Abstract
Background
Neonatal/infantile jaundice is relatively common, and most cases resolve spontaneously. However, in the setting of unresolved neonatal cholestasis, a prompt and accurate assessment for biliary atresia is vital to prevent poor outcomes.
Objective
To determine whether shear wave elastography (SWE) alone or combined with gray-scale imaging improves the diagnostic performance of US in discriminating biliary atresia from other causes of neonatal jaundice over that of gray-scale imaging alone.
Materials and methods
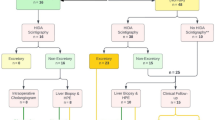
Infants referred for cholestatic jaundice were assessed with SWE and gray-scale US. On gray-scale US, two radiology readers assessed liver heterogeneity, presence of the triangular cord sign, hepatic artery size, presence/absence of common bile duct and gallbladder, and gallbladder shape; associated interobserver correlation coefficients (ICC) were calculated. SWE speeds were performed on a Siemens S3000 using 6C2 and 9 L4 transducers with both point and two-dimensional (2-D) SWE US. Both univariable and multivariable analyses were performed, as were receiver operating characteristic curves (ROC) and statistical significance tests (chi-squared, analysis of variance, t-test and Wilcoxon rank sum) when appropriate.
Results
There were 212 infants with biliary atresia and 106 without biliary atresia. The median shear wave speed (SWS) for biliary atresia cases was significantly higher (P<0.001) than for non-biliary-atresia cases for all acquisition modes. For reference, the median L9 point SWS was 2.1 m/s (interquartile range [IQR] 1.7–2.4 m/s) in infants with biliary atresia and 1.5 m/s (IQR 1.3–1.9 m/s) in infants without biliary atresia (P<0.001). All gray-scale US findings were significantly different between biliary-atresia and non-biliary-atresia cohorts (P<0.001), intraclass correlation coefficient (ICC) range 0.7–1.0. Triangular cord sign was most predictive of biliary atresia independent of other gray-scale findings or SWS — 96% specific and 88% sensitive. Multistep univariable/multivariable analysis of both gray-scale findings and SWE resulted in three groups being predictive of biliary atresia likelihood. Abnormal common bile duct/gallbladder and enlarged hepatic artery were highly predictive of biliary atresia independent of SWS (100% for girls and 95–100% for boys). Presence of both the common bile duct and the gallbladder along with a normal hepatic artery usually excluded biliary atresia independent of SWS. Other gray-scale combinations were equivocal, and including SWE improved discrimination between biliary-atresia and non-biliary-atresia cases.
Conclusion
Shear wave elastography independent of gray-scale US significantly differentiated biliary-atresia from non-biliary-atresia cases. However, gray-scale findings were more predictive of biliary atresia than elastography. SWE was useful for differentiating biliary-atresia from non-biliary-atresia cases in the setting of equivocal gray-scale findings.







Similar content being viewed by others
References
Woodgate P, Jardine LA (2015) Neonatal jaundice: phototherapy. BMJ Clin Evid 2015:0319
Nio M, Ohi R, Miyano T et al (2003) Five- and 10-year survival rates after surgery for biliary atresia: a report from the Japanese biliary atresia registry. J Pediatr Surg 38:997–1000
Altman RP, Lilly JR, Greenfeld J et al (1997) A multivariable risk factor analysis of the portoenterostomy (Kasai) procedure for biliary atresia: twenty-five years of experience from two centers. Ann Surg 226:348–355
Ryckman FC, Alonso MH, Bucuvalas JC, Balistreri WF (1998) Biliary atresia — surgical management and treatment options as they relate to outcome. Liver Transpl Surg 4:S24–S33
Haafiz AB (2010) Liver fibrosis in biliary atresia. Expert Rev Gastroenterol Hepatol 4:335–343
Shteyer E, Ramm GA, Xu C et al (2006) Outcome after portoenterostomy in biliary atresia: pivotal role of degree of liver fibrosis and intensity of stellate cell activation. J Pediatr Gastroenterol Nutr 42:93–99
Weerasooriya VS, White FV, Shepherd RW (2004) Hepatic fibrosis and survival in biliary atresia. J Pediatr 144:123–125
Hung PY, Chen CC, Chen WJ et al (2008) Long-term prognosis of patients with biliary atresia: a 25 year summary. J Pediatr Gastroenterol Nutr 42:190–195
Lee HJ, Lee SM, Park WH, Choi SO (2003) Objective criteria of triangular cord sign in biliary atresia on US scans. Radiology 229:395–400
Park WH, Choi SO, Lee HJ (1999) The ultrasonographic 'triangular cord' coupled with gallbladder images in the diagnostic prediction of biliary atresia from infantile intrahepatic cholestasis. J Pediatr Surg 34:1706–1710
Zhou L, Shan Q, Tian W et al (2016) Ultrasound for the diagnosis of biliary atresia: a meta-analysis. AJR Am J Roentgenol 206:W73–W82
Kim WS, Cheon JE, Youn BJ et al (2007) Hepatic arterial diameter measured with US: adjunct for US diagnosis of biliary atresia. Radiology 245:549–555
Zhou LY, Wang W, Shan QY et al (2015) Optimizing the US diagnosis of biliary atresia with a modified triangular cord thickness and gallbladder classification. Radiology 277:181–191
Farrant P, Meire HB, Mieli-Vergani G (2001) Improved diagnosis of extraheptic biliary atresia by high frequency ultrasound of the gall bladder. Br J Radiol 74:952–954
Bedossa P, Dargère D, Paradis V (2003) Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 38:1449–1457
Noruegas MJ, Matos H, Gonçalves I et al (2012) Acoustic radiation force impulse-imaging in the assessment of liver fibrosis in children. Pediatr Radiol 42:201–204
Barr RG, Ferraioli G, Palmeri ML et al (2015) Elastography assessment of liver fibrosis: Society of Radiologists in Ultrasound consensus conference statement. Radiology 276:845–861
Bruno C, Minniti S, Bucci A, Pozzi Mucelli R (2016) ARFI: from basic principles to clinical applications in diffuse chronic disease — a review. Insights Imaging 7:735–746
Hanquinet S, Courvoisier DS, Rougemont AL et al (2016) Acoustic radiation force impulse sonography in assessing children with biliary atresia for liver transplantation. Pediatr Radiol 46:1011–1016
Zhou LY, Jiang H, Shan QY et al (2017) Liver stiffness measurements with supersonic shear wave elastography in the diagnosis of biliary atresia: a comparative study with grey-scale US. Eur Radiol 27:3474–3484
Shin NY, Kim MJ, Lee MJ et al (2014) Transient elastography and sonography for prediction of liver fibrosis in infants with biliary atresia. J Ultrasound Med 33:853–864
Leschied JR, Dillman JR, Bilhartz J et al (2015) Shear wave elastography helps differentiate biliary atresia from other neonatal/infantile liver diseases. Pediatr Radiol 45:366–375
Wang X, Qian L, Jia L et al (2016) Utility of shear wave elastography for differentiating biliary atresia from infantile hepatitis syndrome. J Ultrasound Med 35:1475–1479
Dillman JR, DiPaola FW, Smith SJ et al (2019) Prospective assessment of ultrasound shear wave elastography for discriminating biliary atresia from other causes of neonatal cholestasis. J Pediatr 212:60–65.e3
Sun Y, Zheng S, Qian Q (2011) Ultrasonographic evaluation in the differential diagnosis of biliary atresia and infantile hepatitis syndrome. Pediatr Surg Int 27:675–679
Tan Kendrick AP, Phua KB, Ooi BC, Tan CE (2003) Biliary atresia: making the diagnosis by the gallbladder ghost triad. Pediatr Radiol 33:311–315
Batts KP, Ludwig J (1995) Chronic hepatitis. An update on terminology and reporting. Am J Surg Pathol 19:1409–1417
Goodman ZD (2007) Grading and staging systems for inflammation and fibrosis in chronic liver diseases. J Hepatol 47:598–607
Fluss R, Faraggi D, Reiser B (2005) Estimation of the Youden index and its associated cutoff point. Biom J 47:458–472
Kwatra N, Shalaby-Rana E, Narayanan S et al (2013) Phenobarbital-enhanced hepatobiliary scintigraphy in the diagnosis of biliary atresia: two decades of experience at a tertiary center. Pediatr Radiol 43:1365–1375
Rastogi A, Krishnani N, Yachha SK et al (2009) Histopathological features and accuracy for diagnosing biliary atresia by prelaparotomy liver biopsy in developing countries. J Gastroenterol Hepatol 24:97–102
Yang JG, Ma DQ, Peng Y et al (2009) Comparison of different diagnostic methods for differentiating biliary atresia from idiopathic neonatal hepatitis. Clin Imaging 33:439–446
Azar G, Beneck D, Lane B et al (2002) Atypical morphologic presentation of biliary atresia and value of serial liver biopsies. J Pediatr Gastroenterol Nutr 34:212–215
Eiler J, Kleinholdermann U, Albers D et al (2012) Standard value of ultrasound elastography using acoustic radiation force impulse imaging (ARFI) in healthy liver tissue of children and adolescents. Ultraschall Med 33:474–479
Fontanilla T, Cañas T, Macia A et al (2014) Normal values of liver shear wave speed in healthy children assessed by acoustic radiation force impulse imaging using a convex probe and a linear probe. Ultrasound Med Biol 40:470–477
Hanquinet S, Courvoisier D, Kanavaki A et al (2013) Acoustic radiation force impulse imaging — normal values of liver stiffness in healthy children. Pediatr Radiol 43:539–544
Matos H, Trindade A, Noruegas MJ (2014) Acoustic radiation force impulse imaging in paediatric patients: normal liver values. J Pediatr Gastroenterol Nutr 59:684–688
Tutar O, Beşer ÖF, Adaletli I et al (2014) Shear wave elastography in the evaluation of liver fibrosis in children. J Pediatr Gastroenterol Nutr 58:750–755
Pinto J, Matos H, Nobre S et al (2014) Comparison of acoustic radiation force impulse/serum noninvasive markers for fibrosis prediction in liver transplant. J Pediatr Gastroenterol Nutr 58:382–386
Franchi-Abella S, Corno L, Gonzales E et al (2016) Feasibility and diagnostic accuracy of supersonic shear-wave elastography for the assessment of liver stiffness and liver fibrosis in children: a pilot study of 96 patients. Radiology 278:554–562
Shima H, Igarashi G, Wakisaka M et al (2012) Noninvasive acoustic radiation force impulse (ARFI) elastography for assessing the severity of fibrosis in the post-operative patients with biliary atresia. Pediatr Surg Int 28:869–872
Danks DM, Campbell PE, Jack I et al (1977) Studies of the aetiology of neonatal hepatitis and biliary atresia. Arch Dis Child 52:360–367
Strickland AD, Shannon K (1982) Studies in the etiology of extrahepatic biliary atresia: time-space clustering. J Pediatr 100:749–753
Yoon PW, Bresee JS, Olney RS et al (1997) Epidemiology of biliary atresia: a population-based study. Pediatrics 99:376–382
Barr RG, Wilson SR, Rubens D et al (2020) Update to the Society of Radiologists in Ultrasound liver elastography consensus statement. Radiology 296:263–274
Maggiore G, Bernard O, Hadchouel M et al (1991) Diagnostic value of serum gamma-glutamyl transpeptidase activity in liver diseases in children. J Pediatr Gastroenterol Nutr 12:21–26
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors disclose support from Siemens Healthineers (Erlangen, Germany) on supplying equipment to both Stanford and research colleagues in China.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sandberg, J.K., Sun, Y., Ju, Z. et al. Ultrasound shear wave elastography: does it add value to gray-scale ultrasound imaging in differentiating biliary atresia from other causes of neonatal jaundice?. Pediatr Radiol 51, 1654–1666 (2021). https://doi.org/10.1007/s00247-021-05024-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-05024-9