Abstract
Background
The utilization of 3-T magnetic field strength in obstetric imaging is increasingly common. It is important to ensure that magnetic resonance (MR) imaging with higher magnetic field strength is safe for the fetus. Comparison of neurodevelopmental outcome in neonates undergoing prenatal MR imaging with 1.5-T versus 3-T is of interest but has not yet been examined.
Objective
We hypothesized no clinically meaningful difference in neurodevelopmental outcome between fetuses undergoing 1.5-T versus 3-T fetal MR imaging. As imaging a normal fetus for research purposes is illegal in Pennsylvania, this study was conducted in a population of fetuses with left congenital diaphragmatic hernia (left-CDH).
Materials and methods
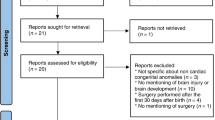
A retrospective review of neurodevelopmental outcome of fetuses with left-CDH scanned at 1.5-T (n=75) versus 3-T (n=25) magnetic field strength between July of 2012 and December of 2019 was performed. Neurodevelopmental outcomes were assessed using the Bayley Scales of Infant Development, 3rd Edition (BSID-III).
Results
There were no statistical differences in median age of assessment (1.5-T: 18 [12, 25] versus 3-T: 21 [11, 26], P=0.79), in mean BSID-III cognitive (1.5-T: 91 ± 14 versus 3-T: 90 ± 16, P=0.82), language (1.5-T: 92 ± 20 versus 3-T: 91 ± 20, P=0.91), and motor composite (1.5-T: 89 ± 15 versus 3-T: 87 ± 18, P=0.59) scores, subscales scores (for all, P>0.50), or in risk of abnormal neuromuscular exam (P=0.29) between neonates with left-CDH undergoing a 1.5-T versus 3-T MR imaging during fetal life. Additionally, the distribution of patients with average, mildly delayed, and severely delayed BSID-III scores was similar between the two groups (for all, P>0.50). The overall distribution of the composite scores in this CDH population was similar to the general population independent of exposure to 1.5-T or 3-T fetal MR imaging. Two 3-T patients (8%) and five 1.5-T patients (7%) scored within the significant delayed range for all BSID-III domains. Subjects with lower observed-to-expected fetal lung volume (O/E FLV) and postnatal need for ECMO had lower cognitive, language, motor, and subscales scores (for all, P<0.03) regardless of being imaged at 1.5-T versus 3-T.
Conclusion
This preliminary study suggests that, compared to 1.5-T MR imaging, fetal exposure to 3-T MR imaging does not increase the risk of neurodevelopmental impairment in fetuses with left-CDH. Additional MR imaging studies in larger CDH cohorts and other fetal populations are needed to replicate and extend the present findings.
Similar content being viewed by others
References
Victoria T, Johnson AM, Edgar JC et al (2016) Comparison between 1.5-T and 3-T MRI for fetal imaging: is there an advantage to Imaging with a higher field strength? AJR Am J Roentgenol 206:195–201
Chapman T, Alazraki AL, Eklund MJ (2018) A survey of pediatric diagnostic radiologists in North America: current practices in fetal magnetic resonance imaging. Pediatr Radiol 48:1924–1935
Chartier AL, Bouvier MJ, McPherson DR et al (2019) The safety of maternal and fetal MRI at 3 T. AJR Am J Roentgenol 213:1170–1173
Cannie MM, De Keyzer F, Van Laere S et al (2016) Potential heating effect in the gravid uterus by using 3-T MR imaging protocols: experimental study in miniature pigs. Radiology 279:754–761
Danzer E, Hedrick HL (2014) Controversies in the management of severe congenital diaphragmatic hernia. Semin Fetal Neonatal Med 19:376–384
Meyers ML, Garcia JR, Blough KL et al (2018) Fetal lung volumes by MRI: normal weekly values from 18 through 38 weeks’ gestation. AJR Am J Roentgenol 211:432–438
Victoria T, Danzer E, Adzick NS (2013) Use of ultrasound and MRI for evaluation of lung volumes in fetuses with isolated left congenital diaphragmatic hernia. Semin Pediatr Surg 22:30–36
Wild KT, Schindewolf E, Hedrick HL et al (2022) The genomics of congenital diaphragmatic hernia: a 10-year retrospective review. J Pediatr 248:108-113e102
Barrera CA, Francavilla ML, Serai SD et al (2020) Specific absorption rate and specific energy dose: comparison of 1.5-T versus 3.0-T fetal MRI. Radiology 295:664–674
Danzer E, Hedrick HL (2011) Neurodevelopmental and neurofunctional outcomes in children with congenital diaphragmatic hernia. Early Hum Dev 87:625–632
Danzer E, Gerdes M, D’Agostino JA et al (2015) Neurodevelopmental outcome at one year of age in congenital diaphragmatic hernia infants not treated with extracorporeal membrane oxygenation. J Pediatr Surg 50:898–903
Danzer E, Gerdes M, D’Agostino JA et al (2013) Preschool neurological assessment in congenital diaphragmatic hernia survivors: outcome and perinatal factors associated with neurodevelopmental impairment. Early Hum Dev 89:393–400
Danzer E, Gerdes M, D’Agostino JA et al (2013) Longitudinal neurodevelopmental and neuromotor outcome in congenital diaphragmatic hernia patients in the first 3 years of life. J Perinatol 33:893–898
Jaimes C, Delgado J, Cunnane MB et al (2019) Does 3-T fetal MRI induce adverse acoustic effects in the neonate? A preliminary study comparing postnatal auditory test performance of fetuses scanned at 1.5 and 3 T. Pediatr Radiol 49:37–45
Victoria T, Bebbington MW, Danzer E et al (2012) Use of magnetic resonance imaging in prenatal prognosis of the fetus with isolated left congenital diaphragmatic hernia. Prenat Diagn 32:715–723
Ruano R, Lazar DA, Cass DL et al (2014) Fetal lung volume and quantification of liver herniation by magnetic resonance imaging in isolated congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 43:662–669
Victoria T, Jaramillo D, Roberts TP et al (2014) Fetal magnetic resonance imaging: jumping from 1.5 to 3 tesla (preliminary experience). Pediatr Radiol 44:376–386 (quiz 373–375)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conficts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Danzer, E., Eppley, E., Edgar, J.C. et al. Effects of 1.5-T versus 3-T magnetic resonance imaging in fetuses: is there a difference in postnatal neurodevelopmental outcome? Evaluation in a fetal population with left-sided congenital diaphragmatic hernia. Pediatr Radiol 53, 1085–1091 (2023). https://doi.org/10.1007/s00247-023-05629-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05629-2