Abstract
Background
Rapid and accurate diagnosis of appendicitis, particularly with respect to the presence or absence of perforation, is essential in guiding appropriate management. Although many studies have explored sonographic findings associated with acute appendicitis, few investigations discuss specific signs that can reliably differentiate perforated appendicitis from acute appendicitis prior to abscess formation.
Objective
The purpose of our study was to identify sonographic findings that improve the specificity of US in the diagnosis of perforated appendicitis. Our assessment of hepatic periportal echogenicity, detailed analysis of intraperitoneal fluid, and formulation of select constellations of sonographic findings expands upon the literature addressing this important diagnostic challenge.
Materials and methods
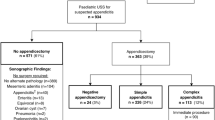
We retrospectively reviewed 116 abdominal US examinations for evaluation of abdominal pain in children ages 2 to 18 years from January 2008 to September 2011 at a university hospital pediatric radiology department. The study group consisted of surgical and pathology proven acute appendicitis (n = 51) and perforated appendicitis (n = 22) US exams. US exams without a sonographic diagnosis of appendicitis (n = 43) confirmed by follow-up verbal communication were included in the study population as the control group. After de-identification, the US exams were independently reviewed on a PACS workstation by four pediatric radiologists blinded to diagnosis and all clinical information. We recorded the presence of normal or abnormal appendix, appendicolith, appendiceal wall vascularity, thick-walled bowel, dilated bowel, right lower quadrant (RLQ) echogenic fat, increased hepatic periportal echogenicity, bladder debris and abscess or loculated fluid. We also recorded the characteristics of intraperitoneal fluid, indicating the relative quantity (number of abdominal regions) and quality of the fluid (simple fluid or complex fluid). We used logistic regression for correlated data to evaluate the association of diagnosis with the presence versus absence of each US finding. We conducted multivariable analysis to identify constellations of sonographic findings that were predictive of perforated appendicitis.
Results
The individual US findings of abscess/loculated fluid, appendicolith, dilated bowel and increased hepatic periportal echogenicity were significantly associated with perforated appendicitis when compared with acute appendicitis (P < 0.01). The sonographic observation of increased hepatic periportal echogenicity demonstrated a statistically significant association with perforated appendicitis compared with acute appendicitis (P < 0.01). The presence of complex fluid yielded a specificity of 87.7% for perforated appendicitis compared with the acute appendicitis group. The US findings of ≥2 regions or ≥3 regions with fluid had specificity of 87.3% and 99.0%, respectively, for perforated appendicitis compared with the acute appendicitis group. Select combinations of sonographic findings yielded high specificity in the diagnosis of perforated appendicitis compared with acute appendicitis. These constellations yielded higher specificity than that of each individual finding in isolation. The constellation of dilated bowel, RLQ echogenic fat, and complex fluid had the highest specificity (99.5%) for perforated appendicitis (P < 0.01).
Conclusion
Our study demonstrates that identification of select constellations of findings using abdominal sonography, in addition to focused US examination of the right lower quadrant, can improve sonographic diagnosis of perforated appendicitis in the pediatric population.





Similar content being viewed by others
References
Somme S, Bronsert M, Morrato E et al (2013) Frequency and variety of inpatient pediatric surgical procedures in the United States. Pediatrics 132:1466–1472
Addiss DG, Shaffer N, Fowler BS et al (1990) The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 132:910–925
Strouse P (2010) Pediatric appendicitis: an argument for US. Radiology 255:8–13
Ramarajan N, Krishnamoorthi R, Barth R et al (2009) An interdisciplinary initiative to reduce radiation exposure: evaluation of appendicitis in a pediatric emergency department with clinical assessment supported by a staged ultrasound and computed tomography pathway. Acad Emerg Med 16:1258–1265
Hernanz-Schulman M (2010) Controversies: CT and US in diagnosis of appendicitis: argument for CT. Radiology 255:3–7
Puylaert JB, Rutgers PH, Lalisang RI et al (1987) A prospective study of ultrasonography in the diagnosis of appendicitis. N Engl J Med 317:666–669
Hayden CK, Kuchelmeister J, Lipscomb TS (1992) Sonography of acute appendicitis in childhood: perforation versus nonperforation. J Ultrasound Med 11:209–216
Garcia Pena BM, Mandl KD, Kraus SJ et al (1999) Ultrasonography and limited computed tomography in the diagnosis and management of appendicitis in children. JAMA 282:1041–1046
Kaiser S, Frenckner B, Jorulf HK (2002) Suspected appendicitis in children: US and CT — a prospective randomized study. Radiology 223:633–638
Simonovsky V (1999) Sonographic detection of normal and abnormal appendix. Clin Radiol 54:533–539
Wiersma F, Sramek A, Holscher HC (2005) US features of the normal appendix and surrounding area in children. Radiology 235:1018–1022
Peletti AB, Baldisseerotto M (2006) Optimizing US examination to detect the normal and abnormal appendix in children. Pediatr Radiol 36:1171–1176
Ozel A, Orhan UP, Akdana B et al (2011) Sonographic appearance of the normal appendix in children. J Clin Ultrasound 39:183–186
Quillin SP, Siegel MJ, Coffin CM (1992) Acute appendicitis in children: value of sonography in detecting perforation. AJR Am J Roentgenol 159:1265–1268
Borushok KF, Jeffrey RB, Laing FC et al (1990) Sonographic diagnosis of perforation in patients with acute appendicitis. AJR Am J Roentgenol 154:275–278
Chan L, Shin LK, Pai RK et al (2011) Pathologic continuum of acute appendicitis: sonographic findings and clinical management implications. Ultrasound Q 27:71–79
Wiersma F, Toorenvliet BR, Bloem JL et al (2009) US examination of the appendix in children with suspected appendicitis: the additional value of secondary signs. Eur Radiol 19:455–461
Blumfield E, Niyak G, Srinivasan R et al (2013) Ultrasound for differentiation between perforated and nonperforated appendicitis in pediatric patients. AJR Am J Roentgenol 200:957–962
Haber HP, Stern M (2000) Intestinal ultrasonography in children and young adults: bowel wall thickness is age dependent. J Ultrasound Med 19:315–321
Dialer I, Hundt C, Bertele-Harms RM et al (2003) Sonographic evaluation of bowel wall thickness in patients with cystic fibrosis. J Clin Gastroenterol 37:55–60
Siegel MJ (2008) Pediatric body CT, 2nd edn. Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia, PA
Abu-Judeh HH (2002) The ‘starry sky’ liver with right-sided heart failure. AJR Am J Roentgenol 178:78
Rak K, Hoper KD, Parker SH (1996) The ‘starry sky’ liver with fasting: variations in glycogen stores? J Ultrasound Med 15:405–407
Siegel MJ (2011) Pediatric sonography, 4th edn. Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia, PA
Quillin SP, Siegel MJ (1994) Appendicitis: efficacy of color Doppler sonography. Radiology 191:557–560
Quillin SP, Siegel MJ (1992) Appendicitis in children: color Doppler sonography. Radiology 184:745–747
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Lieberman JM, Bryan PJ, Cohen AM (1981) Toxic shock syndrome: sonographic appearance of the liver. AJR Am J Roentgenol 173:606–607
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tulin-Silver, S., Babb, J., Pinkney, L. et al. The challenging ultrasound diagnosis of perforated appendicitis in children: constellations of sonographic findings improve specificity. Pediatr Radiol 45, 820–830 (2015). https://doi.org/10.1007/s00247-014-3232-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-014-3232-5