Abstract
Objectives
To describe the radiographic and MRI features of histologically proven Langerhans cell histiocytosis (LCH) of the bone.
Materials and methods
A retrospective review of the radiographic and MRI features of 85 histologically proven cases of skeletal LCH over a 12-year period. Clinical data recorded included age, gender and location. Radiographic features evaluated included Lodwick grading, cortical/periosteal response and matrix mineralisation. MRI features assessed included lesion size and T1-weighted signal intensity (T1W SI), nature of margin, hypointense rim, enhancement pattern, bone marrow and soft tissue oedema, soft tissue mass, fluid-fluid levels, the penumbra sign and the budding and bulging signs.
Results
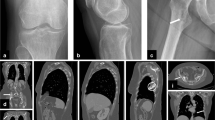
The study included 85 patients, 54 males and 31 females with mean age of 13 years (range 1–76 years). The femur was the commonest bone involved (38.8%), followed by the scapula (9.4%), clavicle (8.2%), ilium (8.2%) and ischium (8.2%). The mean maximal lesion size was 40 mm (range 16–85 mm). The commonest radiographic appearance was of a lytic lesion with no appreciable sclerotic rim, an intact expanded cortex and either absent or laminated periosteal response. MRI demonstrated a hypointense rim (41.5%), the budding (31.7%) and bulging (36.6%) signs, eccentric extra-osseous mass (42.7%), prominent bone marrow (95.3%) and soft tissue oedema (84.1%). Rarer features included haemorrhage (2.4%), the penumbra sign (3.5%) and fluid-fluid levels (2.4%). Thirteen of 25 post-contrast studies showed peripheral/rim enhancement with central necrosis.
Conclusions
LCH classically presents as a moderately aggressive lytic bone lesion on radiography, with prominent reactive bone and soft tissue oedema being a characteristic feature on MRI.
















Similar content being viewed by others
References
Howarth DM, Gilchrist GS, Mullan BP, Wiseman GA, Edmonson JH, Schomberg PJ. Langerhans cell histiocytosis: diagnosis, natural history, management, and outcome. Cancer. 1999;85:2278–90.
Demellawy DE, Young JL, Nanassy J, Chernetsova E, Nasr A. Langerhans cell histiocytosis: a comprehensive review. Pathology. 2015;47(4):294–301.
Badalian-Very G, Vergilio JA, Degar BA, MacConaill LE, Brandner B, Calicchio ML, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116(11):1919–23.
Mickelson MR, Bonfiglio M. Eosinophilic granuloma and its variations. OrthopClinNorth Am. 1977;8:933–45.
Resnick D. Lipidoses, histiocytoses, and hypenlipoproteinemias. In: Resnick D, Niwayama G, editors. Diagnosis ofbone and joint disorders. Vol 4. 2nd ed. Philadelphia: Saunders; 1988. p. 2429–39.
Huvos AG. Bone tumors. 2nd ed. Philadelphia: Saunders; 1991. p. 695–771.
Berry DH, Gresik M, Maybee D, Marcus R. Histiocytosis X in bone only. Med PediatrOncol. 1990;18:292–4.
Carstensen H, Ornvold K. The epidemiology of Langerhans cell histiocytosis in children in Denmark, 1975–1989. Med PediatrOncol. 1993;21:387–8.
Baumgartner I, von Hochstetter A, Baumert B, Luetolf U, Follath F. Langerhans’ cell histiocytosis in adults. Med PediatrOncol. 1997;28(1):9–14.
Venkatramani R, Rosenberg S, Indramohan G, Jeng M, Jubran R. An exploratory epidemiological study of Langerhans cell histiocytosis. Pediatr Blood Cancer. 2012;59(7):1324–6.
Jezierska M, Stefanowicz J, Romanowicz G, Kosiak W, Lange M. Langerhans cell histiocytosis in children - a disease with many faces. Recent advances in pathogenesis, diagnostic examinations and treatment. Postepy Dermatol Alergol. 2018;35(1):6–17.
Khung S, Budzik JF, Amzallag-Bellenger E, et al. Skeletal involvement in Langerhans cell histiocytosis. Insights Imaging. 2013;4(5):569–79.
George JC, Buckwalter KA, Cohen MD, Edwards MK, Smith RR. Langerhans cell histiocytosis of bone: MR imaging. PediatrRadiol. 1994;24(1):29–32.
Kilborn TN, The J, Goodman TR. Paediatric manifestations of Langerhans cell histiocytosis: a review of the clinical and radiological findings. Clin Radiol. 2003;58(4):269–78.
David R, Oria RA, Kumar R, Singleton EB, Lindell MM, Shirkhoda A, et al. Radiologic features of eosinophilic granuloma of bone. AJR Am J Roentgenol. 1989;153(5):1021–6.
Samet J, Weinstein J, Fayad LM. MRI and clinical features of Langerhans cell histiocytosis (LCH) in the pelvis and extremities: can LCH really look like anything? Skelet Radiol. 2016;45:607–13.
De Schepper AM, Ramon F, Van Marck E. MR imaging of eosinophilic granuloma: report of 11 cases. Skelet Radiol. 1993;22(3):163–6.
Song YS, Lee IS, Yi JH, Cho K, Kim DK, Song JW. Radiologic findings of adult pelvis and appendicular skeletal Langerhans cell histiocytosis in nine patients. Skelet Radiol. 2011;40:1421–6.
Davies AM, Pikoulas C, Griffith J. MRI of eosinophilic granuloma. Eur J Radiol. 1994;18:205–9.
McCarville MB, Chen JY, Coleman JL, Li Y, Li X, Adderson EE, et al. Distinguishing osteomyelitis from Ewing sarcoma on radiography and MRI. AJR Am J Roentgenol. 2015;205:640–51.
Henninger B, Glodny B, Rudisch A, Trieb T, Loizides A, Putzer D, et al. Ewing sarcoma versus osteomyelitis: differential diagnosis with magnetic resonance imaging. Skelet Radiol. 2013;42(8):1,097–104.
Kasalak O, Overbosch J, Adams HJA, Dammann A, Dierckx RAJO, Jutte PC, et al. Diagnostic value of MRI signs in differentiating Ewing sarcoma from osteomyelitis. Acta Radiol. 2019;60(2):204–12.
Caracciolo JT, Temple HT, Letson GD, Kransdorf MJ. A modified Lodwick-Madewell grading system for the evaluation of lytic bone lesions. AJR Am J Roentgenol. 2016;207(1):150–6.
James SL, Hughes RJ, Ali KE, Saifuddin A. MRI of bone marrow oedema associated with focal bone lesions. Clin Radiol. 2006;61(12):1003–9.
Moon TY, Lee J, Lee IS, Choi KU, Chae JM, Kim JI, et al. MRI and histopathologic classification of Langerhans cell histiocytosis. Curr Med Imaging Rev. 2009;5:14–8.
Zaveri J, La Q, Yarmish G, Neuman J. More than just Langerhans cell histiocytosis: a radiologic review of histiocytic disorders. Radiographics. 2014;34:2008–24.
Kaplan GR, Saifuddin A, Pringle JA, Noordeen MH, Mehta MH. Langerhans’ cell histiocytosis of the spine: use of MRI in guiding biopsy. Skelet Radiol. 1998;27:673–6.
Wang S, Zhang W, Na S, Zhang L, Lang Z. Langerhans cell histiocytosis of the clavicle: a case report and review of the literature. Medicine (Baltimore). 2014;93:e117.
Stull MA, Devaney KO, Kransdorf MJ. From the archives of the AFIP: Langerhans cell histiocytosis of bone. Radiographics. 1992;12:801–23.
Usui M, Matsuno T, Kobayashi M, Yagi T, Sasaki T, Ishii S. Eosinophilic granuloma of the growing epiphysis: a case report and review of the literature. Clin Orthop. 1983;176:201–5.
Stern MB, Cassidy R, Mirra J. Eosinophilic granuloma of the proximal tibial epiphysis. Clin Orthop. 1976;118:153–6.
Hindman BW, Thomas RD, Young LW, Yu L. Langerhans cell histiocytosis: unusual skeletal manifestations observed in thirty-four cases. Skelet Radiol. 1998;27:177–81.
Murphey MD, Senchak LT, Mambalam PK, Logie CI, Klassen-Fischer MK, Kransdorf MJ. From the radiologic pathology archives: Ewing sarcoma family of tumors: radiologic-pathologic correlation. Radiographics. 2013;33(3):803–31.
Lodwick GS. Radiographic diagnosis and grading of bone tumors, with comments on computer evaluation. Proc Natl Cancer Conf. 1964;5:369–80.
Ragsdale BD, Madewell JE, Sweet DE. Radiologic and pathologic analysis of solitary bone lesions Part II: Periosteal reactions. Radiol Clin N Am. 1981;19:749–83.
Rana RS, Wu JS, Eisenberg RL. Periosteal reaction. AJR AM J Roentenol. 2009;193(4):W259–72.
Resnick D, Kyriakos M, Greenway GD. Tumors and tumor like lesions of bone: imaging and pathology of specific lesions. In: Resnick D, editor. Diagnosis of bone and joint disorders. 4th ed. Philadelphia: Saunders; 2002. p. 4060–73.
Mueller DL, Grant RM, Riding MD, Coppes MJ. Cortical saucerization: an unusual imaging finding of Ewing sarcoma. AJR AM J Roentenol. 1994;163:401–3.
Reinus WR, Gilula LA. Radiology of Ewing’s sarcoma: Ewing’s sarcoma: intergroup Ewing’s sarcoma study (IESS). Radiographics. 1984;4:929–44.
Alyas F, James S, Davies A, Saifuddin A. The role of MR imaging in the diagnostic characterisation of appendicular bone tumours and tumour-like conditions. Eur Radiol. 2007;17(10):2675–86.
Mirra JM. Histiocytoses. In: Mirra JM, Picci P, Gold RH, editors. Bone tumors: clinical, radiologic, and pathologic correlations. 2nd ed. Philadelphia: Lea &Febiger; 1989. p. 1021–60. 16.
Crim JR, Mirra JM, Eckhardt JJ, Seeger LL. Widespread inflammatory response to osteobtastoma: the flare phenomenon. Radiology. 1990;177:835–6.
Beltran J, Aparisi F, Bonmati LM, Rosenberg ZS, Present D, Steiner GC. Eosinophilic granuloma: MRI manifestations. Skelet Radiol. 1993;22(3):157–61.
Kroon HM, Bloem JL, Holscher HC, Van der Woude HJ, Reijnierse M, Taminiau AH. MR imaging of edema accompanying benign and malignant bone tumors. Skelet Radiol. 1994;23:261–9.
Grimer RJ. Size matters for sarcomas. Ann R Coll Surg Engl. 2006;88(6):519.
Bloem JL, Reidsma II. Bone and soft tissue tumors of hip and pelvis. Eur J Radiol. 2012;81:3793–801.
Albadr FB, Elgamal EA, Alorainy IA, Hassan HH. Fluid-fluid level in Langerhans cell histiocytosis of the skull. Neurosciences (Riyadh). 2006;11:47–9.
Krishna Varanasi VR, Leong MY, Tan AM, Derrick Lian WQ, Teo ELHJ. Langerhans cell histiocytosis: another cause of a fluid-fluid level within an appendicular bony lesion. BJR Case Rep. 2016;2(1):20150408.
Lomoro P, Simonetti I, Vinci G, Fichera V, Tarotto L, Trovato P, et al. Secondary aneurysmal bone cyst in Langerhans cell histiocytosis: case report, literature review. Eur J Radiol Open. 2019;6:97–100.
Wu C, Li K, Hei Y, Lan P, Mu X. MR imaging features of orbital Langerhans cell Histiocytosis. BMC Ophthalmol. 2019;19:263.
Grey AC, Davies AM, Mangham DC, Grimer RJ, Ritchie DA. The ‘penumbra sign’ on T1-weighted MR imaging in subacute osteomyelitis: frequency, cause and significance. Clin Radiol. 1998;53(8):587–92.
Davies AM, Grimer R. The penumbra sign in subacute osteomyelitis. Eur Radiol. 2005;15:1268–70.
Chang WF, Hsu YC, Wu YD, Kuo CL, Huang GS. Localized Langerhans cell histiocytosis masquerading as Brodie’s abscess in a 2-year-old child: a case report. EXCLI J. 2016;18(15):33–7.
Verstraete KL, Lang P. Bone and soft tissue tumors: the role of contrast agents for MR imaging. Eur J Radiol. 2000;34(3):229–46.
Kransdorf MJ. The use of gadolinium in the MR evaluation of musculoskeletal tumors. Top Magn Reson Imaging. 1996;8(1):15–23.
Kalus S, Saifuddin A. Whole-body MRI vs bone scintigraphy in the staging of Ewing sarcoma of bone: a 12-year single-institution review. Eur Radiol. 2019;29(10):5700–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local Research and Innovation Centre of the Institute of Orthopaedics as well as the Outer North London Research Ethics Committee, with no requirement for informed patient consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, J., Rajakulasingam, R. & Saifuddin, A. Langerhans cell histiocytosis of the shoulder girdle, pelvis and extremities: a review of radiographic and MRI features in 85 cases. Skeletal Radiol 49, 1925–1937 (2020). https://doi.org/10.1007/s00256-020-03472-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03472-2