Abstract
Crohn’s disease (CD) is a chronic inflammatory condition that affects the gastrointestinal tract, particularly the ileum and colon. This disease is characterized by recurrent bouts of intestinal inflammation with subsequent bowel wall damage, including scarring (i.e., fibrosis) and abnormal smooth muscle proliferation. MR enterography, an MRI examination tailored to assess the small bowel, is a first-line diagnostic tool for diagnosing CD in children, characterization and monitoring of disease severity and extent, and assessment of disease-related complications. To date, such MRI evaluations have been mostly qualitative, which can adversely impact diagnostic performance and inter-radiologist agreement. Quantitative MRI methods have been shown to aid in the evaluation of a variety of medical conditions and have been increasingly investigated in children and adults with CD. In CD, such objective techniques have been used to assist with diagnosis, assess treatment response, and characterize bowel wall histologic abnormalities. In the current work, we will review quantitative MRI methods for detecting and measuring intestinal active inflammation (MRI-based scoring systems, T1 relaxation mapping, diffusion-weighted imaging, intra-voxel incoherent motion, mesenteric phase contrast), bowel wall damage (magnetization transfer), and motility (quantitative cine imaging) in small bowel CD, with an emphasis on the pediatric population.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) is a chronic inflammatory condition that can affect any portion of the gastrointestinal tract, but that most often involves the ileum and colon [1]. It is characterized by recurrent episodes of active inflammation and aberrant healing that can lead to scarring (i.e., fibrosis) and abnormal smooth muscle proliferation within the bowel wall [2]. Associated narrowing of the intestinal lumen can cause a variety of complications, including intestinal obstruction (i.e., strictures) and internal penetrating disease (e.g., fistulas and abscesses) [3].
MR enterography (MRE), an MRI examination tailored to assess the small bowel, is commonly a first-line diagnostic tool in children with CD and is used for diagnosis, characterization, and monitoring of disease severity and extent, and assessment of disease-related complications [4]. To date, such MRI evaluations have been mostly qualitative, which can adversely impact both diagnostic performance and inter-radiologist agreement [5, 6]. Quantitative MRI methods have been shown to aid in the evaluation of a variety of medical conditions and have been increasingly investigated in children and adults with CD [7]. In CD, such objective imaging techniques have been used to help with diagnosis, assessment of treatment response, and characterization of bowel wall histologic abnormalities.
Sakai et al. have recently summarized the use of quantitative MRI in small bowel Crohn’s disease with a primary focus on adults [8]. In the current work, we will review quantitative MRI methods for detecting and measuring intestinal active inflammation (MRI-based scoring systems, T1 relaxation mapping, diffusion-weighted imaging, intra-voxel incoherent motion, mesenteric phase contrast), bowel wall damage (magnetization transfer), and motility (quantitative cine imaging) in small bowel CD, with an emphasis on the pediatric population.
Assessment of bowel wall active inflammation
Transmural active inflammation in the bowel wall is the hallmark of untreated and undertreated CD and places affected patients at increased risk for intestinal fibrosis, abnormal smooth muscle proliferation, and stricturing and internal penetrating complications. Histologically, active inflammation is characterized by the presence of an acute inflammatory infiltrate (i.e., neutrophilic inflammation with cryptitis) and mucosal ulcerations [9]. Conventional MRE findings of intestinal active inflammation include bowel wall thickening, mural edema, restricted diffusion, and postcontrast hyperenhancement as well as peri-enteric inflammation [10]. High-quality imaging also may reveal mucosal-based defects due to ulcers [10]. Numerous quantitative MRI methods have been described for evaluating bowel wall active inflammation in CD, including MRI-based scoring systems, bowel wall T1 mapping, diffusion-weighted imaging (including intra-voxel incoherent motion [IVIM]), and measurement of mesenteric blood flow.
MRI-based scoring systems
Magnetic Resonance Index of Activity (MaRIA)
The MaRIA is perhaps the most well-known MRI-based scoring system for detecting and measuring bowel wall inflammation and relies upon bowel wall thickness, relative contrast enhancement, edema, and radiologic ulcers as inputs (Fig. 1) [11]. The exact formula used to calculate this score is presented in Table 1. This scoring system, which has been mostly investigated and validated in adults and in research settings, has been shown to strongly correlate with endoscopic findings of intestinal inflammation when using the Crohn’s Disease Endoscopic Index of Severity (CDEIS) (r= 0.83, P< 0.001) [11]. A cut-off point ≥7 has been shown to predict active inflammation with a sensitivity of 0.87 and specificity of 0.87 in adults, while a cut-off point ≥11 can predict severe disease with a sensitivity of 0.92 and specificity of 0.92 [11].
A 17-year-old female with ileal Crohn’s disease (arrows). a Coronal unenhanced T1-weighted, (b) coronal contrast-enhanced T1-weighted, (c) axial T2-weighted single-shot fast spin-echo (SSFSE), and (d) axial T2-weighted SSFSE with fat saturation MRI images can be used to calculate the Magnetic Resonance Index of Activity (MaRIA). Components of the MaRIA score include the degree of bowel wall thickening, presence of bowel wall edema, degree of bowel wall postcontrast hyperenhancement, and presence of radiologic ulcers (all of which are present in this patient)
In children with CD, MaRIA scores have been shown to moderately correlate with the Simplified Endoscopic Score for Crohn’s Disease (SES-CD) (r = 0.68, P < 0.005) and have good inter-reader agreement (intraclass correlation coefficient [ICC] = 0.81, P < 0.001) [12]. Another pediatric study also demonstrated that the MaRIA score correlated with the SES-CD (r = 0.70, P = 0.001) [13]. Similar to those in adults, primary drawbacks of the MaRIA are its need for intravenous gadolinium chelate contrast material and the complexity of the formula used to calculate the score in the clinical setting.
Simplified Magnetic Resonance Index of Activity (sMaRIA)
More recently, Ordás et al. developed and validated a simplified MaRIA (sMaRIA) MRI-based scoring system (Table 1) that has also been shown to correlate with both the CDEIS (r = 0.83, P < 0.001) and original MaRIA (r = 0.93, P < 0.001) [14]. This scoring system, which does not require intravenous gadolinium chelate contrast material, is semi-quantitative ranging from 0 to 5 and allocates one-point each based on the presence of bowel wall thickening (> 3 mm), bowel wall edema, and peri-enteric inflammation; two-points are allocated for the presence of radiologic ulcers (Fig. 2) [14]. In adults, an sMaRIA score ≥ 1 has been shown to accurately detect active inflammation (sensitivity of 0.90 and specificity of 0.81), and a score ≥ 2 has been shown to accurately detect severe endoscopic disease accurate (sensitivity of 0.85 and specificity of 0.92) [14].
An 11-year-old male with ileal Crohn’s disease (arrows). a Coronal T2-weighted single-shot fast spin-echo (SSFSE), (b) axial T2-weighted SSFSE, and (c) axial T2-weighted SSFSE with fat saturation MR images show bowel wall thickening, intramural edema, and radiologic ulcers, yielding an simplified Magnetic Resonance Index of Activity (sMaRIA) score of 4/5. There is no peri-enteric edema
In children with CD, substantial inter-reader agreement has been observed when using the sMaRIA (four readers: κ = 0.65, ICC = 0.71; P < 0.001 for both), and scores have been shown to correlate with the weighted pediatric Crohn’s disease activity index (wPCDAI) (ρ = 0.46, P < 0.001) and C-reactive protein (CRP) (ρ = 0.48; P < 0.001) [15]. sMaRIA scores also have been shown to significantly decrease within 6 months of starting medical therapy for CD, and they have been associated with the need for surgery in pediatric patients upon multivariable modeling [16]. Another study in children with CD concluded that the sMaRIA is accurate in reflecting disease activity in the terminal ileum but not in the colon [17].
Pediatric Inflammatory Crohn’s Magnetic Resonance Enterography Index (PICMI)
Focht et al. developed the Pediatric Inflammatory Crohn’s Magnetic Resonance Enterography Index (PICMI) as part of the multi-national ImageKids study. Like the sMaRIA, this MRI-based scoring system does not require intravenous gadolinium chelate contrast material [18]. Using a multivariable approach guided by experts in the field, five items were included in the final index, including wall thickness (scored if ≥ 3 mm), restricted diffusion, radiologic ulcers, mesenteric edema, and comb sign (i.e., mesenteric vascular engorgement) [18]. The exact formula used to calculate this score is presented in Table 1.
The PICMI score has been shown to correlate with the radiologist global assessment of inflammation (r = 0.85; P < 0.001) as well as the SES-CD (r = 0.63; P < 0.001) in children [18]. This scoring system also has satisfactory inter-reader agreement (ICC = 0.84, P < 0.001). Transmural healing, defined as PICMI ≤ 10, and therapy response, defined as a change of > 20 points, have demonstrated excellent discriminative validity (areas under the receiver operating characteristic curve = 0.92–0.97). Not surprisingly, PICMI scores highly correlate with sMaRIA scores as bowel wall thickness, radiologic ulcers, and peri-enteric inflammation are included in both indices.
Bowel wall T1 relaxation mapping
MRI T1, or longitudinal, relaxation times are specific for a given tissue and have been shown to change with disease. These estimates have been shown to be impacted by inflammation, fibrosis, fat, edema, and iron deposition. Tissue T1 measurements have been used to detect inflammation and fibrosis in the heart and liver [19, 20]. There are few studies assessing noncontrast, or “native,” T1 relaxation estimates of the bowel wall in children or adults with CD (Fig. 3) [21, 22]. A study by Horsthuis et al. evaluated bowel wall T1 estimates, before and after intravenous gadolinium chelate injection [21].
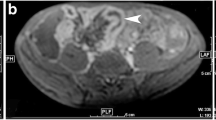
A 12-year-old female with Crohn’s disease. a Axial T2-weighted single-shot fast spin-echo MR image shows ileal wall thickening, intramural edema, and radiologic ulcers (arrow). b Axial T1 relaxation parametric map shows a region of interest (white circle) within the wall of the inflamed bowel (T1 = 1,361 ms) (arrow). Median bowel wall T1 relaxation time (ms) has been reported to be 1,159 (interquartile range 953 to 1,253) in healthy controls at 1.5-T [22]
Mahalingam et al. demonstrated that bowel wall T1 relaxation estimates are higher in children with newly diagnosed ileal CD patients (median 1,302 ms) when compared to healthy control subjects (median 1,159 ms, P < 0.001) [22]. These authors also showed that these measurements decrease in response to medical therapy (P = 0.001), and that they correlate with clinical inflammatory markers, including C-reactive protein and the weighted Pediatric Crohn’s Disease Activity Index [22]. These authors used a modified Look-Locker inversion recovery pulse sequence (5 s(3 s)3 s implementation requiring an 11-s breath-hold) with imaging performed through the most inflamed segment of terminal ileum [22].
Bowel wall diffusion-weighted imaging (DWI)
Diffusion-weighted imaging (DWI) creates a signal based on impeded diffusion of water molecules in body tissues [23]. DWI images are most often qualitatively assessed by radiologists to identify hyperintense bowel loops, an imaging feature of active inflammation (Fig. 4). Such a subjective evaluation is supported by numerous published studies [24] and is commonly included in routine clinical pediatric and adult MRE protocols [10]. The degree of impeded, or restricted, diffusion can be quantified using apparent diffusion coefficients (i.e., ADC values).
A 14-year-old male with ileal Crohn’s disease. a Axial low b-value (b = 0 s/mm2) diffusion-weighted MR image shows wall thickening of the terminal ileum (arrows). b Axial high b-value (b = 800 s/mm2) diffusion-weighted MR image shows restricted diffusion of water within the terminal ileum suggestive of active inflammation (arrows). This portion of the bowel appeared hypointense on the corresponding apparent diffusion coefficient (ADC) image
A recent meta-analysis by Kim et al. which involved nine studies that included pediatric patients with inflammatory bowel disease reported a sensitivity and specificity of DWI-MRE of 0.93 and 0.95, respectively [25]. In another pediatric cohort, Dillman et al. demonstrated that bowel wall ADC values increase over time after patients were treated with anti-tumor necrosis factor-alpha medical therapy [26]. Adding DWI to conventional MRE protocols also has been shown to improve diagnostic accuracy when evaluating children with CD [27].
A modified version of the original MaRIA score that replaces relative contrast enhancement with DWI ADC values is known as the Clermont score and does not require intravenous gadolinium chelate contrast material (Table 1) [28]. This scoring system has been shown to have good inter-observer agreement and to highly correlate with MaRIA scores when assessing the small bowel [29]. A small study in children demonstrated a moderate correlation with the SES-CD (r = 0.68) and good inter-reader agreement (ICC = 0.77) [12].
Intra-voxel incoherent motion (IVIM)
The biexponential intra-voxel incoherent motion (IVIM) approach to modeling DWI data has been proposed as an alternative to the monoexponential approach that yields ADC values. This more advanced model provides three separate quantitative parameters that reflect water diffusivity (D, analogous to ADC), blood flow in the microvasculature (D*), and microvascular blood volume, or perfusion fraction (f) from multi-b-value DWI data (Fig. 5) [30]. Alves et al. reported that IVIM D (P < 0.001), D* (P = 0.004), and f (P = 0.001) measurements were all lower in children with newly diagnosed ileal CD than in healthy control subjects [31]. The IVIM f (P = 0.016) and D* (P = 0.047) measurements both increased in response to medical therapy, while there was no significant change in IVIM D measurements (P = 0.10) [31]. These results suggest that more severely inflamed bowel may be relatively hypoperfused at the microvascular level (demonstrating both decreased blood volume and blood flow), a finding that has been suggested in previous pathology-based studies [32, 33].
A 12-year-old female with ileal Crohn’s disease. Multiple diffusion-weighted MR images were acquired for intra-voxel incoherent motion (IVIM) assessment. a-h Normal bowel loops show progressive loss of signal intensity on eight diffusion-weighted images with increasing b-values (from 0 s/mm2 to 800 s/mm2). The terminal ileum appears relatively hyperintense on all eight images (arrows). Change in terminal ileal signal intensity vs. b-value was fit using a biexponential model to obtain the IVIM parameters f (microcirculation blood volume), D* (pseudodiffusion coefficient associated with microcirculation blood flow), and D (pure diffusion coefficient)
Measurement of mesenteric blood flow
Mesenteric arterial and venous blood flow commonly increase in the setting of intestinal inflammation. This can be subjectively detected based on increased conspicuity of mesenteric vasculature adjacent to the bowel wall (i.e., the “comb sign”) [34] and bowel wall hyperenhancement on postcontrast imaging, especially early phase imaging. Abu Ata et al. objectively showed that both superior mesenteric arterial and venous blood flow are increased in the setting of small bowel CD using velocity-encoded phase-contrast MRI [35]. This technique uses bipolar gradients to encode phase shifts that are proportional to the proton velocity (Fig. 6) [36] and has been used to successfully quantify arterial and venous blood flow in other areas of the body, such as the cardiovascular system.
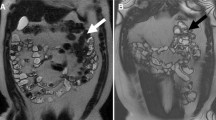
A 12-year-old male with Crohn’s disease. a Axial T2-weighted single-shot fast spin-echo (SSFSE) MR image shows ileal wall thickening (arrow). b Axial SSFSE through the level of the root of the small bowel mesentery shows the superior mesenteric artery and vein in cross-section (arrows). This anatomic level was used for phase-contrast imaging. c Axial velocity-encoded phase-contrast MRI image shows signal in the superior mesenteric artery and vein (long arrows) as well as in the abdominal aorta and inferior vena cava (short arrows). Blood flowing inferiorly is hypointense, while blood flowing superiorly is hyperintense
Abu Ata et al. hypothesized that inflamed ileum supplied and drained by ileal and ileocolic mesenteric vessels would increase both superior mesenteric arterial and venous blood flow in the root of the small bowel mesentery when normalized to abdominal aortic blood flow [35]. Their study showed that both superior mesenteric artery and superior mesenteric vein blood flow are increased in children with small bowel CD compared to healthy control subjects (P = 0.003 and P = 0.002, respectively) [35]. Furthermore, blood flow in both vessels significantly decreased by 6 weeks into medical therapy [35]. While these initial results are promising, more studies are needed to determine the clinical value of this quantitative technique for diagnosing and monitoring children and adults with small bowel CD.
Assessment of bowel wall fibrosis
Bowel wall fibrosis occurs in patients with CD due to persistent or recurrent bouts of active inflammation with abnormal healing. This aberrant healing process is characterized by excess mural collagen and extracellular matrix that are primarily deposited in the submucosal layer of the bowel [2]. This deposition of scar tissue commonly co-exists with abnormally increased smooth muscle in the bowel wall. The literature suggests that fibrogenesis, once initiated, may continue in the absence of active inflammation [2]. Currently, there are no anti-fibrotic medications approved for use in CD in the United States. Consequently, patients with CD with substantial bowel wall fibrosis are typically managed with surgical intestinal resection, surgical stricturoplasty, or endoscopic dilation [37].
Histologic bowel wall fibrosis and active inflammation commonly co-exist. Thus, substantial bowel wall fibrosis can be present even when MRE shows findings of intestinal active inflammation, such as postcontrast hyperenhancement and restricted diffusion. Qualitative MRE findings that have been associated with the presence of bowel wall fibrosis include decreased signal intensity on T2-weighted imaging, delayed postcontrast hyperenhancement, and prestenotic dilation of the bowel > 3–4 cm [38, 39]. These features are assessed in a mostly qualitative manner when used in the clinic and are likely insensitive to early (i.e., mild and moderate) fibrosis. Most recently, the more objective stricture ratio, the ratio of maximum upstream lumen diameter to minimum lumen diameter, has also been shown to correlate with the need for bowel resection in children with stricturing ileal CD [40].
Prior studies in animal models and adults have shown an association between bowel wall fibrosis and magnetization transfer ratio (MTR) measurements [41,42,43]. It is hypothesized that macromolecules in the bowel wall related to fibrosis such as collagen and extracellular matrix proteins lose signal with the application of an off-resonance magnetization transfer radiofrequency saturation pulse (Fig. 7) [44]. Greater loss of bowel wall signal can also likely be due to abnormally increased smooth muscle [45]. An adult study by Li et al. showed that bowel wall MTR normalized to skeletal muscle strongly correlated with histologic fibrosis scores (r = 0.77) [42]. These authors identified significant differences seen between nonfibrotic and mildly, moderately, and severely fibrotic bowel walls (P < 0.001) [42]. MTR measurements had an area under the receiver operating characteristic curve of 0.92 for differentiating moderately and severely fibrotic bowel walls from nonfibrotic and mildly fibrotic bowel walls [42]. In a recent mixed pediatric and adult study of 50 patients with CD undergoing small bowel resection and 83 patients with nonsurgical CD, normalized MTR was determined to be an independent predictor of the need for surgery when adjusted for other MRI features and clinical severity (OR = 1.07; P = 0.007) [16].
A 12-year-old female with Crohn’s disease. a Axial magnetization transfer (MT) MR image without an off-resonance radiofrequency (RF) pulse shows that the ileal wall is hyperintense (arrow). b Axial MR image with an off-resonance RF pulse shows loss of signal intensity in the bowel wall (arrow), presumably due to the presence of macromolecules. Regions of interest (white circles) were placed in the bowel wall on both sequences to calculate the MT ratio (45% for this patient)
Assessment of intestinal motility
Bowel segments affected by patients with CD show altered peristalsis [46]. Abnormal motility may be due to inflammation and/or fibrosis and can change over time with disease progression or treatment response. Several studies evaluating bowel motility in patients with CD have been performed to date, mostly in adult populations [47,48,49]. Cine MRI is most often evaluated in a subjective manner in the clinic. Specifically, the “frozen bowel sign” is commonly used to identify segments of bowel affected by CD and can be helpful for further characterizing bowel segments that are equivocally abnormal on other non-cine sequences [46].
Cine MRI of the bowel also can be evaluated using quantitative methods (Fig. 8). In a prospective study by Dillman et al., cine MRI was analyzed using voxel-based deformation field mapping in children with newly diagnosed ileal CD [50]. In that study, patients with CD were found to have decreased intestinal motility compared to healthy control subjects when normalized to motility measurements from fluid-filled, more proximal normal appearing bowel loops [50]. In addition, intestinal motility was shown to increase over time in response to medical therapy [50]. In their study, dynamic cine imaging was performed using a coronal 2D balanced steady-state free precession sequence at six to eight slice locations, including through the terminal ileum [50]. A US FDA-cleared tool (GIQuant; Motilent; London, UK) was used to process the images and measure intestinal motility. This tool had been previously validated and creates parametric motility maps based on deformation fields. Cococcioni et al. also quantitatively evaluated cine MRI in 25 children with CD or unclassified inflammatory bowel disease and showed that terminal ileal motility was lower in active disease and decreased with increasing histologic abnormalities [51].
A 12-year-old female with Crohn’s disease. a Coronal two-dimensional balanced steady-state free precession MR image from a cine imaging sequence shows regions of interest encircling the terminal ileum (long arrows) and more proximal normal small bowel (short arrows). b Parametric map of intestinal motility shows that the terminal ileum (long arrows) has decreased peristalsis compared to more proximal bowel loops (short arrows) (blue is indicative of relatively little voxel motion compared to red and yellow which are indicative of relatively greater voxel motion)
While all of the above quantitative methods show promise for diagnosing and/or assessing treatment response, most techniques require further validation, particularly in children. In general, there is a current lack of pediatric-specific normative data as well as few studies assessing repeatability and reproducibility data. Additional work also is needed to understand the value of these methods (i.e., how they improve outcomes and/or lower healthcare costs), particularly when compared to standard of care diagnostic methods. Table 2 summarizes all the techniques listed in this review along with their advantages and disadvantages.
Conclusion
In conclusion, numerous MRI techniques can be used to objectively assess intestinal inflammation, bowel wall damage, and motility in children with small bowel CD. Several of these quantitative methods are based on sequences that are routinely acquired in the clinic and that are presently evaluated in a qualitative manner. At present, there is a need to better understand the appropriate use of such quantitative assessments, their multiparametric performance, and how they impact meaningful patient outcomes in order to increase their use in the clinic.
Data availability
Our manuscript has no associated data since it is a review article.
References
Day AS, Ledder O, Leach ST, Lemberg DA (2012) Crohn’s and colitis in children and adolescents. World J Gastroenterol 18:5862–5869
Li C, Kuemmerle JF (2014) Mechanisms that mediate the development of fibrosis in patients with Crohn’s disease. Inflamm Bowel Dis 20:1250–1258
Orscheln ES, Dillman JR, Towbin AJ et al (2018) Penetrating Crohn disease: does it occur in the absence of stricturing disease? Abdom Radiol (NY) 43:1583–1589
Mollard BJ, Smith EA, Dillman JR (2015) Pediatric MR enterography: technique and approach to interpretation-how we do it. Radiology 274:29–43
Rees MA, Dillman JR, Anton CG et al (2019) Inter-radiologist agreement using Society of Abdominal Radiology-American Gastroenterological Association (SAR-AGA) consensus nomenclature for reporting CT and MR enterography in children and young adults with small bowel Crohn disease. Abdom Radiol (NY) 44:391–397
Dane B, Qian K, Gauvin S et al (2021) Inter-reader agreement of the Society of Abdominal Radiology-American Gastroenterological Association (SAR-AGA) consensus reporting for key phenotypes at MR enterography in adults with Crohn disease: impact of radiologist experience. Abdom Radiol (NY) 46:5095–5104
Bane O, Gee MS, Menys A et al (2021) Emerging imaging biomarkers in Crohn disease. Top Magn Reson Imaging 30:31–41
Sakai NS, Bray TJP, Taylor SA (2024) Quantitative magnetic resonance imaging (qMRI) of the small bowel in Crohn’s disease: state-of-the-art and future directions. J Magn Reson Imaging. https://doi.org/10.1002/jmri.29511
Feuerstein JD, Cheifetz AS (2017) Crohn disease: epidemiology, diagnosis, and management. Mayo Clin Proc 92:1088–1103
Guglielmo FF, Anupindi SA, Fletcher JG et al (2020) Small bowel Crohn disease at CT and MR enterography: imaging atlas and glossary of terms. Radiographics 40:354–375
Rimola J, Ordás I, Rodriguez S et al (2011) Magnetic resonance imaging for evaluation of Crohn’s disease: validation of parameters of severity and quantitative index of activity. Inflamm Bowel Dis 17:1759–1768
Gladkikh M, Benchimol EI, Mack DR et al (2023) MR enterography scores correlate with degree of mucosal healing in pediatric Crohn’s disease: a pilot study. J Can Assoc Gastroenterol 6:125–130
Pomerri F, Al Bunni F, Zuliani M et al (2017) Assessing pediatric ileocolonic Crohn’s disease activity based on global MR enterography scores. Eur Radiol 27:1044–1051
Ordás I, Rimola J, Alfaro I et al (2019) Development and validation of a simplified Magnetic Resonance Index of activity for Crohn’s disease. Gastroenterology 157:432-439.e431
Dillman JR, Ata NA, Towbin AJ et al (2023) The simplified MR Index of activity score in pediatric small-bowel Crohn disease: an interreader agreement and responsiveness study. Am J Roentgenol 220:126–133
Dillman JR, Tkach JA, Fletcher JG et al (2024) MRI and blood-based biomarkers are associated with surgery in children and adults with ileal Crohn’s disease. Inflamm Bowel Dis. https://doi.org/10.1093/ibd/izae101
Lepus CA, Moote DJ, Bao S et al (2022) Simplified Magnetic Resonance Index of activity is useful for terminal ileal but not colonic disease in pediatric Crohn disease. J Pediatr Gastroenterol Nutr 74:610–616
Focht G, Cytter-Kuint R, Greer MC et al (2022) Development, validation, and evaluation of the pediatric inflammatory Crohn’s Magnetic Resonance Enterography Index from the ImageKids study. Gastroenterology 163:1306–1320
Haaf P, Garg P, Messroghli DR et al (2016) Cardiac T1 mapping and extracellular volume (ECV) in clinical practice: a comprehensive review. J Cardiovasc Magn Reson 18:89
Pavlides M, Banerjee R, Sellwood J et al (2016) Multiparametric magnetic resonance imaging predicts clinical outcomes in patients with chronic liver disease. J Hepatol 64:308–315
Horsthuis K, Nederveen AJ, de Feiter MW et al (2009) Mapping of T1-values and gadolinium-concentrations in MRI as indicator of disease activity in luminal Crohn’s disease: a feasibility study. J Magn Reson Imaging 29:488–493
Mahalingam N, Tkach JA, Denson LA, Dillman JR (2022) Bowel wall MRI T1 relaxation estimates for assessment of intestinal inflammation in pediatric Crohn’s disease. Abdom Radiol (NY) 47:2730–2738
Bammer R (2003) Basic principles of diffusion-weighted imaging. Eur J Radiol 45:169–184
Chavhan GB, Caro-Dominguez P (2016) Diffusion-weighted imaging in pediatric body magnetic resonance imaging. Pediatr Radiol 46:847–857
Kim PH, Yoon HM, Jung AY et al (2022) Diagnostic performance of diffusion-weighted imaging for evaluation of bowel inflammation in paediatric inflammatory bowel disease: a systematic review and meta-analysis. J Crohns Colitis 16:68–78
Dillman JR, Smith EA, Sanchez R et al (2016) DWI in pediatric small-bowel Crohn disease: are apparent diffusion coefficients surrogates for disease activity in patients receiving infliximab therapy? AJR Am J Roentgenol 207:1002–1008
Shenoy-Bhangle AS, Nimkin K, Aranson T, Gee MS (2016) Value of diffusion-weighted imaging when added to magnetic resonance enterographic evaluation of Crohn disease in children. Pediatr Radiol 46:34–42
Buisson A, Joubert A, Montoriol PF et al (2013) Diffusion-weighted magnetic resonance imaging for detecting and assessing ileal inflammation in Crohn’s disease. Aliment Pharmacol Ther 37:537–545
Puylaert CAJ, Nolthenius CJT, Tielbeek JAW et al (2019) Comparison of MRI activity scoring systems and features for the terminal ileum in patients with Crohn disease. AJR Am J Roentgenol 212:W25-w31
Koh D-M, Collins DJ, Orton MR (2011) Intravoxel incoherent motion in body diffusion-weighted MRI: reality and challenges. Am J Roentgenol 196:1351–1361
Alves VdPV, Mahalingam N, Tkach JA et al (2024) Prospective characterization of intestinal MRI intravoxel incoherent motion in pediatric and young adult patients with newly diagnosed small bowel Crohn’s disease. Abdom Radiol. https://doi.org/10.1007/s00261-024-04318-4
Higashijima J, Kono T, Shimada M et al (2021) Intestinal hypoperfusion in patients with Crohn’s disease revealed by intraoperative indocyanine green fluorescence imaging. Ann Med Surg (Lond) 66:102402
Carr ND, Pullan BR, Schofield PF (1986) Microvascular studies in non-specific inflammatory bowel disease. Gut 27:542–549
Madureira AJ (2004) The comb sign. Radiology 230:783–784
Ata NA, Dillman JR, Gandhi D et al (2022) Velocity-encoded phase-contrast MRI for measuring mesenteric blood flow in patients with newly diagnosed small-bowel Crohn disease. AJR Am J Roentgenol 219:132–141
Wymer DT, Patel KP, Burke WF III, Bhatia VK (2020) Phase-contrast MRI: physics, techniques, and clinical applications. Radiographics 40:122–140
Gionchetti P, Dignass A, Danese S et al (2017) 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 2: Surgical management and special situations. J Crohns Colitis 11:135–149
Rimola J, Planell N, Rodríguez S et al (2015) Characterization of inflammation and fibrosis in Crohn’s disease lesions by magnetic resonance imaging. Am J Gastroenterol 110:432–440
Barkmeier DT, Dillman JR, Al-Hawary M et al (2016) MR enterography-histology comparison in resected pediatric small bowel Crohn disease strictures: can imaging predict fibrosis? Pediatr Radiol 46:498–507
Debnath P, Epstein KN, Kocaoglu M et al (2024) Imaging and clinical predictors of surgery in stricturing ileal Crohn’s disease: a retrospective study from a large pediatric hospital. Abdom Radiol (NY). https://doi.org/10.1007/s00261-024-04314-8
Dillman JR, Swanson SD, Johnson LA et al (2015) Comparison of noncontrast MRI magnetization transfer and T2 -weighted signal intensity ratios for detection of bowel wall fibrosis in a Crohn’s disease animal model. J Magn Reson Imaging 42:801–810
Li XH, Mao R, Huang SY et al (2018) Characterization of degree of intestinal fibrosis in patients with Crohn disease by using magnetization transfer MR imaging. Radiology 287:494–503
Adler J, Swanson SD, Schmiedlin-Ren P et al (2011) Magnetization transfer helps detect intestinal fibrosis in an animal model of Crohn disease. Radiology 259:127–135
Balaban RS, Ceckler TL (1992) Magnetization transfer contrast in magnetic resonance imaging. Magn Reson Q 8:116–137
Henkelman RM, Stanisz GJ, Graham SJ (2001) Magnetization transfer in MRI: a review. NMR Biomed 14:57–64
Guglielmo FF, Mitchell DG, O’Kane PL et al (2015) Identifying decreased peristalsis of abnormal small bowel segments in Crohn’s disease using cine MR enterography: the frozen bowel sign. Abdom Imaging 40:1150–1156
Menys A, Makanyanga J, Plumb A et al (2016) Aberrant motility in unaffected small bowel is linked to inflammatory burden and patient symptoms in Crohn’s disease. Inflamm Bowel Dis 22:424–432
Odille F, Menys A, Ahmed A et al (2012) Quantitative assessment of small bowel motility by nonrigid registration of dynamic MR images. Magn Reson Med 68:783–793
Menys A, Atkinson D, Odille F et al (2012) Quantified terminal ileal motility during MR enterography as a potential biomarker of Crohn’s disease activity: a preliminary study. Eur Radiol 22:2494–2501
Dillman JR, Tkach JA, Imbus R et al (2022) MRI-based characterization of intestinal motility in children and young adults with newly diagnosed ileal Crohn disease treated by biologic therapy: a controlled prospective study. AJR Am J Roentgenol 219:655–664
Cococcioni L, Fitzke H, Menys A et al (2021) Quantitative assessment of terminal ileum motility on MR enterography in Crohn disease: a feasibility study in children. Eur Radiol 31:775–784
Author information
Authors and Affiliations
Contributions
Dr Debnath was involved in conceptualization, data acquisition, data analysis, and manuscript writing process.
Dr Dillman was involved in conceptualization, data acquisition, data analysis, and manuscript writing process.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Debnath has no declarations of interest.
Dr. Dillman has received research support from Motilent, Perspectum, Philips Healthcare, GE HealthCare, and Bracco Imaging and is currently serving on the Pediatric Radiology Editorial Board for Uroradiology. No support was received for the current work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Debnath, P., Dillman, J.R. Quantitative MRI in children with Crohn’s disease – where do we stand?. Pediatr Radiol (2024). https://doi.org/10.1007/s00247-024-06033-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00247-024-06033-0