Abstract
Background
Percutaneous radiological gastrostomy tube insertion is a common procedure in children. An approach using ultrasound and fluoroscopy may not be feasible in patients with challenging anatomy; therefore, advanced techniques or other imaging modalities may be required.
Objective
To describe our experience using cone-beam computed tomography (CT)–assisted percutaneous gastrostomy insertion in pediatric patients with challenging anatomy.
Materials and methods
A retrospective review was performed in children who underwent cone-beam CT–assisted percutaneous radiologic gastrostomy between January 2015 and July 2019. Indications, technique, outcomes, complications, and radiation dose (reference-point air kerma, air kerma area product) were assessed through chart and imaging review. Descriptive statistics only were used.
Results
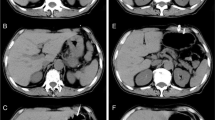
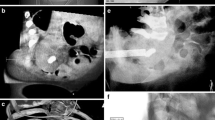
Twenty-seven procedures were attempted in 26 patients. Reasons for utilizing cone-beam CT guidance were high-positioned stomach (n = 10), interposing bowel loops and liver (n = 19), omphalocele (n = 1), severe scoliosis (n = 1), and ventriculoperitoneal shunt (n = 1). Technical success was 85% (23/27). Mean procedure time was 96 min (range 50–131 min). No safe access route into the stomach was encountered in four patients; three were referred for surgical gastrostomy and one had a successful re-attempt. Radiation dose data was obtained from 19 procedures (17 successful) with a total dose in successful procedures ranging from 8.1 to 63.6 mGy (average 26.2 mGy, median 24.9 mGy). The number of cone-beam CT acquisitions per procedure ranged from 1 to 4. Major complication frequency was 11% (3/27) (bleeding, peritonitis, and aspiration pneumonia); minor complication frequency was 3.7% (1/27).
Conclusion
This study shows that cone-beam CT guidance can be useful for assisting percutaneous radiologic gastrostomy in children with challenging anatomy.




Similar content being viewed by others
Abbreviations
- G-tube:
-
Gastrostomy tube
- PEG:
-
Percutaneous endoscopic gastrostomy
- US:
-
Ultrasound
- VP:
-
Ventriculoperitoneal
- CT:
-
Computed tomography
- NPO:
-
Nil per os
- Ka,r :
-
Reference-point air kerma
- PKA :
-
Air kerma area product
References
Baker L, Beres AL, Baird R (2015) A systematic review and meta-analysis of gastrostomy insertion techniques in children. J Pediatr Surg 50:718–725.
Möhlenbruch M, Nelles M, Thomas D et al (2010) Cone-beam computed tomography-guided percutaneous radiologic gastrostomy. Cardiovasc Intervent Radiol 33:315–320.
Connolly B, Krishnamurthy G, Amaral J (2010) Upper gastrointestinal access in children: techniques and outcomes. Tech Vasc Interv Radiol 13:222–228.
Friedman JN, Ahmed S, Connolly B et al (2004) Complications associated with image-guided gastrostomy and gastrojejunostomy tubes in children. Pediatrics 114:458–461.
Nijs ELF, Cahill AM (2010) Pediatric enteric feeding techniques: insertion, maintenance, and management of problems. Cardiovasc Intervent Radiol 33:1101–1110.
Wollman B, D’Agostino HB, Walus-Wigle JR et al (1995) Radiologic, endoscopic, and surgical gastrostomy: an institutional evaluation and meta-analysis of the literature. Radiology 197:699–704.
Rosenberg J, Amaral JG, Sklar CM et al (2008) Gastrostomy and gastrojejunostomy tube placements: outcomes in children with gastroschisis, omphalocele, and congenital diaphragmatic hernia. Radiology 248:247–253.
Kapoor BS, Esparaz A, Levitin A et al (2013) Nonvascular and portal vein applications of cone-beam computed tomography: current status. Tech Vasc Interv Radiol 16:150–160.
Kim H, Park CM, Lee SM, Goo JM (2015) C-arm cone-beam CT virtual navigation-guided percutaneous mediastinal mass biopsy: diagnostic accuracy and complications. Eur Radiol 25:3508–3517.
Perry BC, Monroe EJ, McKay T et al (2017) Pediatric percutaneous osteoid osteoma ablation: cone-beam CT with fluoroscopic overlay versus conventional CT guidance. Cardiovasc Intervent Radiol 40:1593–1599.
Tacher V, Radaelli A, Lin M, Geschwind JF (2015) How i do it: cone-beam CT during transarterial chemoembolization for liver cancer. Radiology 274:320–334.
Muthusami P, Shkumat N, Rea V et al (2017) CT reconstruction and MRI fusion of 3D rotational angiography in the evaluation of pediatric cerebrovascular lesions. Neuroradiology 59:625–633.
Cahill AM, Baskin KM, Kaye RD et al (2007) CT-guided percutaneous steroid injection for management of inflammatory arthropathy of the temporomandibular joint in children. Am J Roentgenol 188(1):182.
Wallace MJ, Kuo MD, Glaiberman C et al (2008) Three-dimensional C-arm cone-beam CT: applications in the interventional suite. J Vasc Interv Radiol 20(7):S523–S537.
Acord M, Shellikeri S, Vatsky S et al (2017) Reduced-dose C-arm computed tomography applications at a pediatric institution. Pediatr Radiol 47:1817–1824.
Parra DA, Temple M (2014) Gastrointestinal interventions in children. Pediatric interventional radiology: handbook of vascular and non-vascular interventions pp. 307–325. https://doi.org/10.1007/978-1-4419-5856-3_20
Bernhard N, McAlpine K, Moineddin R, Connolly BL (2014) Variations in blood glucose levels following gastrostomy tube insertion in a paediatric population. Pediatr Radiol 44:863–870.
Shkumat NA, Al BY, Volodina S et al (2020) Dosimetric feasibility of cone-beam CT in pediatric image-guided retrograde gastrostomy tube insertions. Can Assoc Radiol J 71:68–74.
Sacks D, McClenny TE, Cardella JF, Lewis CA (2003) Society of interventional radiology clinical practice guidelines. J Vasc Interv Radiol 14:S199-202.
Tam A, Mohamed A, Pfister M et al (2009) C-arm cone beam computed tomographic needle path overlay for fluoroscopic-guided placement of translumbar central venous catheters. Cardiovasc Intervent Radiol 32:820–824.
Angle JF (2013) Cone-beam CT: Vascular applications. Tech Vasc Interv Radiol 16:144–149.
Gottschalk A, Strotzer M, Feuerbach S et al (2007) CT-guided percutaneous gastrostomy: success rate, early and late complications. RöFo 179:387–395.
Tsukuda T, Fujita T, Ito K et al (2006) Percutaneous radiologic gastrostomy using push-type gastrostomy tubes with CT and fluoroscopic guidance. Am J Roentgenol 186:574–576.
Orth RC, Wallace MJ, Kuo MD (2008) C-arm cone-beam CT: general principles and technical considerations for use in interventional radiology. J Vasc Interv Radiol 19:814–820.
Petersen TO, Reinhardt M, Fuchs J et al (2017) Analysis of patients’ X-ray exposure in 146 percutaneous radiologic gastrostomies. RöFo 189:820–827.
Dookhoo L, Mahant S, Parra DA et al (2016) Peritonitis following percutaneous gastrostomy tube insertions in children. Pediatr Radiol 46:1444–1450.
Haber ZM, Charles HW, Gross JS et al (2017) Percutaneous radiologically guided gastrostomy tube placement: comparison of antegrade transoral and retrograde transabdominal approaches. Diagn Interv Radiol 23:55.
Kuo YC, Shlansky-Goldberg RD, Mondschein JI et al (2008) Large or small bore, push or pull: a comparison of three classes of percutaneous fluoroscopic gastrostomy catheters. J Vasc Interv Radiol. https://doi.org/10.1016/j.jvir.2007.09.027
Funaki B, Peirce R, Lorenz J et al (2001) Comparison of balloon- and mushroom-retained large-bore gastrostomy catheters. Am J Roentgenol 177:359–362.
Author information
Authors and Affiliations
Contributions
T. R. and M. G. collected and analyzed the data and wrote the first draft of the manuscript.
D. P. performed most of the procedures, was responsible for study design, participated in the data collection and in the drafting and review of the manuscript.
J. Y. participated in some procedures, collected, and analyzed data, and critically reviewed the manuscript.
N. S. performed the radiation data analyses and critically reviewed the manuscript.
B. C. performed data analysis and critically reviewed the manuscript.
All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained from the Research Ethics Board of the Hospital for Sick Children (REB # 1000058981) and was performed in accordance with the principles of the Declaration of Helsinki. Due to the retrospective nature of the study, individual consent was waived, and all the procedures being performed were part of the routine care.
Conflicts of interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rohringer, T.J., Gladkikh, M., Yodying, J. et al. Cone-beam computed tomography–assisted percutaneous gastrostomy tube insertion in children with challenging anatomy. Pediatr Radiol 53, 963–970 (2023). https://doi.org/10.1007/s00247-023-05593-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05593-x