Abstract
Brain contrast-enhanced ultrasound (CEUS) is an emerging application that can complement gray-scale US and yield additional insights into cerebral flow dynamics. CEUS uses intravenous injection of ultrasound contrast agents (UCAs) to highlight tissue perfusion and thus more clearly delineate cerebral pathologies including stroke, hypoxic–ischemic injury and focal lesions such as tumors and vascular malformations. It can be applied not only in infants with open fontanelles but also in older children and adults via a transtemporal window or surgically created acoustic window. Advancements in CEUS technology and post-processing methods for quantitative analysis of UCA kinetics further elucidate cerebral microcirculation. In this review article we discuss the CEUS examination protocol for brain imaging in children, current clinical applications and future directions for research and clinical uses of brain CEUS.






Similar content being viewed by others
References
Hwang M (2018) Introduction to contrast-enhanced ultrasound of the brain in neonates and infants: current understanding and future potential. Pediatr Radiol 49:254–262
Vinke EJ, Kortenbout AJ, Eyding J et al (2017) Potential of contrast-enhanced ultrasound as a bedside monitoring technique in cerebral perfusion: a systematic review. Ultrasound Med Biol 43:2751–2757
Archer LN, Levene MI, Evans DH (1986) Cerebral artery Doppler ultrasonography for prediction of outcome after perinatal asphyxia. Lancet 2:1116–1118
Hwang M, Sridharan A, Darge K et al (2019) Novel quantitative contrast-enhanced ultrasound detection of hypoxic ischemic injury in neonates and infants: pilot study 1. J Ultrasound Med 38:2025–2038
Prada F, Bene MD, Fornaro R et al (2016) Identification of residual tumor with intraoperative contrast-enhanced ultrasound during glioblastoma resection. Neurosurg Focus 40:E7
Kern R, Diels A, Pettenpohl J et al (2011) Real-time ultrasound brain perfusion imaging with analysis of microbubble replenishment in acute MCA stroke. J Cereb Blood Flow Metab 31:1716–1724
Meves SH, Wilkening W, Thies T et al (2002) Comparison between echo contrast agent-specific imaging modes and perfusion-weighted magnetic resonance imaging for the assessment of brain perfusion. Stroke 33:2433–2437
Puls I, Hauck K, Demuth K et al (1999) Diagnostic impact of cerebral transit time in the identification of microangiopathy in dementia: a transcranial ultrasound study. Stroke 30:2291–2295
Jungehulsing GJ, Brunecker P, Nolte CH et al (2008) Diagnostic transcranial ultrasound perfusion-imaging at 2.5 MHz does not affect the blood–brain barrier. Ultrasound Med Biol 34:147–150
Holscher T, Wilkening W, Draganski B et al (2005) Transcranial ultrasound brain perfusion assessment with a contrast agent-specific imaging mode: results of a two-center trial. Stroke 36:2283–2285
Hwang M, Riggs BJ, Katz J et al (2018) Advanced pediatric neurosonography techniques: contrast-enhanced ultrasonography, elastography, and beyond. J Neuroimaging 28:150–157
Christensen-Jeffries K, Couture O, Dayton PA et al (2020) Super-resolution ultrasound imaging. Ultrasound Med Biol 46:865–891
Zhang Z, Katz J, Hwang M et al (2019) Cerebral vasculars super resolution imaging and blood flow measurement using ultrasound enhanced particle tracking velocimetry. 72nd annual meeting of the APS division of fluid dynamics, Seattle
Prada F, Perin A, Martegani A et al (2014) Intraoperative contrast-enhanced ultrasound for brain tumor surgery. Neurosurgery 74:542–552
Knieling F, Ruffer A, Cesnjevar R et al (2020) Transfontanellar contrast-enhanced ultrasound for monitoring brain perfusion during neonatal heart surgery. Circ Cardiovasc Imaging 13:e010073
Hwang M, Riggs BJ, Saade-Lemus S et al (2018) Bedside contrast-enhanced ultrasound diagnosing cessation of cerebral circulation in a neonate: a novel bedside diagnostic tool. Neuroradiol J 31:578–580
Kramer MR, Bhagat N, Back SJ et al (2018) Influence of contrast-enhanced ultrasound administration setups on microbubble enhancement: a focus on pediatric applications. Pediatr Radiol 48:101–108
Eisenbrey JR, Daecher A, Kramer MR et al (2015) Effects of needle and catheter size on commercially available ultrasound contrast agents. J Ultrasound Med 34:1961–1968
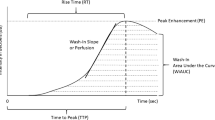
Tang MX, Mulvana H, Gauthier T et al (2011) Quantitative contrast-enhanced ultrasound imaging: a review of sources of variability. Interface Focus 1:520–539
Vinke EJ, Eyding J, de Korte CL et al (2017) Repeatability of bolus kinetics ultrasound perfusion imaging for the quantification of cerebral blood flow. Ultrasound Med Biol 43:2758–2764
Pitre-Champagnat S, Coiffier B, Jourdain L et al (2017) Toward a standardization of ultrasound scanners for dynamic contrast-enhanced ultrasonography: methodology and phantoms. Ultrasound Med Biol 43:2670–2677
Gauthier TP, Chebil M, Peronneau P et al (2012) In vitro evaluation of the impact of ultrasound scanner settings and contrast bolus volume on time-intensity curves. Ultrasonics 52:12–19
Meairs S (2008) Contrast-enhanced ultrasound perfusion imaging in acute stroke patients. Eur Neurol 59:17–26
Shen C, Xu J, Fang NX et al (2014) Anisotropic complementary acoustic metamaterial for canceling out aberrating layers. Phys Rev X 4:041033
Prada F, Del Bene M, Casali C et al (2015) Intraoperative navigated angiosonography for skull base tumor surgery. World Neurosurg 84:1699–1707
Prada F, Del Bene M, Saini M et al (2015) Intraoperative cerebral angiosonography with ultrasound contrast agents: how I do it. Acta Neurochir 157:1025–1029
Kearns KN, Sokolowski JD, Chadwell K et al (2019) The role of contrast-enhanced ultrasound in neurosurgical disease. Neurosurg Focus 47:E8
Krix M (2008) Time intensity curves. In: Baert AL (ed) Encyclopedia of diagnostic imaging. Springer, Berlin
Peronneau P, Lassau N, Leguerney I et al (2010) Contrast ultrasonography: necessity of linear data processing for the quantification of tumor vascularization. Ultraschall Med 31:370–378
Gauthier M, Leguerney I, Thalmensi J et al (2011) Estimation of intra-operator variability in perfusion parameter measurements using DCE-US. World J Radiol 3:70–81
Pitre-Champagnat S, Leguerney I, Bosq J et al (2015) Dynamic contrast-enhanced ultrasound parametric maps to evaluate intratumoral vascularization. Investig Radiol 50:212–217
Miller DL, Averkiou MA, Brayman AA et al (2008) Bioeffects considerations for diagnostic ultrasound contrast agents. J Ultrasound Med 27:611–632
Morse SV, Pouliopoulos AN, Chan TG et al (2019) Rapid short-pulse ultrasound delivers drugs uniformly across the murine blood–brain barrier with negligible disruption. Radiology 291:459–466
Kurinczuk JJ, White-Koning M, Badawi N (2010) Epidemiology of neonatal encephalopathy and hypoxic–ischaemic encephalopathy. Early Hum Dev 86:329–338
Hickey RW, Painter MJ (2006) Brain injury from cardiac arrest in children. Neurol Clin 24:147–158
Kirschen MP, Topjian AA, Berg RA (2016) Neurologic outcome after cardiac arrest: what you see at hospital discharge may or may not be what you get. Resuscitation 102:A1–A2
Sorokan ST, Jefferies AL, Miller SP (2018) Imaging the term neonatal brain. Paediatr Child Health 23:322–328
Intrapiromkul J, Northington F, Huisman TA et al (2013) Accuracy of head ultrasound for the detection of intracranial hemorrhage in preterm neonates: comparison with brain MRI and susceptibility weighted imaging. J Neuroradiol 40:81–88
Huang BY, Castillo M (2008) Hypoxic–ischemic brain injury: imaging findings from birth to adulthood. Radiographics 28:417–439
Hagmann P, Jonasson L, Maeder P et al (2006) Understanding diffusion MR imaging techniques: from scalar diffusion-weighted imaging to diffusion tensor imaging and beyond. Radiographics 26:205–223
Lally PJ, Montaldo P, Oliveira V et al (2019) Magnetic resonance spectroscopy assessment of brain injury after moderate hypothermia in neonatal encephalopathy: a prospective multicentre cohort study. Lancet Neurol 18:35–45
De Vis JB, Hendrikse J, Petersen ET et al (2015) Arterial spin-labelling perfusion MRI and outcome in neonates with hypoxic–ischemic encephalopathy. Eur Radiol 25:113–121
Massaro AN, Evangelou I, Fatemi A et al (2015) White matter tract integrity and developmental outcome in newborn infants with hypoxic–ischemic encephalopathy treated with hypothermia. Dev Med Child Neurol 57:441–448
Haller S, Zaharchuk G, Thomas DL et al (2016) Arterial spin labeling perfusion of the brain: emerging clinical applications. Radiology 281:337–356
Ouyang MH, Liu PY, Jeon T et al (2017) Heterogeneous increases of regional cerebral blood flow during preterm brain development: preliminary assessment with pseudo-continuous arterial spin labeled perfusion MRI. Neuroimage 147:233–242
Wong EC (2014) An introduction to ASL labeling techniques. J Magn Reson Imaging 40:1–10
Proisy M, Mitra S, Uria-Avellana C et al (2016) Brain perfusion imaging in neonates: an overview. AJNR Am J Neuroradiol 37:1766–1773
Busl KM, Greer DM (2010) Hypoxic–ischemic brain injury: pathophysiology, neuropathology and mechanisms. NeuroRehabilitation 26:5–13
Zheng Q, Ouyang M, Martin-Saavedra JS et al (2019) Increased brain perfusion in neonatal hypoxic ischemic injury with negative reading of DWI, T1/T2-weighted images: implications of perfusion MRI for reperfusion response monitoring and prognostication. ISMRM, Montreal
Wintermark P, Hansen A, Gregas MC et al (2011) Brain perfusion in asphyxiated newborns treated with therapeutic hypothermia. AJNR Am J Neuroradiol 32:2023–2029
Khaw K, Sridharan A, Poznick L et al (2020) Evaluating the correlation between bolus perfusion kinetics using contrast-enhanced ultrasound and intracranial pressure in a pediatric porcine model of asphyxia-associated cardiac arrest. Society for Pediatric Radiology Annual Meeting & Postgraduate Course, Miami
Mavroudis CD, Karlsson M, Ko T et al (2018) Cerebral mitochondrial dysfunction associated with deep hypothermic circulatory arrest in neonatal swine. Eur J Cardiothorac Surg 54:162–168
Lee JK, Brady KM, Chung SE et al (2014) A pilot study of cerebrovascular reactivity autoregulation after pediatric cardiac arrest. Resuscitation 85:1387–1393
Sekhon MS, Ainslie PN, Griesdale DE (2017) Clinical pathophysiology of hypoxic ischemic brain injury after cardiac arrest: a “two-hit” model. Crit Care 21:90
Kushwah S, Kumar A, Verma A et al (2017) Comparison of fractional anisotropy and apparent diffusion coefficient among hypoxic ischemic encephalopathy stages 1, 2, and 3 and with nonasphyxiated newborns in 18 areas of brain. Indian J Radiol Imaging 27:447–456
Lemmon ME, Wagner MW, Bosemani T et al (2017) Diffusion tensor imaging detects occult cerebellar injury in severe neonatal hypoxic-ischemic encephalopathy. Dev Neurosci 39:207–214
Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39:1890–1900
Reller MD, Strickland MJ, Riehle-Colarusso T et al (2008) Prevalence of congenital heart defects in metropolitan Atlanta, 1998-2005. J Pediatr 153:807–813
Centers for Disease Control and Prevention (2019) Data and statistics on congenital heart defects. CDC website. https://www.cdc.gov/ncbddd/heartdefects/data.html. Accessed 9 Dec 2020
Centers for Disease Control and Prevention (2010) Morbidity and mortality weekly report: racial differences by gestational age in neonatal deaths attributable to congenital heart defects — United States, 2003–2006. CDC website. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5937a3.htm?s_cid=mm5937a3_w. Accessed 9 Dec 2020
Licht DJ, Shera DM, Clancy RR et al (2009) Brain maturation is delayed in infants with complex congenital heart defects. J Thorac Cardiovasc Surg 137:529–536
Best KE, Rankin J (2016) Long-term survival of individuals born with congenital heart disease: a systematic review and meta-analysis. J Am Heart Assoc 5:e002846
McQuillen PS, Barkovich AJ, Hamrick SE et al (2007) Temporal and anatomic risk profile of brain injury with neonatal repair of congenital heart defects. Stroke 38:736–741
Newburger JW, Bellinger DC (2006) Brain injury in congenital heart disease. Circulation 113:183–185
Dent CL, Spaeth JP, Jones BV et al (2005) Brain magnetic resonance imaging abnormalities after the Norwood procedure using regional cerebral perfusion. J Thorac Cardiovasc Surg 130:1523–1530
Mahle WT, Tavani F, Zimmerman RA et al (2002) An MRI study of neurological injury before and after congenital heart surgery. Circulation 106:I109–I114
Lorusso R, Taccone FS, Belliato M et al (2017) Brain monitoring in adult and pediatric ECMO patients: the importance of early and late assessments. Minerva Anestesiol 83:1061–1074
Licht DJ, Wang J, Silvestre DW et al (2004) Preoperative cerebral blood flow is diminished in neonates with severe congenital heart defects. J Thorac Cardiovasc Surg 128:841–849
Zaleski KL, Kussman BD (2020) Near-infrared spectroscopy in pediatric congenital heart disease. J Cardiothorac Vasc Anesth 34:489–500
Simons J, Sood ED, Derby CD et al (2012) Predictive value of near-infrared spectroscopy on neurodevelopmental outcome after surgery for congenital heart disease in infancy. J Thorac Cardiovasc Surg 143:118–125
Khan MS, Fraser CD (2012) Neonatal brain protection in cardiac surgery and the role of intraoperative neuromonitoring. World J Pediatr Congenit Heart Surg 3:114–119
Hovels-Gurich HH (2016) Factors influencing neurodevelopment after cardiac surgery during infancy. Front Pediatr 4:137
Spaeder MC, Klugman D, Skurow-Todd K et al (2017) Perioperative near-infrared spectroscopy monitoring in neonates with congenital heart disease: relationship of cerebral tissue oxygenation index variability with neurodevelopmental outcome. Pediatr Crit Care Med 18:213–218
Andropoulos DB, Stayer SA, Diaz LK et al (2004) Neurological monitoring for congenital heart surgery. Anesth Analg 99:1365–1375
Earley CJ, Kittner SJ, Feeser BR et al (1998) Stroke in children and sickle-cell disease: Baltimore-Washington cooperative young stroke study. Neurology 51:169–176
Chung B, Wong V (2004) Pediatric stroke among Hong Kong Chinese subjects. Pediatrics 114:e206–e212
Schoenberg BS, Mellinger JF, Schoenberg DG (1978) Cerebrovascular disease in infants and children: a study of incidence, clinical features, and survival. Neurology 28:763–768
Lynch JK, Hirtz DG, DeVeber G et al (2002) Report of the National Institute of Neurological Disorders and Stroke workshop on perinatal and childhood stroke. Pediatrics 109:116–123
Lanthier S, Carmant L, David M et al (2000) Stroke in children: the coexistence of multiple risk factors predicts poor outcome. Neurology 54:371–378
deVeber GA, MacGregor D, Curtis R et al (2000) Neurologic outcome in survivors of childhood arterial ischemic stroke and sinovenous thrombosis. J Child Neurol 15:316–324
Ellis C, McGrattan K, Mauldin P, Ovbiagele B (2014) Costs of pediatric stroke care in the United States: a systematic and contemporary review. Expert Rev Pharmacoecon Outcomes Res 14:643–650
Wiesmann M, Meyer K, Albers T et al (2004) Parametric perfusion imaging with contrast-enhanced ultrasound in acute ischemic stroke. Stroke 35:508–513
Keedy AW, Fischette WS, Soares BP et al (2012) Contrast delay on perfusion CT as a predictor of new, incident infarct: a retrospective cohort study. Stroke 43:1295–1301
Ostrom QT, de Blank PM, Kruchko C et al (2015) Alex's Lemonade Stand Foundation infant and childhood primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol 16:x1–x36
Sahu RK, Das KK, Bhaisora KS et al (2015) Pediatric intramedullary spinal cord lesions: pathological spectrum and outcome of surgery. J Pediatr Neurosci 10:214–221
Kanno H, Ozawa Y, Sakata K et al (2005) Intraoperative power Doppler ultrasonography with a contrast-enhancing agent for intracranial tumors. J Neurosurg 102:295–301
Sidhu PS, Cantisani V, Dietrich CF et al (2018) The EFSUMB guidelines and recommendations for the clinical practice of contrast-enhanced ultrasound (CEUS) in non-hepatic applications: update 2017 (short version). Ultraschall Med 39:154–180
Vetrano IG, Prada F, Nataloni IF et al (2015) Discrete or diffuse intramedullary tumor? Contrast-enhanced intraoperative ultrasound in a case of intramedullary cervicothoracic hemangioblastomas mimicking a diffuse infiltrative glioma: technical note and case report. Neurosurg Focus 39:E17
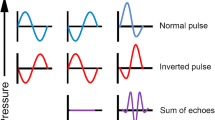
Holscher T, Ozgur B, Singel S et al (2007) Intraoperative ultrasound using phase inversion harmonic imaging: first experiences. Neurosurgery 60:382–386
Engelhardt M, Hansen C, Eyding J et al (2007) Feasibility of contrast-enhanced sonography during resection of cerebral tumours: initial results of a prospective study. Ultrasound Med Biol 33:571–575
He W, Jiang XQ, Wang S et al (2008) Intraoperative contrast-enhanced ultrasound for brain tumors. Clin Imaging 32:419–424
Mattei L, Prada F, Legnani FG et al (2016) Neurosurgical tools to extend tumor resection in hemispheric low-grade gliomas: conventional and contrast enhanced ultrasonography. Childs Nerv Syst 32:1907–1914
Prada F, Mattei L, Del Bene M et al (2014) Intraoperative cerebral glioma characterization with contrast enhanced ultrasound. Biomed Res Int 2014:484261
Vetrano IG, Prada F, Erbetta A, DiMeco F (2015) Intraoperative ultrasound and contrast-enhanced ultrasound (CEUS) features in a case of intradural extramedullary dorsal schwannoma mimicking an intramedullary lesion. Ultraschall Med 36:307–310
Prada F, Vitale V, Del Bene M et al (2017) Contrast-enhanced MR imaging versus contrast-enhanced US: a comparison in glioblastoma surgery by using intraoperative fusion imaging. Radiology 285:242–249
Cheng LG, He W, Zhang HX et al (2016) Intraoperative contrast enhanced ultrasound evaluates the grade of glioma. Biomed Res Int 2016:2643862
Aaberg KM, Gunnes N, Bakken IJ et al (2017) Incidence and prevalence of childhood epilepsy: a nationwide cohort study. Pediatrics 139:e20163908
Camfield P, Camfield C (2015) Incidence, prevalence and aetiology of seizures and epilepsy in children. Epileptic Disord 17:117–123
Fisher RS, van Emde BW, Blume W et al (2005) Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 46:470–472
Beghi E (2016) Addressing the burden of epilepsy: many unmet needs. Pharmacol Res 107:79–84
Hamandi K, Beniczky S, Diehl B et al (2017) Current practice and recommendations in UK epilepsy monitoring units. Report of a national survey and workshop. Seizure 50:92–98
Plummer C, Harvey AS, Cook M (2008) EEG source localization in focal epilepsy: where are we now? Epilepsia 49:201–218
Tewolde S, Oommen K, Lie DY et al (2015) Epileptic seizure detection and prediction based on continuous cerebral blood flow monitoring — a review. J Healthc Eng 6:159–178
Jeppesen J, Beniczky S, Johansen P et al (2015) Exploring the capability of wireless near infrared spectroscopy as a portable seizure detection device for epilepsy patients. Seizure 26:43–48
Leeman-Markowski B (2016) Review of MRI-negative epilepsy. JAMA Neurol 73:1377
Kim S, Mountz JM (2011) SPECT imaging of epilepsy: an overview and comparison with F-18 FDG PET. Int J Mol Imaging 2011:813028
Tringali G, Bono B, Dones I et al (2018) Multimodal approach for radical excision of focal cortical dysplasia by combining advanced magnetic resonance imaging data to intraoperative ultrasound, electrocorticography, and cortical stimulation: a preliminary experience. World Neurosurg 113:e738–e746
Humphreys RP, Hendrick EB, Hoffman HJ (1972) Cerebrovascular disease in children. Can Med Assoc J 107:774–776
Vanaman MJ, Hervey-Jumper SL, Maher CO (2010) Pediatric and inherited neurovascular diseases. Neurosurg Clin N Am 21:427–441
Ladner TR, Mahdi J, Attia A et al (2015) A multispecialty pediatric neurovascular conference: a model for interdisciplinary management of complex disease. Pediatr Neurol 52:165–173
Banker BQ (1961) Cerebral vascular disease in infancy and childhood. 1. Occlusive vascular diseases. J Neuropathol Exp Neurol 20:127–140
Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360:1226–1237
Acerbi F, Prada F, Vetrano IG et al (2019) Indocyanine green and contrast-enhanced ultrasound videoangiography: a synergistic approach for real-time verification of distal revascularization and aneurysm occlusion in a complex distal middle cerebral artery aneurysm. World Neurosurg 125:277–284
Prada F, Del Bene M, Mauri G et al (2018) Dynamic assessment of venous anatomy and function in neurosurgery with real-time intraoperative multimodal ultrasound: technical note. Neurosurg Focus 45:E6
Espagnet MCR, Bernardi B, Pasquini L et al (2017) Erratum to: signal intensity at unenhanced T1-weighted magnetic resonance in the globus pallidus and dentate nucleus after serial administrations of a macrocyclic gadolinium-based contrast agent in children. Pediatr Radiol 47:1366
Du J, Li FH, Fang H et al (2008) Microvascular architecture of breast lesions: evaluation with contrast-enhanced ultrasonographic micro flow imaging. J Ultrasound Med 27:833–842
Linden RA, Trabulsi EJ, Forsberg F et al (2007) Contrast enhanced ultrasound flash replenishment method for directed prostate biopsies. J Urol 178:2354–2358
Sugimoto K, Moriyasu F, Kamiyama N et al (2008) Analysis of morphological vascular changes of hepatocellular carcinoma by microflow imaging using contrast-enhanced sonography. Hepatol Res 38:790–799
Wilson SR, Jang HJ, Kim TK et al (2008) Real-time temporal maximum-intensity-projection imaging of hepatic lesions with contrast-enhanced sonography. AJR Am J Roentgenol 190:691–695
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hwang, M., Barnewolt, C.E., Jüngert, J. et al. Contrast-enhanced ultrasound of the pediatric brain. Pediatr Radiol 51, 2270–2283 (2021). https://doi.org/10.1007/s00247-021-04974-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-04974-4