Abstract
Background
Published case series have described central hepatic macroregenerative nodules or masses as a common feature of Alagille syndrome. Our experience suggests this regenerative pattern can be seen more generally in cholangiopathic disorders.
Objective
To define the frequency of central regenerative tissue in Alagille syndrome and other cholangiopathic disorders and to describe the typical appearance of such regenerative tissue.
Materials and methods
We conducted a retrospective study of CT and MR imaging performed in children and young adults with cholangiopathic disorders between January 2000 and June 2016. Two pediatric radiologists reviewed images in consensus for the presence and features of macroregenerative tissue. Tissue histopathology, when available, was retrieved from the medical record.
Results
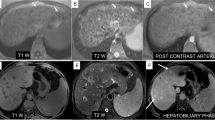
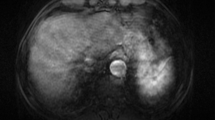
Of 226 patients with cholangiopathic disorders, 23% (52/226) had macroregenerative tissue, and this tissue was central in 96% (50/52). Tissue was well defined and mass-like in 38% (20/52). Regenerative tissue was most common among the subset of patients with Langerhans cell histiocytosis with hepatic involvement (71%, 5/7) and was identified in 43% (16/37) of patients with Alagille syndrome. Regenerative tissue was iso- to hyperintense on T1-weighted MR sequences in 96% (50/52) of cases and hypointense on T2-weighted MR imaging in 94% (48/51). Arterial phase hyperenhancement was present in only five patients (12% of 43), none of whom showed portal venous phase washout. Histopathology was available for 20 cases, all showing benign regenerative tissue.
Conclusion
Central mass-like regeneration appears to be a common regenerative pattern in cholangiopathic disorders and should not be mistaken for malignancy.








Similar content being viewed by others
References
Krantz ID, Piccoli DA, Spinner NB (1997) Alagille syndrome. J Med Genet 34:152–157
Liang JL, Cheng YF, Concejero AM et al (2008) Macro-regenerative nodules in biliary atresia: CT/MRI findings and their pathological relations. World J Gastroenterol 14:4529–4534
Ludwig J (1987) New concepts in biliary cirrhosis. Semin Liver Dis 7:293–301
Alhammad A, Kamath BM, Chami R et al (2016) Solitary hepatic nodule adjacent to the right portal vein: a common finding of Alagille syndrome? J Pediatr Gastroenterol Nutr 62:226–232
Syed MA, Khalili K, Guindi M (2008) Regenerating nodules in arteriohepatic syndrome: a case report. Br J Radiol 81:e79–e83
Tajima T, Honda H, Yanaga K et al (2001) Hepatic nodular hyperplasia in a boy with Alagille syndrome: CT and MR appearances. Pediatr Radiol 31:584–588
Torizuka T, Tamaki N, Fujita T et al (1996) Focal liver hyperplasia in Alagille syndrome: assessment with hepatoreceptor and hepatobiliary imaging. J Nucl Med 37:1365–1367
Wetli SC, Gralla ES, Schibli S, Stranzinger E (2010) Hepatocellular carcinoma and regenerating nodule in a 3-year-old child with Alagille syndrome. Pediatr Radiol 40:1696–1698
Rapp JB, Bellah RD, Maya C et al (2017) Giant hepatic regenerative nodules in Alagille syndrome. Pediatr Radiol 47:197–204
International Working Party (1995) Terminology of nodular hepatocellular lesions. Hepatology 22:983–993
Rougemont AL, Alvarez F, McLin VA et al (2015) Bile ducts in regenerative liver nodules of Alagille patients are not the result of genetic mosaicism. J Pediatr Gastroenterol Nutr 61:91–93
Libbrecht L, Spinner NB, Moore EC et al (2005) Peripheral bile duct paucity and cholestasis in the liver of a patient with Alagille syndrome: further evidence supporting a lack of postnatal bile duct branching and elongation. Am J Surg Pathol 29:820–826
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Roberts, P., Trout, A.T. & Dillman, J.R. Nodular macroregenerative tissue as a pattern of regeneration in cholangiopathic disorders. Pediatr Radiol 48, 932–940 (2018). https://doi.org/10.1007/s00247-018-4129-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4129-5