in the diagnosis of associated injuries using MRI in patients with ACL tears.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) tears are rarely isolated [1,2,3,4]. Thus, recognition of associated injuries in patients with ACL tears is essential. Misdiagnosed or untreated peripheral laxities are known causes of ACL graft failure [5]. LaPrade et al. [6] demonstrated that ACL graft forces increased significantly with varus loading at 0 and 30 degrees of flexion and internal rotation, after sectioning the lateral collateral ligament (LCL). Deficiency of the medial collateral ligament (MCL) complex is responsible for significantly increased forces in the ACL during valgus and external rotation [7, 8]. Meniscal and cartilage injuries are frequently observed in patients with ACL tears [1, 3, 9], and they are associated with increased knee laxity [3, 10], inferior subjective knee outcomes, and osteoarthritis development [11,12,13]. Meniscal ramp lesions, which can be easily overlooked during standard arthroscopic evaluation (using the anteromedial and anterolateral portals) [14, 15], have been associated with increased anterior tibial translation, internal and external rotation, pivot shift [16, 17], and accelerated cartilage degeneration in the medial compartment [18]. Bone bruising patterns are regarded as a footprint of the mechanism of injury, offering insights into possible associated injuries [19,20,21,22]. Finally, impaction fractures of the lateral femoral condyle (LFC), posterolateral tibia (PLT), and the Segond fracture have been associated with poorer outcomes and increased anterolateral rotatory laxity in ACL-injured knees [23,24,25].
Therefore, knowledge about the presence of associated injuries in ACL tears is essential for the orthopedic surgeon to maximize the treatment outcome of patients with ACL injuries.
Magnetic resonance imaging (MRI) is regarded (due to its high accuracy in evaluating soft tissues) as the best imaging modality to diagnose associated injuries in ACL tears [26].
The purpose of the present study was to provide a comprehensive analysis, which can be used as a reference tool for radiologists and orthopedic surgeons, regarding the type and prevalence of associated injuries on MRI in patients with ACL tears.
Materials and methods
Ethical approval was obtained from the Regional Ethics Committee of Linköping, Sweden (no. 2016/44–31 and 2017/221–32). All patients provided written informed consent before participation. Data were extracted from the Natural Corollaries and Recovery after ACL injury (NACOX) study [27]. Patients were recruited between May 2016 and October 2018 from seven orthopedic clinics across Sweden. The inclusion criteria were an ACL injury sustained no more than 6 weeks before presentation and an age between 15 and 40 years at the time of injury. The exclusion criteria were previous ACL injury or ACL reconstruction (ACLR), fractures requiring separate treatment, inability to understand written or spoken Swedish language, cognitive impairments, or other illnesses or injuries that impaired function (e.g., fibromyalgia, rheumatic diseases, or other diagnoses associated with chronic pain). ACL tears were clinically diagnosed by an orthopedic surgeon and verified using MRI. In this study, only patients with available MRI data were included. Patients who only had a clinical diagnosis of ACL injury were not included.
The MRI prevalence and the factors associated with meniscal ramp lesions and MCL complex injuries from the NACOX study have been previously reported [1, 2].
Radiological assessment
A total of 210 patients underwent MRI at two institutions (Capio Artro Clinic, Stockholm Sweden, and Linköping University Hospital, Linköping, Sweden). The remaining patients participating in the NACOX study (n = 44) underwent MRI at other institutions [27]. MRI was performed using a 1.5-T (Siemens) (n = 115) and 3.0-T scanners (Philips) (n = 139). A detailed description of MRI sequences is reported in Table 1. A sensitivity analysis of the MRI scanners (1.5-T vs. 3.0-T) is reported in the Appendix Table 4. The mean time from injury to MRI was 19.6 ± 15.2 days. All MRI examinations were retrospectively and independently assessed by an orthopedic knee surgeon (R.C.) and a musculoskeletal radiologist (F.v.d.B.) (fair interrater reliability: median Kappa 0.51). A conjoined assessment was performed to reach a consensus in the event of inconsistencies.
The classification of associated injuries was based on the ACL Osteoarthritis Score (ACLOAS) for ligament, meniscus, and cartilage injuries [28]; Greif classification for meniscal ramp lesions [29]; and Sanders classification for bone bruising patterns [19]. The classification and grading were as follows:
-
The posterior cruciate ligament (PCL) was classified as intact or injured.
-
The MCL and LCL were classified as intact, partially or completely torn. Partial tears were defined as a partial rupture or discontinuity with preserved fibers, whereas complete tears were defined as complete ligament disruption [28]. Injury localization was also assessed [proximal (proximal third), mid-substance (central third), or distal (distal third)] [28]. A deep MCL (dMCL) injury was defined as a tear of the meniscofemoral and/or meniscotibial ligaments. Isolated dMCL tears were defined as isolated tears of the meniscofemoral and/or meniscotibial ligaments with intact superficial MCL (sMCL) [2]. The posterior oblique ligament (POL) was classified as intact or injured. Similarly, the popliteus tendon was classified as intact or injured.
-
The medial meniscus (MM) and lateral meniscus (LM) were classified as normal, horizontal tears, radial and vertical tears, bucket handle tears, complex tears, root tears, and ramp lesions (for the MM) [28]. The locations were registered as posterior horn, corpus, or anterior horn. MM ramp lesions were classified into seven subtypes according to Greif et al. [29]: type 1, meniscocapsular ligament tears; type 2, partial superior peripheral meniscal horn tears; type 3A, partial inferior peripheral posterior horn meniscal tears; type 3B, meniscotibial ligament tears; type 4A, complete peripheral posterior horn meniscal tears; type 4B, complete meniscocapsular junction tears; and type 5, peripheral posterior horn meniscal double tears.
-
Cartilage lesions were classified as partial thickness, full thickness, or degeneration [28]. The injury locations were the medial femoral condyle (MFC), lateral femoral condyle (LFC), medial or lateral tibial plateau, trochlea, or patella.
-
Bone bruising patterns were documented and classified as described by Sanders et al. [19] in pivot-shift, dashboard, and hyperextension injuries. Pivot-shift bone bruising was defined as the presence of bone marrow edema in the posterolateral area of the lateral tibial plateau and the central area of the LFC. If the bone bruising pattern did not fit any of the patterns described by Sanders et al. [19], it was classified as “other”. In addition, bone bruising in the MFC and posteromedial tibia (PMT) was also assessed.
-
Impaction fractures in the LFC and posterolateral tibia (PLT) were defined as depressions with a normal or injured cartilage surface [28].
-
The presence of a Segond fracture was also documented [30].
Statistical analysis
The present study serves as a descriptive study. All data were analyzed using Microsoft Excel (version 2018).
Results
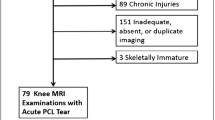
A total of 275 patients were included in the NACOX study. Eight patients only had a clinical diagnosis of ACL injury (no MRI), and the MRI scans of 13 patients were not available for analysis. Finally, a total of 254 patients (48.4% males) with a mean age of 25.4 ± 7.1 years and a mean body mass index of 23.8 ± 3.3 were included. The median (range) pre-injury Tegner activity score was 7 (2–9). Activity at the time of injury was as follows: football (37.4%), skiing (18.5%), floorball (13.4%), handball (5.9%), daily life activities (3.1%), martial arts (2.4%), basketball (2.4%), and others (16.7%).
Only one patient (0.4%) was identified with a PCL tear.
MCL complex and LCL injuries
Overall, MCL (sMCL and dMCL) injuries (Fig. 1) were identified in 42 patients (16.5%). Isolated sMCL injuries were not observed. In the event of an sMCL injury, a dMCL (particularly the meniscofemoral ligament) injury was always present. The severity and location of the sMCL injuries are displayed in Table 2. Isolated dMCL injuries (Fig. 2) were observed in 63 patients (24.8%). All but one tear involved the meniscofemoral ligament. Only one patient had an isolated tear of the meniscotibial ligament. POL injuries (Fig. 3) were observed in 12 patients (4.7%). The POL was never injured in isolation. In all the cases, an MCL (sMCL and dMCL) injury was present [2].
Lateral collateral ligament injuries (Fig. 4) were identified in six patients (2.4%). The severity and location of the injuries are reported in Table 2. No popliteal tendon injuries were observed.
MM and LM injuries
Overall, MM and LM injuries were identified in 146 (57.4%) and 64 (25.2%) patients, respectively. The types, distributions, and locations of injuries are reported in Table 3. Figure 5 displays a meniscal ramp lesion type 4B (complete meniscocapsular junction tear), whereas Fig. 6 demonstrates a radial-vertical LM posterior horn tear.
Cartilage injuries
Cartilage injuries were identified in 38 (15.0%) patients. Partial- and full-thickness tears (Fig. 7) and cartilage degeneration were observed in 25 (65.8%), nine (23.7%), and four (10.5%) patients, respectively. The injury locations were as follows: MFC (five patients, 13.2%), LFC (13 patients, 34.2%), lateral tibial plateau (two patients, 5.3%), trochlea (one patient, 2.6%), and patella (17 patients, 44.7%).
Bone bruising, impaction fractures, and Segond fracture
Bone bruising was observed in 236 patients (92.9%). The injury patterns were as follows: pivot shift (Fig. 8) (184 patients, 78%) and other (52 patients, 22%). Dashboard or hyperextension patterns were not observed. Additionally, MFC and PMT bone bruising (Fig. 9) were observed in 48 (18.9%) and 100 (39.4%) patients, respectively.
Impaction fractures of the LFC and PLT (Fig. 10) were identified in 116 (45.7%) and 12 (4.7%) patients, respectively. Nineteen (7.5%) patients had Segond fractures (Fig. 11).
Discussion
The most important finding of this study was the high prevalence of associated injuries in patients with ACL tears. This is consistent with previous research, suggesting that ACL tears are rarely isolated [1,2,3,4, 9, 21].
In the present study, the prevalence of MCL (sMCL and dMCL) and isolated dMCL injuries was 41.3% (16.5% + 24.8%). POL injuries were identified in 4.7% of patients and were never isolated. The aforementioned injuries were always associated with MCL (sMCL and dMCL) tears. Previous MRI studies have reported a variable prevalence (22–67%) of MCL complex injuries [4, 31,32,33]. This large variation may be the result of different intervals from injury to MRI as well as differences in the assessment and criteria used to define injuries to the MCL complex structures (sMCL, dMCL, and POL). In the present study, partial or complete sMCL tears were always associated with dMCL (meniscofemoral ligament) tears [2]. The load to failure of the dMCL is significantly lower than that of the sMCL (101 N and 557 N, respectively) [34]. A dMCL tear may occur before an sMCL tear. This may also explain why dMCL tears occurred in isolation (with intact sMCL). In the event of isolated dMCL tears, the meniscofemoral ligament was injured in all but one case. This ligament is thinner than the meniscotibial ligament [35, 36].
Lateral collateral ligament injuries were rare (2.4%). This might be related to the fact that the most common mechanism of ACL injuries in sports activities is a valgus-external rotation (“knee-in & toe-out”) [37], whereas the LCL is the primary restraint to varus loading [38]. The same consideration could be applied to popliteus tendon injuries which were not identified in any patient of the present cohort. However, recognition of these injuries is important, as a deficiency in the posterolateral corner (PLC) structures is responsible for persistent laxity and increased loads on the ACL graft [6, 39]. A previous study reported high rates (50–76%) of missed clinical diagnoses of PLC injuries by orthopedic surgeons [40].
Overall, MM and LM injuries were the most common (57.4% and 25.2%, respectively). Comparisons of prevalence with other studies are difficult as most of the relevant literature is based on arthroscopic findings [3, 9, 11, 21, 41]. Most meniscal injuries occurred in the posterior horn of the meniscus. This is not surprising because the posterior horns of the MM and LM provide secondary stability against anterior tibial translation [42] and internal tibial rotation [43], respectively. Interestingly, the most common meniscal injuries were MM ramp lesions. These injuries were present in 39.4% of the patients, as previously reported (overall 68.5% of MM injuries) [1]. Even though arthroscopy is generally regarded as the gold standard for the diagnosis of ramp lesions, previous studies have reported a significantly low prevalence (9–17%) of meniscal ramp lesions diagnosed arthroscopically at the time of ACLR [44,45,46,47]. This may be because the standard anteromedial and anterolateral portals have low sensitivity when diagnosing ramp lesions [14]. Sonnery-Cottet et al. [14] reported a 40% prevalence of meniscal ramp lesions (similar to that in our study) during ACLR. Interestingly, only 58% of these tears were diagnosed using the modified Gillquist view. Forty-two percent were diagnosed after probing and debridement through the posteromedial portal. Previous studies may have overlooked a significant number of meniscal ramp lesions identified by Sonnery-Cottet et al. [14] after debridement through a posteromedial portal and by us via MRI. Similar to our study, Balazs et al. [48] reported an overall MRI prevalence of meniscal ramp lesions of 42% in patients with ACL injuries. The meniscal ramp area can be visualized using an MRI performed with an appropriate magnetic field strength and spatial resolution [48].
Cartilage injuries were identified in 15% of the patients. Previous studies have reported a higher prevalence (16–28%) of cartilage injuries diagnosed arthroscopically at the time of ACLR [3, 9, 11, 49]. Compared with arthroscopy, MRI has moderate sensitivity for detecting cartilage injuries [50]. In addition, the risk of cartilage injury is directly correlated with the increased time since ACL injury [3, 9]. In the present study, the mean time from injury to MRI was relatively short (19.6 ± 15.2 days). These factors may explain the lower prevalence of cartilage injuries in this study than that in previous studies.
Bone bruising was observed in most patients (92.9%). The most frequent pattern (78% of patients) was the pivot-shift pattern (bone marrow edema in the posterolateral area of the lateral tibial plateau and central area of the LFC). This might be explained by the fact that most ACL injuries and the pivot-shift bone-bruising pattern share the same trauma mechanism [flexion valgus and external rotation (pivot-shift)] [19, 51, 52]. It is hypothesized that, during the pivot shift mechanism, the posterolateral aspect of the lateral tibial plateau subluxates anteriorly and impinges with the central part of the LFC [19, 21]. In line with the present study, Yoon et al. [21] reported a high prevalence (84%) of bone bruising in patients with ACL injuries (MRI performed within 6 weeks of the trauma), with most bone bruising occurring in the LFC (68%) and the lateral tibial plateau (73%). These findings support the hypothesis that bone bruising should be interpreted as a footprint of the mechanism of injury [19]. Impaction fractures in the LFC and PLT (present in 45.7% and 4.7% of the patients, respectively) can also be observed in the context of a pivot-shift mechanism [19, 53]. Interestingly, these impaction fractures are associated with progressive cartilage degeneration, greater anterolateral rotatory laxity, and poorer postoperative outcomes [23, 24]. Bone bruising was also commonly observed in the MFC and PMT (18.9% and 39.4%, respectively). It has been hypothesized that bone bruising in the medial compartment occurs as the result of a contrecoup mechanism. If energy trauma is not dissipated by the initial pivot-shift mechanism, a contrecoup injury with impaction of the MFC and PMT may occur as a result of sudden tibial reduction with compensatory varus alignment and internal tibial rotation [52]. However, we previously reported a strong association between MFC bone bruising and dMCL injuries in the same patient cohort from the NACOX study [2]. We hypothesized that the avulsion of the meniscofemoral ligament from the MFC may be responsible for bone bruising in the MFC. PMT bone bruising has been strongly associated with MM ramp lesions [1] as they probably share the same trauma mechanism [1, 54].
Segond fractures were present in a small number of patients (7.5%). This rate is consistent with that reported in the literature [55]. The low rate of Segond fractures may be explained by the fact that this injury is thought to occur after internal rotation and varus stress [30], whereas most ACL injuries occur after external rotation and valgus stress [37]. However, it is important to note that this injury has been associated with increased anterolateral rotatory laxity in ACL-injured knee [25].
MRI is generally considered the best imaging modality for diagnosing associated injuries in patients with ACL tears. Although MRI cannot be regarded as a substitute for a thorough clinical examination, it can serve as an alert to orthopedic surgeons, guiding them to pay particular attention (during the clinical assessment) to the injured structures on imaging [2]. Additionally, MRI is useful for preoperative planning and can affect clinical decision-making in patients with ACL injuries.
The main strength of this study was that all MRI scans were reviewed by two experienced examiners (an orthopedic surgeon specializing in knee surgery and a musculoskeletal radiologist). A relatively high prevalence (54.5%) of MRI scans was obtained using a 3.0 Tesla scanner. Moreover, the time from injury to MRI was relatively short (19.6 ± 15.2 days). This prevented the edema in the injured structures (and bone bruising) from resolving and improved the diagnosis of the associated injuries. Associated injuries were evaluated and reported according to established classifications [19, 28]. Furthermore, meniscal ramp lesions were evaluated using well-defined MRI pathological signs [29]. The injury patterns of the MCL complex (sMCL, dMCL, and POL) were analyzed in detail. This is clinically relevant because, in the event of surgical treatment, all MCL complex structures should be repaired or reconstructed [56]. Finally, the cohort studied (n = 254) was relatively large.
Some limitations are present. First, the patients underwent MRI scans at different institutions using different scanners. However, all examinations were performed with a strength of 1.5 or 3.0 T. Moreover, the MRIs were assessed by the same two examiners. Second, some associated injuries (ex. cartilage injuries in the patellofemoral joint) are unlikely to have occurred in concomitance with the ACL injury. However, the purpose of the study was to provide an overview of all associated injuries in the ACL-injured patient, rather than evaluating only them possibly occurring in concomitance with the ACL tear.
In conclusion, the prevalence of associated injuries in patients with ACL tears was very high. The findings reported in this study may serve as a reference tool for orthopedic surgeons and radiologists in the diagnosis of associated injuries in patients with ACL tears using MRI.
References
Cristiani R, van de Bunt F, Kvist J, Stålman A. High prevalence of meniscal ramp lesions in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2023;31:316–24.
Cristiani R, van de Bunt F, Kvist J, Stålman A. High prevalence of superficial and deep medial collateral ligament injuries on magnetic resonance imaging in patients with anterior cruciate ligament tears. Arthroscopy. 2024;40:103–10.
Cristiani R, Janarv PM, Engström B, Edman G, Forssblad M, Stålman A. Delayed anterior cruciate ligament reconstruction increases the risk of abnormal prereconstruction laxity, cartilage, and medial meniscus injuries. Arthroscopy. 2021;37:1214–20.
Willinger L, Balendra G, Pai V, et al. High incidence of superficial and deep medial collateral ligament injuries in “isolated” anterior cruciate ligament ruptures: a long overlooked injury. Knee Surg Sports Traumatol Arthrosc. 2022;30:167–75.
Samitier G, Marcano AI, Alentorn-Geli E, Cugat R, Farmer KW, Moser MW. Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg. 2015;3:220–40.
LaPrade RF, Resig S, Wentorf F, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med. 1999;27:469–75.
Shapiro MS, Markolf KL, Finerman GA, Mitchell PW. The effect of section of the medial collateral ligament on force generated in the anterior cruciate ligament. J Bone Joint Surg Am. 1991;73:248–56.
Mehl JT, Kia C, Murphy M, et al. Posteromedial ligament repair of the knee with suture tape augmentation: a biomechanical study. Am J Sports Med. 2019;47:2952–9.
Brambilla L, Pulici L, Carimati G, et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med. 2015;43:2966–73.
Hoshino Y, Hiroshima Y, Miyaji N, et al. Unrepaired lateral meniscus tears lead to remaining pivot-shift in ACL-reconstructed knees. Knee Surg Sports Traumatol Arthrosc. 2020;28:3504–10.
Røtterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Arøen A. Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: a nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up. Am J Sports Med. 2013;41:535–43.
Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–43.
Pedersen M, Johnson JL, Grindem H, Magnusson K, Snyder-Mackler L, Risberg MA. Meniscus or cartilage injury at the time of anterior cruciate ligament tear is associated with worse prognosis for patient-reported outcome 2 to 10 years after anterior cruciate ligament injury: a systematic review. J Orthop Sports Phys Ther. 2020;50:490–502.
Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921–6.
Cristiani R, Mouton C, Stålman A, Seil R. Meniscal ramp lesions: a lot is known, but a lot is also unknown…. Knee Surg Sports Traumatol Arthrosc. 2023;31:2535–9.
Mouton C, Magosch A, Pape D, Hoffmann A, Nührenbörger C, Seil R. Ramp lesions of the medial meniscus are associated with a higher grade of dynamic rotatory laxity in ACL-injured patients in comparison to patients with an isolated injury. Knee Surg Sports Traumatol Arthrosc. 2020;28:1023–8.
DePhillipo NN, Moatshe G, Brady A, et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med. 2018;46:2422–31.
Guimaraes JB, Schwaiger BJ, Gersing AS, et al. Meniscal ramp lesions: frequency, natural history, and the effect on knee cartilage over 2 years in subjects with anterior cruciate ligament tears. Skeletal Radiol. 2021;50:551–8.
Sanders TG, Medynski MA, Feller JF, Lawhorn KW (2000) Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics 20 Spec No:S135–51
Illingworth KD, Hensler D, Casagranda B, Borrero C, van Eck CF, Fu FH. Relationship between bone bruise volume and the presence of meniscal tears in acute anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2014;22:2181–6.
Yoon KH, Yoo JH, Kim KI. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am. 2011;93:1510–8.
Zhang L, Hacke JD, Garrett WE, Liu H, Yu B. bone bruises associated with anterior cruciate ligament injury as indicators of injury mechanism: a systematic review. Sports Med. 2019;49:453–62.
Mostowy M, Ruzik K, Ebisz M, LaPrade RF, Malinowski K. Impaction fractures of the lateral femoral condyle related to anterior cruciate ligament injury: a scoping review concerning diagnosis, prevalence, clinical importance, and management. Clin Orthop Surg. 2023;15:781–92.
Bernholt DL, Dornan GJ, DePhillipo NN, Aman ZS, Kennedy MI, LaPrade RF. High-grade posterolateral tibial plateau impaction fractures in the setting of a primary anterior cruciate ligament tear are correlated with an increased preoperative pivot shift and inferior postoperative outcomes after anterior cruciate ligament reconstruction. Am J Sports Med. 2020;48:2185–94.
Monaco E, Mazza D, Redler A, et al. Segond’s fracture: a biomechanical cadaveric study using navigation. J Orthop Traumatol. 2017;18:343–8.
Mohankumar R, White LM, Naraghi A. Pitfalls and pearls in MRI of the knee. AJR Am J Roentgenol. 2014;203:516–30.
Kvist J, Gauffin H, Tigerstrand Grevnerts H, et al. Natural corollaries and recovery after acute ACL injury: the NACOX cohort study protocol. BMJ Open. 2018;8(6): e020543.
Roemer FW, Frobell R, Lohmander LS, Niu J, Guermazi A. Anterior cruciate ligament osteoarthritis score (ACLOAS): longitudinal MRI-based whole joint assessment of anterior cruciate ligament injury. Osteoarthritis Cartilage. 2014;22:668–82.
Greif DN, Baraga MG, Rizzo MG, et al. MRI appearance of the different meniscal ramp lesion types, with clinical and arthroscopic correlation. Skeletal Radiol. 2020;49:677–89.
Segond P. Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. Progres Med. 1879;7:340–1.
Helito CP, Helito PVP, Leão RV, Demange MK, Bordalo-Rodrigues M. Anterolateral ligament abnormalities are associated with peripheral ligament and osseous injuries in acute ruptures of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2017;25:1140–8.
Kim SH, Seo HJ, Seo DW, Kim KI, Lee SH. Analysis of risk factors for ramp lesions associated with anterior cruciate ligament injury. Am J Sports Med. 2020;48:1673–81.
Spindler KP, Schils JP, Bergfeld JA, et al. Prospective study of osseous, articular, and meniscal lesions in recent anterior cruciate ligament tears by magnetic resonance imaging and arthroscopy. Am J Sports Med. 1993;21:551–7.
Wijdicks CA, Ewart DT, Nuckley DJ, Johansen S, Engebretsen L, Laprade RF. Structural properties of the primary medial knee ligaments. Am J Sports Med. 2010;38:1638–46.
LaPrade MD, Kennedy MI, Wijdicks CA, LaPrade RF. Anatomy and biomechanics of the medial side of the knee and their surgical implications. Sports Med Arthrosc Rev. 2015;23:63–70.
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–10.
Kobayashi H, Kanamura T, Koshida S, et al. Mechanisms of the anterior cruciate ligament injury in sports activities: a twenty-year clinical research of 1,700 athletes. J Sports Sci Med. 2010;9:669–75.
Shon OJ, Park JW, Kim BJ. Current concepts of posterolateral corner injuries of the knee. Knee Surg Relat Res. 2017;29:256–68.
Bonanzinga T, Signorelli C, Lopomo N, et al. Biomechanical effect of posterolateral corner sectioning after ACL injury and reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23:2918–24.
Pacheco RJ, Ayre CA, Bollen SR. Posterolateral corner injuries of the knee: a serious injury commonly missed. J Bone Joint Surg Br. 2011;93:194–7.
Granan LP, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004–2007: baseline epidemiology. Acta Orthop. 2009;80:563–7.
Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res. 2000;18:109–15.
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38:1591–7.
Arner JW, Herbst E, Burnham JM, et al. MRI can accurately detect meniscal ramp lesions of the knee. Knee Surg Sports Traumatol Arthrosc. 2017;25:3955–60.
Bollen SR. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognised association. J Bone Joint Surg Br. 2010;92:222–3.
DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:2233–7.
Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39:832–7.
Balazs GC, Greditzer HG 4th, Wang D, Marom N, Potter HG, Marx RG, Rodeo SA, Williams RJ 3rd. Ramp lesions of the medial meniscus in patients undergoing primary and revision ACL reconstruction: prevalence and risk factors. Orthop J Sports Med. 2019;7:2325967119843509.
Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW; MOON Consortium and the MARS Group (2011) Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med 39:1889–93
Danieli MV, Guerreiro JP, Queiroz Ad, et al. Diagnosis and classification of chondral knee injuries: comparison between magnetic resonance imaging and arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2016;24:1627–33.
Hayes CW, Brigido MK, Jamadar DA, Propeck T (2000) Mechanism-based pattern approach to classification of complex injuries of the knee depicted at MR imaging. Radiographics 20 Spec No:S121–34
Kaplan PA, Gehl RH, Dussault RG, Anderson MW, Diduch DR. Bone contusions of the posterior lip of the medial tibial plateau (contrecoup injury) and associated internal derangements of the knee at MR imaging. Radiology. 1999;211:747–53.
Yoo JH, Yang BK, Ryu HK. A case of fracture of posterior margin of lateral tibial plateau by pivot shift mechanism in chronic ACL insufficiency. Arch Orthop Trauma Surg. 2009;129:363–7.
Green JS, Moran J, Marcel A, et al. Posteromedial tibial plateau bone bruises are associated with medial meniscal ramp lesions in patients with concomitant anterior cruciate ligament ruptures: a systematic review & meta-analysis. Phys Sportsmed. 2023;51:531–8.
Phua SKA, Lim JY, Li T, Ho SWL. The segond fracture: A narrative review of the anatomy, biomechanics and clinical implications. J Clin Orthop Trauma. 2023;38: 102127.
Wijdicks CA, Griffith CJ, Johansen S, Engebretsen L, LaPrade RF. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. 2010;92:1266–80.
Acknowledgements
This study is part of the NACOX-cohort, a project investigating the natural corollaries and recovery after acute ACL injury. We would like to thank all collaborators in the NACOX study and Henrik Hedevik for his contribution to data management. The NACOX-cohort study is supported by the Swedish Research Council, the Swedish Research Council for Sport Science, the Medical Research Council of Southeast, and ALF Grants Region Östergötland.
Funding
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no competing interests.
Additional information
IRB
Ethical approval was obtained by the regional ethics committee in Linköping, Sweden (Dnr 2016/44–31 and 2017/221–32). All patients signed informed consent to participate.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cristiani, R., van de Bunt, F., Kvist, J. et al. High prevalence of associated injuries in anterior cruciate ligament tears: A detailed magnetic resonance imaging analysis of 254 patients. Skeletal Radiol (2024). https://doi.org/10.1007/s00256-024-04665-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00256-024-04665-9