Abstract
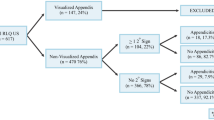
This study evaluated the additional value of secondary signs in the diagnosing of appendicitis in children with ultrasound. From May 2005 to June 2006, 212 consecutive paediatric patients with suspected appendicitis were examined. Ultrasonographic depiction of the appendix was classified into four groups: 1, normal appendix; 2, appendix not depicted, no secondary signs of appendicitis; 3, appendix not depicted with one of the following secondary signs: hyperechoic mesenteric fat, fluid collection, local dilated small bowel loop; 4, depiction of inflamed appendix. We classified 96 patients in group 1, 41 in group 2, 13 in group 3, and 62 in group 4. Prevalence of appendicitis was 71/212 (34%). Negative predictive values of groups 1 and 2 were 99% and 100%, respectively. Positive predictive values of groups 3 and 4 were 85% and 95%, respectively. In groups 3 and 4, hyperechoic mesenteric fat was seen in 73/75 (97.3%), fluid collections and dilated bowel loops were seen in 12/75 (16.0%) and 5/75 (6.6%), respectively. This study shows that in case of non-visualization of the appendix without secondary signs, appendicitis can be safely ruled out. Furthermore, secondary signs of appendicitis alone are a strong indicator of acute appendicitis.
Similar content being viewed by others
Introduction
Acute appendicitis remains a clinical diagnosis [1], but ultrasound (US) proved to be a helpful imaging tool in the evaluation of children with clinically suspected appendicitis [2–5]. Several studies show that additional computed tomography (CT) after a negative or equivocal US can increase the accuracy in the diagnosis of appendicitis [6–8]. In the literature, overall, the sensitivity and specificity of CT in diagnosing appendicitis is higher than sensitivity and specificity of US [9]. However, many studies are concerned about the long-term risk of ionizing radiation of CT, especially in the paediatric population [9, 10]. US findings in diagnosing acute appendicitis are historically divided into three groups; negative, equivocal and appendicitis. Evaluation of secondary signs of appendicitis in absence of the depiction of the appendix might be of use in splitting the equivocal group into a negative or positive US diagnosis of acute appendicitis, using secondary signs as an additional finding. In this study, we applied a new four-part classification of the results of the abdominal US in diagnosing or excluding appendicitis. Therefore, the purpose of this study was to evaluate the additional value of the evaluation of secondary signs of acute appendicitis in children with suspected appendicitis by means of US.
Materials and methods
Patients
From May 2005 to June 2006, 212 consecutive children with acute abdominal pain (acute onset, less then 2 days) who were clinically suspected of having appendicitis and referred by the resident of surgery or the paediatric surgeon in our community-based children’s teaching hospital to the department of radiology for abdominal US were included in our prospective study. Clinical suspicion of appendicitis included a positive history, acute pain in the right lower quadrant of the abdomen, abdominal guarding and elevated C-reactive protein and leucocyte levels. The study population (n = 212) included 129 boys and 83 girls with a mean age of 10 years (age range 2–15 years). Informed consent was obtained from each patient and/or his or her parents. Institutional review board approval was obtained for our study.
Measurements
The abdomen was examined by using an ATL HDI 5000 US system (ATL HDI 5000; Philips Medical Systems). The entire abdomen was examined with a curved-array 2– to 5-MHz transducers, and the right lower quadrant of the abdomen with a 7– to 12-MHz linear-array transducer. The US examinations were performed by a paediatric radiologist with 14 years’ experience in paediatric abdominal US (60% of all the US examinations), a staff radiologist (adult-orientated) during non-working hours with 6–30 years’ experience (altogether they performed 22% of all the US examinations) or a resident of radiology in the third or fourth year of their education with about 6 months of specific experience in paediatric abdominal US (all together they performed 18% of all the examinations).
All abdominal organs were examined with special attention to the appendix, using the graded compression technique [11]. The examiner classified the results of the abdominal US in four groups: 1, normal appendix; 2, appendix not depicted without secondary signs of appendicitis; 3, appendix not depicted with one of the following secondary signs of appendicitis: hyperechogenic mesenteric fat, fluid collection, local dilated small bowel loop; 4, appendicitis with depiction of an inflamed appendix. The normal appendix was defined as a compressible blind-ending lamellated structure without peristalsis. The diameter of the normal appendix is less than 6 mm [12]. Criteria for an inflamed appendix were a non-compressible appendix with a diameter of 6 mm or more with or without the presence of an appendicolith. Secondary signs of appendicitis were increased echogenicity of the surrounding area of the appendix suggesting inflammation of mesenteric fat, local fluid collection suggesting an appendicular abscess, or local dilatation of the thin bowel without peristalsis indicating focal peritonitis. We labelled tissue as inflamed fat when it was recognized with US as hyperechoic, noncompressible intraabdominal mesenteric tissue.
Alternative diagnoses found in patients of group 1 or 2 during US examination causing abdominal pain were recorded. These were defined as infectious ileocaecitis if diffuse thickening of the (sub-) mucosa of the terminal ileum and caecum was depicted, as mesenteric lymphadenitis if enlarged (short axis, 8 mm or more), hypervascular mesenteric lymph nodes (three or more) were depicted [13], as diffuse bowel wall thickening as seen in the clinical diagnosis gastro-enteritis and as colitis or Crohn’s disease when bowel wall thickening of segments of the colon [13] was depicted. Intussusception was defined as a hyperechoic rim of homogenous thickness and contour with a central hyperechoic core at the axial images, also referred to as the ‘doughnut-sign’ [14]. US diagnosis was negative of acute appendicitis in groups 1 and 2. In groups 3 and 4, US diagnosis was positive for acute appendicitis. Patients in US classification groups 3 and 4 were treated surgically and patients in groups 1 and 2 were given expectant treatment (i.e. observation or “wait and see”) or conservative treatment for the alternative diagnosis found by US. The US results were correlated with the pathological findings of those patients who had been operated on and with 1 year clinical follow-up for children who were treated non-surgically. Perforation of the appendix noted at surgery and/or pathological examination was recorded. Clinical data were reviewed of all patients (not-operated) which were given re-evaluation appointments at the out-patient clinic after 1 year for complications (i.e. missed appendicitis) and recurrence of a new episode of abdominal complaints diagnosed as appendicitis within 3 months after the first visit. Surgical data of hospitals in the surrounding area were reviewed to determine whether patients visited another hospital after their primary visit to our hospital.
Statistical analysis
Data analysis was performed using SPSS (SPSS for Windows, version 12.0, SPSS, Chicago, Ill.). Predictive values, sensitivity and specificity of US examination in diagnosing appendicitis were calculated according to standard epidemiologic methods. To evaluate the distribution of perforated appendices in groups 3 and 4, the Fisher’s exact test was used. (The subgroups were too small to apply the chi-squared test). A P value of less than 0.05 was considered to indicate a statistically significant difference.
Results
Prevalence of appendicitis, proven by surgery and/or pathology, in this study was 34% (71/212). The US diagnosis of acute appendicitis was true positive in 70 patients, false positive in five patients (2/13 patients in group 3 and 3/62 patients in group 4), false negative in one patient and true negative in 136 patients. The sensitivity of this US classification method was 99%; the specificity of the imaging strategy was 97%. Negative predictive values (NPVs) of groups 1 and 2 were 99% and 100%, respectively. Positive predictive values (PPVs) of groups 3 and 4 were 85% and 95%, respectively. Outcome results and predictive values of the classification are summarized in Table 1.
A normal appendix was seen in 96 (45%) of 212 patients, all of whom were in group 1 (Fig. 1). No abnormalities were found in 63 of these patients. The alternative diagnoses in this subgroup were mesenteric lymphadenitis (n = 18); infectious ileocaecitis (n = 11); thickening of the sigmoid wall (n = 1, this patient was clinically diagnosed as having Crohn’s disease); diffuse thickening of the bowel wall as seen in the clinical diagnosis of gastroenteritis (n = 1); colitis (n = 1); and in one case, a patient had an abnormally located kidney in the pelvis.
Group 2 contained all the patients whose appendix could not be depicted in the absence of secondary signs of appendicitis (n = 41, 20%). In 32 patients no abnormalities were found ultrasonographically. The alternative diagnoses were mesenteric lymphadenitis (n = 7), infectious ileocaecitis (n = 1) and ileocolic intussusception (n = 1).
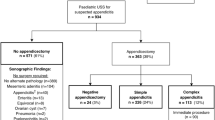
In 13 patients (6%), the appendix was not depicted, but US did indicate secondary signs of appendicitis (Fig. 2). These patients were included in group 3 and their US diagnosis was appendicitis. Present secondary signs were hyperechoic mesenteric fat (13/13), fluid collection (7/13) and local dilated small bowel loop (5/13).
a US image showing a dilated small bowel loop in a patient with secondary signs, but without the depiction of the appendix itself. b Increased echogenicity of the mesenteric fat in the right lower quadrant of the abdomen in the same patient. The patient was included in group 3 (M inflamed mesenteric fat)
Group 4 contained 62 patients (29%) who met the ultrasonographic criteria of acute appendicitis (Fig. 3). Secondary signs were depicted in 60 (97%) patients of this group. In one of the two cases without secondary signs, pathology confirmed acute appendicitis of the paracolic appendix. In the other, pathology showed lymphoid hyperplasia of the appendiceal wall. Present secondary signs were hyperechoic mesenteric fat (60/62), fluid collection (5/62) and there was no dilatation of small bowel loops.
In total, the appendix (normal or inflamed) was depicted in 158 (75%) of all 212 patients. Hyperechoic mesenteric fat was depicted in 97.2% (69/71) of the patients with proven appendicitis. In patients with acute appendicitis, local fluid collections and dilated small bowel loops were depicted in 16.9% (12/71) and 7.0% (5/71), respectively. US classification and pathological correlation are summarized in Table 2.
Seventy-five children went to surgery: one patient of group one (the false negative case) (1/96), all 13 patients of group 3 (13/13), and 61 patients of group 4 (61/62). Pathological results proved appendicitis in 71 of the 75 children, yielding a negative appendectomy rate of 5%. In 22 cases the appendix was perforated; the total perforation rate was 31%. The perforation rate in group 3 was 54% (7/13). In group 4 the appendix was perforated in 24% (15/62) patients. Appendiceal perforation was statistically significant more common in group 3 than in group 4 (P = 0.046).
As mentioned above, the diagnosis was false positive for five patients: two patients of group 3, and three patients of group 4. Four normal appendices were removed surgically. One patient (group 4) was treated conservatively despite the protocol, based on mild clinical presentation. US examination revealed that the origin of the appendix was normal, more distally non-compressible and enlarged (outer diameter 8 mm with local loss of wall structure), but the tip was normal. No appendectomy has been performed for this patient since then.
In one patient there was a non-compressible appendix depicted with a maximal outer diameter of 6 mm. Surgery was performed and pathology showed lymphoid hyperplasia of the appendiceal wall. For another patient, US showed a clearly inflamed appendix and the surgical report stated resection of an inflamed appendix, but pathology results indicated a normal appendix with some lipomatosis. The other two surgically removed normal appendices were not depicted by US, but there were secondary signs of appendicitis. During surgery free pus was clearly visible in the abdomen of one patient; culture of the pus showed presence of Streptococcus pneumoniae. The other patient had an enlarged, macroscopically necrotic, enlarged lymph node. Pathology showed acute inflammation in the lymph node and a normal appendix.
US diagnosis was false negative in one instance; the first US examination in this case showed a normal appendix and symmetrically thickening of the terminal ileum and caecum. Primary diagnosis was thought to be infectious ileocaecitis. Abdominal pain worsened in 10 days, however, whereupon US revealed a large abscess above the right psoas muscle suspected to indicate complicated appendicitis. CT was performed to delineate the size of the abscess, and pathology proved appendicitis.
None of the other patients with a normal appendix or with a non-visualized appendix without secondary signs did have appendicitis during re-evaluation at the out-patient clinic or went to another hospital in the surrounding area during the follow-up period of 1 year.
Discussion
This paper has demonstrated that when ultrasound yields equivocal findings in children with clinically suspected appendicitis, the use of ancilliary signs may help in securing a definitive positive or negative diagnosis. This is especially important as, in this study population, the appendix itself was not depicted, nor were there any secondary signs of acute appendicitis in 20% (n = 41) of the 212 patients. As yet, none of these patients developed acute appendicitis. So, when secondary signs are absent (with or without visualization of the normal appendix) at US examination, the diagnosis of acute appendicitis can be ruled out safely. In a CT study of the appendix, Nikolaidis et al. [15] found similar findings; non-visualization of the appendix and absence of secondary signs of acute appendicitis at CT excludes acute appendicitis.
Secondary signs were depicted in 73 of 75 children with the ultrasonographic diagnosis of appendicitis (groups 3 and 4). Pathology proved the diagnosis of acute appendicitis in 70 (96%) of these 73 children with secondary signs. In only 2 patients (of group 4, i.e. patients with an appendix which met the ultrasonographic criteria of acute appendicitis) there were no secondary signs present upon US examination. The appendix of one patient with proven appendicitis was located paracolically; perhaps the development of secondary signs is limited by its location. In the case of the second patient, pathology showed lymphoid hyperplasia of the appendiceal wall and was regarded as one of the false positive cases in this study. The presence of secondary signs (with or without the depiction of the appendix) in the right lower quadrant of the abdomen, therefore, was a strong indicator of appendicitis in this study population.
Fluid collections, solely or in combination with hyperechogenic mesenteric fat or dilated small bowel loops, were suggestive findings of acute appendicitis in this study population. But most frequently, hyperechogenicity of the mesenteric fat in the right lower quadrant of the abdomen was depicted by sonography as secondary sign of acute appendicitis. In absence of a visualized appendix, this finding strongly suggest appendicitis in this specific patient population. However, Gracey et al. [16] mentioned that a significant proportion of the false-positive scans were based solely on the presence of secondary signs of appendicitis in their study. This was not the case in our study.
Appendiceal perforation was noted statistically significant more in group 3 than in group 4. An explanation of this difference, is the fact that perforation of the appendix is one of the causes of non-visualization of the appendix [17]. According to Sivit et al. [17] the appendix is visible in only 40–60% of the patients with perforation of the appendix. The secondary signs noted in group 3, like local fluid collections, are suggestive of rupture of the appendix.
In the absence of depiction the appendix itself, secondary signs can be very helpful in establishing the right diagnosis. However, hyperechoic mesenteric fat can be seen in ileocaecal Crohn’s disease as well. Then, an erroneous diagnosis of acute appendicitis could be made. US differentiation between the two different diagnoses might be possible.
In case of ileocaecal Crohn’s disease, there is always mural thickening of all layers of the non-compressible ileum surrounded by inflamed mesenteric fat and enlarged, hypovascular lymph nodes. Mural thickening of the ileum can be seen secondary to acute appendicitis as well. However, in acute appendicitis wall layers stay intact, while in Crohn’s disease the layer structure is disturbed locally. In addition to the abnormal ileum there is often prestenotic dilatation, abscess or fistula formation in ileocaecal Crohn’s disease [13].
Despite the high sensitivity and specificity of this classification method, a few false-positive and one false-negative US diagnoses were made. This was probably because there are some pitfalls in diagnosing appendicitis with US [13]. First of all, there are several abdominal entities that can mimic the clinical presentation of appendicitis [13]. In two patients, where ultrasonographic findings showed secondary signs of appendicitis and no depiction of the appendix, pathology proved that there was no appendicitis. In one of these patients, an enlarged, acutely inflamed mesenteric lymph node was resected, and the other patient had primary peritonitis [18, 19]. Secondly, there are also entities that are known to give the appendix an abnormal appearance; for example, lymphoid hyperplasia in the appendix (one patient in this study) [3, 13]. Additionally, in the majority of patients with underlying cystic fibrosis, the outer diameter of the appendix is also increased [20, 21]. Another pitfall is the overlooked distal inflamed appendix, when the appendix is normal at its origin, as was the case in the only false-negative US diagnosis in this study [5, 13]. Finally, another possible trap in diagnosing appendicitis with US is the occurrence of spontaneously resolving appendicitis, as was probably the case in one patient in this current study [13, 22] who was not operated on.
Visualization of the appendix can be hampered by abdominal tenderness, its (retrocaecal) position, overlying bowel loops filled with gas or obesity of the patient [23–26]. Furthermore, ultrasonography is operator-dependent. Therefore, there is a difference among different centres in depicting the appendix by means of US [27]. Our institute is quite comparable with non-specialized community-based centres; the staff radiologists and the residents, together, performed almost 40% of the US examinations. Therefore, the high visualization score of the appendix in this study is not only explained by the presence of a dedicated paediatric radiologist.
The results of this ultrasonographic approach in diagnosing or excluding appendicitis in the paediatric population is of high value because of the greater lifetime radiation risk as a consequence of the increasing use of CT for this population [10]. Despite the fact that patient populations are never completely the same, the sensitivity, specificity and negative appendectomy rate found in this study, as mentioned above, are similar to the sensitivity, specificity and negative appendectomy rate of CT in other studies [3, 23, 28–32]. We think, therefore, that the sensitivity, the specificity and the predictive values of our US classification are high enough to avoid unnecessary radiation of CT in children, even in equivocal cases, without increasing the morbidity as a consequence of missed appendicitis.
Besides the radiation risk, CT is also less desirable in children because of their lack of abdominal fat. Fat stranding is difficult to recognize and the appendix is difficult to distinguish from surrounding bowels due to the absence of body fat [33].
Furthermore, CT, in contrast to US, is more expensive, more invasive with the use of oral, intravenous or rectal contrast, needs sedation in some children and brings additional risks with contrast agents, as well [34].
This study was limited by the lack of pathological proof in those patients for whom no appendectomy was performed. We considered a US that did not suggest appendicitis (i.e. groups 1 and 2) as true negative when patient complaints resolved at the re-evaluation in the out-patient clinic or if patients did not go to another hospital during follow-up and/or had a successful response to conservative treatment of an alternative diagnosis.
In conclusion, this study shows that in case of non-visualization of the appendix without secondary signs, appendicitis can be safely ruled out. The presence of secondary signs of appendicitis without depiction of the appendix itself is a strong indicator of acute appendicitis.
References
Klein MD (2007) Clinical approach to a child with abdominal pain who might have appendicitis. Pediatr Radiol 37:11–14
Dilley A, Wesson D, Munden M et al (2001) The impact of ultrasound examinations on the management of children with suspected appendicitis: a 3-year analysis. J Pediatr Surg 36:303–308
Hahn HB, Hoepner FU, Kalle T et al (1998) Sonography of acute appendicitis in children: 7 years experience. Pediatr Radiol 28:147–151
Rioux M (1992) Sonographic detection of the normal and abnormal appendix. AJR Am J Roentgenol 158:773–778
Sivit CJ, Newman KD, Boenning DA et al (1992) Appendicitis: usefulness of US in diagnosis in a pediatric population. Radiology 185:549–552
Garcia Peña BM, Mandl KD, Kraus SJ et al (1999) Ultrasonography and limited computed tomography in the diagnosis and management of appendicitis on children. JAMA 282:1041–1046
Rao PM, Rhea JT, Novelline RA, Mostafavi AA, McCabe CJ (1998) Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med 338:141–146
Wilson EB, Cole JC, Nipper ML, Cooney DR, Smith RW (2001) Computed tomography and ultrasonography in the diagnosis of appendicitis: when are they indicated. Arch Surg 136:670–675
Doria AS, Moineddin R, Kellenberger CJ et al (2006) US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology 241:83–94
Brenner DJ, Elliston CD, Hall EJ, Berdon WE (2001) Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 176:289–296
Puylaert JBCM (1986) Acute appendicitis: US evaluation using graded compression. Radiology 158:355–360
Wiersma F, Šrámek A, Holscher HC (2005) US features of the normal appendix and surrounding area in children. Radiology 235:1018–1022
Puylaert JBCM (2003) Ultrasonography of the acute abdomen: gastrointestinal conditions. Radiol Clin North Am 41:1227–1242
Verschelden P, Filiatrault D, Garel L et al (1992) Intussusception in children: reliability of US in diagnosis—a prospective study. Radiology 184:741–744
Nikolaidis P, Hwang CM, Miller FH, Papanicolaou N (2004) The nonvisualized appendix: incidence of acute appendicitis when secondary inflammatory changes are absent. AJR Am J Roentgenol 183:889–892
Gracey D, McClure MJ (2007) The impact of ultrasound in suspected acute appendicitis. Clin Radiol 62:573–578
Sivit CJ, Siegel MJ, Applegate KE, Newman KD (2001) When appendicitis is suspected in children. Radiographics 21:247–262
Dann PH, Amodio JB, Rivera R, Fefferman NR (2005) Primary bacterial peritonitis in otherwise healthy children: imaging findings. Pediatr Radiol 35:198–201
Kimber CP, Hutson JM (1996) Primary peritonitis in children. Aust N Z J Surg 66:169–170
Lardenoye SW, Puylaert JB, Smit MJ, Holscher HC (2004) Appendix in children with cystic fibrosis: US features. Radiology 232:187–189
Menten R, Lebecque P, Saint-Martin C, Clapuyt P (2005) Outer diameter of the vermiform appendix: not a valid sonographic criterion for acute appendicitis in patients with cystic fibrosis. AJR Am J Roentgenol 184:1901–1903
Migraine S, Atri M, Bret PM, Lough JO, Hinchey JE (1997) Spontaneously resolving acute appendicitis: clinical and sonographic documentation. Radiology 205:55–58
Puig S, Hörmann M, Rebhandl W, Felder-Puig R, Prokop M, Paya K (2003) US as a primary diagnostic tool in relation to negative appendectomy: six years experience. Radiology 226:101–104
Karakas SP, Guelfguat M, Leonidas JC, Springer S, Singh SP (2000) Acute appendicitis in children: comparison of clinical diagnosis with ultrasound and CT imaging. Pediatr Radiol 30:94–98
Hörmann M, Scharitzer M, Stadler A, Pokieser P, Puig S, Helbich T (2003) Ultrasound of the appendix in children: Is the child too obese. Eur Radiol 13:1428–1431
Ang A, Chong NK, Daneman A (2001) Pediatric appendicitis in “real-time”: the value of sonography in diagnosis and treatment. Pediatr Emerg Care 17:334–340
Peletti AB, Baldiserotto M (2006) Optimizing US examination to detect the normal and abnormal appendix in children. Pediatr Radiol 36:1171–1176
Kaiser S, Frenckner B, Jorulf HK (2002) Suspected appendicitis in children: US and CT—a prospective randomized study. Radiology 223:633–638
Kosloske AM, Love CL, Rohrer JE, Goldthorn JF, Lacey SR (2004) The diagnosis of appendicitis in children: Outcomes of a strategy based on pediatric surgical evaluation. Pediatrics 113:29–34
Applegate KE, Sivit CJ, Salvator AE et al (2001) Effect of cross-sectional imaging on negative appendectomy and perforation rates in children. Radiology 220:103–107
Hernandez JA, Swischuk LE, Angel CA, Chung D, Chandler R, Lee S (2005) Imaging of acute appendicitis: US as the primary imaging modality. Pediatr Radiol 35:392–395
Poortman P, Lohle PNM, Schoemaker CMC et al (2003) Comparison of CT and sonography in the diagnosis of acute appendicitis: a blinded prospective study. AJR Am J Roentgenol 181:1355–1359
Friedland JA, Siegel MJ (1997) CT appearance of acute appendicitis in childhood. AJR A Am J Roentgenol 168:439–442
Kwok MY, Kim MK, Gorelick MH (2004) Evidence-based approach to the diagnosis of appendicitis in children. Pediatr Emerg Care 20:690–698
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Wiersma, F., Toorenvliet, B.R., Bloem, J.L. et al. US examination of the appendix in children with suspected appendicitis: the additional value of secondary signs. Eur Radiol 19, 455–461 (2009). https://doi.org/10.1007/s00330-008-1176-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-008-1176-6