Abstract
Objectives
To determine the frequency of non-diagnostic and discordant results from bone and soft tissue biopsies performed at our institution over a 3-year period and to investigate whether implementation of a weekly musculoskeletal radiology-pathology correlation conference decreased the time to appropriate patient management in cases of discordance.
Methods
Consecutive image-guided core needle biopsy results obtained over a 12 month period of time were reviewed in a retrospective fashion. Following implementation of the correlation conference, subsequent consecutive image-guided core needle biopsy results obtained over a 26 month period of time were reviewed in a prospective fashion. For non-diagnostic and discordant cases, the time in days from date of availability of the biopsy result to date of documentation of a specific follow-up action plan was recorded.
Results
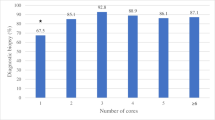
Diagnostic yield was 96.5% and 94.9% for the retrospective and prospective periods, respectively. There were four discordant results in the retrospective cohort (1.7%) and seven discordant results in the prospective cohort (2.1%). Following implementation of the weekly correlation conference, there was significant decrease (p < 0.05) in median time from a discordant biopsy result to follow-up action plan. There were no unnecessary surgeries, litigation, or other unfavorable consequences in either cohort.
Conclusion
Image-guided core needle biopsies of bone and soft tissue provide high diagnostic yield, often with specific diagnoses. The statistically significant decrease in number of days to follow-up action plan for discordant results suggests radiology-pathology review has a positive impact on patient care. Subjective benefits from communication and educational standpoints are also noteworthy.


Similar content being viewed by others
References
Traina F, Errani C, Toscano A, et al. Current concepts in the biopsy of musculoskeletal tumors: AAOS exhibit selection. J Bone Joint Surg Am. 2015;97(2):e7.
Yang J, Frassica FJ, Fayad L, Clark DP, Weber KL. Analysis of nondiagnostic results after image-guided needle biopsies of musculoskeletal lesions. Clin Orthop Relat Res. 2010;468(11):3103–11.
Trieu J, Schlicht SM, Choong PF. Diagnosing musculoskeletal tumours: how accurate is CT-guided core needle biopsy? Eur J Surg Oncol. 2016;42(7):1049–56.
Kim SY, Chung HW. Small musculoskeletal soft-tissue lesions: US-guided core needle biopsy--comparative study of diagnostic yields according to lesion size. Radiology. 2016;278(1):156–63.
Sung KS, Seo SW, Shon MS. The diagnostic value of needle biopsy for musculoskeletal lesions. Int Orthop. 2009;33(6):1701–6.
Rimondi E, Staals EL, Errani C, Bianchi G, Casadei R, AlberghiniM MMC, et al. Percutaneous CT-guided biopsy of the spine: results of 430 biopsies. Eur Spine J. 2008;17(7):975–81.
Ashford RU, McCarthy SW, Scolyer RA, Bonar SF, Karim RZ, Stalley PD. Surgical biopsy with intra-operative frozen section. An accurate and cost-effective method for diagnosis of musculoskeletal sarcomas. J Bone Joint Surg Br. 2006;88(9):1207–11.
Lopez JI, Del Cura JL, Zabala R, Bilbao FJ. Usefulness and limitations of ultrasound-guided core biopsy in the diagnosis of musculoskeletal tumours. APMIS. 2005;113(5):353–60.
Liu PT, Valadez SD, Chivers FS, Roberts CC, Beauchamp CP. Anatomically based guidelines for core needle biopsy of bone tumors: implications for limb-sparing surgery. Radiographics. 2007;27(1):189–205.
Issakov J, Flusser G, Kollender Y, Merimsky O, Lifschitz-Mercer B, Meller I. Computed tomography-guided core needle biopsy for bone and soft tissue tumors. Isr Med Assoc J. 2003;5(1):28–30.
Hau A, Kim I, Kattapuram S, Hornicek FJ, Rosenberg AE, Gebhardt MC, et al. Accuracy of CT-guided biopsies in 359 patients with musculoskeletal lesions. Skelet Radiol. 2002;31(6):349–53.
Torriani M, Etchebehere M, Amstalden E. Sonographically guided core needle biopsy of bone and soft tissue tumors. J Ultrasound Med. 2002;21(3):275–81.
Virayavanich W, Ringler MD, Chin CT, et al. CT-guided biopsy of bone and soft-tissue lesions: role of on-site immediate cytologic evaluation. J Vasc Interv Radiol. 2011;22:1024–30.
Wu JS, Goldsmith JD, Horwich PJ, Shetty SK, Hochman MG. Bone and soft-tissue lesions: what factors affect diagnostic yield of image-guided core-needle biopsy? Radiology. 2008;248:962–70.
Didolkar MM, Anderson ME, Hochman MG, et al. Image guided core needle biopsy of musculoskeletal lesions: are nondiagnostic results clinically useful? Clin Orthop Relat Res 2013;471:3601–3609.
Dupuy DE, Rosenberg AE, Punyaratabandhu T, Tan MH, Mankin HJ. Accuracy of CT-guided needle biopsy of musculoskeletal neoplasms. AJR Am J Roentgenol. 1998;171(3):759–62.
Park VY, Kim EK, Moon HJ, Yoon JH, Kim MJ. Evaluating imaging-pathology concordance and discordance after ultrasound-guided breast biopsy. Ultrasonography. 2018;37(2):107–20.
American College of Radiology. ACR practice parameter for communication of diagnostic imaging findings. 2014; Available at: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/us-guidedbreast.pdf. Accessed June 25, 2019.
American College of Radiology. ACR practice parameter for communication of diagnostic imaging findings. 2014; Available at: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/stereo-breast.pdf. Accessed June 25, 2019.
American Society of Breast Surgeons. Concordance assessment following image-guided breast biopsy. https://www.breastsurgeons.org/docs/statements/Concordance-Assessment-Following-Image-Guided-Breast-Biopsy.pdf. Accessed March 5, 2020.
Schueller G, Schueller-Weidekamm C, Helbich TH. Accuracy of ultrasound-guided, large-core needle breast biopsy. Eur Radiol. 2008;18:1761–73.
Parikh J, Tickman R. Image-guided tissue sampling: where radiology meets pathology. Breast J. 2005;11(6):403–9.
Dane B, Doshi A, Gfytopoulos S, Bhattacharji P, Recht M, Moore W. Automated radiology-pathology module correlation using a novel report matching algorithm by organ system. Acad Radiol. 2018;25:673–80.
Filippiadis DK, Charalampopoulos G, Mazioti A, Keramida K, Kelekis A. Bone and soft-tissue biopsies: what you need to know. Semin Interv Radiol. 2018;35:215–20.
Wallace AN, McWilliams SR, Wallace A, et al. Drill-assisted biopsy of the axial and appendicular skeleton: safety, technical success, and diagnostic efficacy. J Vasc Interv Radiol. 2016;27(10):1618–22.
Miquelestorena-Standley E, Jourdan ML, Collin C, et al. Effect of decalcification protocols on immunohistochemistry and molecular analyses of bone samples. Mod Pathol. 2020. https://doi.org/10.1038/s41379-020-0503-6.
Ezuddin NS, Pretell-Mazzini J, Yechieli RL, Kerr DA, Wilky BA, Subhawong TK. Local recurrence of soft-tissue sarcoma: issues in imaging surveillance strategy. Skelet Radiol. 2018;47(12):1595–606.
Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–81.
Ginat DT, Cipriani NA, Christoforidis G. Educational impact of trainee-facilitated head and neck radiology-pathology correlation conferences. Head Neck Pathol. 2019;13:177–81.
Brady AP. Error and discrepancy in radiology: inevitable or avoidable? Insights Imaging. 2017;8:171–82.
Prakash S, Venkataraman S, Slanetz PJ, et al. Improving patient care by incorporation of multidisciplinary breast radiology-pathology correlation conference. Can Assoc Radiol J. 2016;67:122–9.
Rao VM, Levin DC. The value-added services of hospital-based radiology groups. J Am Coll Radiol 2011;8:626–630.
Abramson RG, Berger PE, Brant-Zawadzki MN. Accountable care organizations and radiology: threat or opportunity? J Am Coll Radiol. 2012;9:900–6.
Accordino MK, Wright JD, Vasan S, Neugut AI, Hillyer GC, Hershman DL. Factors and costs associated with delay in treatment initiation and prolonged length of stay with inpatient EPOCH chemotherapy in patients with hematologic malignancies. Cancer Investig. 2017;35:202–14.
Filice RW. Radiology-pathology correlation to facilitate peer learning: an overview including recent artificial intelligence methods. J Am Coll Radiol. 2019;16:1279–85.
Filice RW. Deep-learning language-modeling approach for automated, personalized, and iterative radiology-pathology correlation. J Am Coll Radiol. 2019;16:1286–91.
Doshi AM, Huang C, Melamud K, et al. Utility of an automated radiology-pathology feedback tool. J Am Coll Radiol. 2019;16:1211–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Banks, J.S., Garner, H.W., Chow, A.Z. et al. Radiology-pathology correlation for bone and soft tissue tumors or tumor-like masses: single institutional experience after implementation of a weekly conference. Skeletal Radiol 50, 731–738 (2021). https://doi.org/10.1007/s00256-020-03616-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03616-4