Abstract
Background
Many infants with congenital diaphragmatic hernia (CDH) show brain abnormality on postnatal brain MRI related to severity of CDH, degree of lung hypoplasia, intrathoracic liver, right diaphragmatic hernia and large diaphragmatic defect. It is not known whether these factors affect brain growth in utero in CDH.
Objective
To assess prenatal brain morphometry and abnormalities on fetal MR in congenital diaphragmatic hernia.
Materials and methods
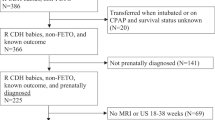
We retrospectively reviewed 109 fetal MRIs in 63 fetuses with CDH from 2009 to 2014 (27 died before discharge, 36 survived to discharge). We compared brain injury and gestational-age-corrected z-scores of brain measurements between survivors and non-survivors. We assessed correlations between brain abnormalities and CDH severity.
Results
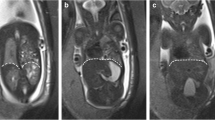
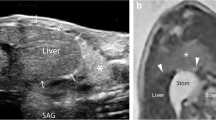
Enlarged extraaxial space was the most common abnormality, frequently seen on fetal MRI at >28 weeks of gestation, similar in survivors versus non-survivors. Anteroposterior cerebellar vermis dimension at >28 weeks of gestation was smaller in non-survivors compared to survivors (P=.02) and positively correlated with observed/expected total fetal lung volume (P=.01). Transverse cerebellar diameter at >28 weeks of gestation was also positively correlated with observed/expected total fetal lung volume (P=.04). We did not identify maturational delay, abnormal parenchymal signal or intracranial hemorrhage on fetal MRI.
Conclusion
Enlarged extraaxial spaces in the third trimester was the most common abnormality on fetal MRI in congenital diaphragmatic hernia. Cerebellar dimensions on fetal MRI are associated with CDH severity. There was no major brain parenchymal injury on fetal MRI, even in the third trimester, in CDH survivors and non-survivors.





Similar content being viewed by others
References
Radhakrishnan R, Merhar S, Meinzen-Derr J et al (2016) Correlation of MRI brain injury findings with neonatal clinical factors in infants with congenital diaphragmatic hernia. AJNR Am J Neuroradiol 37:1745–1751
Tracy S, Estroff J, Valim C et al (2010) Abnormal neuroimaging and neurodevelopmental findings in a cohort of antenatally diagnosed congenital diaphragmatic hernia survivors. J Pediatr Surg 45:958–965
Danzer E, Zarnow D, Gerdes M et al (2012) Abnormal brain development and maturation on magnetic resonance imaging in survivors of severe congenital diaphragmatic hernia. J Pediatr Surg 47:453–461
Ahmad A, Gangitano E, Odell RM et al (1999) Survival, intracranial lesions, and neurodevelopmental outcome in infants with congenital diaphragmatic hernia treated with extracorporeal membrane oxygenation. J Perinatol 19:436–440
Prayer F, Kasprian G, Gruber GM et al (2017) MR-based brain volumetry in fetuses with congenital diaphragmatic hernia. Paper presented at the 27th World Congress on Ultrasound in Obstetrics and Gynecology. Vienna, 16 Sept 2017
Limperopoulos C, Tworetzky W, McElhinney DB et al (2010) Brain volume and metabolism in fetuses with congenital heart disease: evaluation with quantitative magnetic resonance imaging and spectroscopy. Circulation 121:26–33
Owen M, Shevell M, Donofrio M et al (2014) Brain volume and neurobehavior in newborns with complex congenital heart defects. J Pediatr 164:1121–1127
Masoller N, Sanz-Cortes M, Crispi F et al (2016) Severity of fetal brain abnormalities in congenital heart disease in relation to the main expected pattern of in utero brain blood supply. Fetal Diagn Ther 39:269–278
Van Mieghem T, Gucciardo L, Done E et al (2009) Left ventricular cardiac function in fetuses with congenital diaphragmatic hernia and the effect of fetal endoscopic tracheal occlusion. Ultrasound Obstet Gynecol 34:424–429
Vogel M, McElhinney DB, Marcus E et al (2010) Significance and outcome of left heart hypoplasia in fetal congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 35:310–317
Van Mieghem T, Sandaite I, Michielsen K et al (2010) Fetal cerebral blood flow velocities in congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 36:452–457
Danzer E, Gerdes M, D'Agostino JA et al (2013) Longitudinal neurodevelopmental and neuromotor outcome in congenital diaphragmatic hernia patients in the first 3 years of life. J Perinatol 33:893–898
Kline-Fath B, Bulas D, Bahado-Singh R (eds) (2015) Fundamental and advanced fetal imaging. Wolters Kluwer Health, Philadelphia
Radhakrishnan R, Merhar SL, Su W et al (2017) Prenatal factors associated with postnatal brain injury in infants with congenital diaphragmatic hernia. AJNR Am J Neuroradiol. https://doi.org/10.3174/ajnr.A5500
Watanabe Y, Abe S, Takagi K et al (2005) Evolution of subarachnoid space in normal fetuses using magnetic resonance imaging. Prenat Diagn 25:1217–1222
Brossard-Racine M, du Plessis AJ, Vezina G et al (2014) Prevalence and spectrum of in utero structural brain abnormalities in fetuses with complex congenital heart disease. AJNR Am J Neuroradiol 35:1593–1599
Wax JR, Bookman L, Cartin A et al (2003) Mild fetal cerebral ventriculomegaly: diagnosis, clinical associations, and outcomes. Obstet Gynecol Surv 58:407–414
Barnewolt CE, Kunisaki SM, Fauza DO et al (2007) Percent predicted lung volumes as measured on fetal magnetic resonance imaging: a useful biometric parameter for risk stratification in congenital diaphragmatic hernia. J Pediatr Surg 42:193–197
Rypens F, Metens T, Rocourt N et al (2001) Fetal lung volume: estimation at MR imaging-initial results. Radiology 219:236–241
van Heijst AF, de Mol AC, Ijsselstijn H (2014) ECMO in neonates: neuroimaging findings and outcome. Semin Perinatol 38:104–113
Bulas DI, Taylor GA, O'Donnell RM et al (1996) Intracranial abnormalities in infants treated with extracorporeal membrane oxygenation: update on sonographic and CT findings. AJNR Am J Neuroradiol 17:287–294
Brunberg JA, Kewitz G, Schumacher RE (1993) Venovenous extracorporeal membrane oxygenation: early CT alterations following use in management of severe respiratory failure in neonates. AJNR Am J Neuroradiol 14:595–603
Stolar CJ, Reyes C (1988) Extracorporeal membrane oxygenation causes significant changes in intracranial pressure and carotid artery blood flow in newborn lambs. J Pediatr Surg 23:1163–1168
Wien MA, Whitehead MT, Bulas D et al (2017) Patterns of brain injury in newborns treated with extracorporeal membrane oxygenation. AJNR Am J Neuroradiol 38:820–826
Goldstein I, Reece EA, Pilu G et al (1987) Cerebellar measurements with ultrasonography in the evaluation of fetal growth and development. Am J Obstet Gynecol 156:1065–1069
Reece EA, Goldstein I, Pilu G, Hobbins JC (1987) Fetal cerebellar growth unaffected by intrauterine growth retardation: a new parameter for prenatal diagnosis. Am J Obstet Gynecol 157:632–638
Holanda-Filho JA, Souza AI, Souza AS et al (2011) Fetal transverse cerebellar diameter measured by ultrasound does not differ between genders. Arch Gynecol Obstet 284:299–302
Tarui T, Khwaja OS, Estroff JA et al (2012) Altered fetal cerebral and cerebellar development in twin-twin transfusion syndrome. AJNR Am J Neuroradiol 33:1121–1126
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Radhakrishnan, R., Merhar, S.L., Burns, P. et al. Fetal brain morphometry on prenatal magnetic resonance imaging in congenital diaphragmatic hernia. Pediatr Radiol 49, 217–223 (2019). https://doi.org/10.1007/s00247-018-4272-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4272-z