Abstract
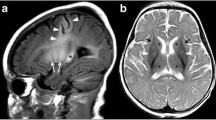
A high metabolic demand, rich vascularization and high concentrations of ionic elements leading to the generation of oxygen free radicals, give to the deep grey matter (DGM) nuclei specific susceptibility to both acute and chronic insults, especially in paediatric patients. Reaching a diagnosis in the early stages of acute diseases in many patients is crucial for instigating prompt specific therapy leading to a favourable outcome. On the basis of a review of a 10-year in-house database and a review of the literature on CNS pathology involving the DGM nuclei in paediatric patients, we summarize the MR findings and clinical clues that may help the radiologist in the difficult differential diagnosis process. The terms “acute” and “chronic” refer to the clinical onset of the disease. MR imaging allows the detection of an injury, determination of its precise anatomical location and characterization of the signal changes. This, combined with a knowledge of specific MRI patterns, may be a roadmap to a definite diagnosis. Clinical history, physical and laboratory findings, timing of the MR examination and advanced MR imaging techniques (diffusion-weighted imaging and 1H-MR spectroscopy), are crucial in some patients.




















Similar content being viewed by others
References
De Long MR (1990) Primate models of movement disorders of basal ganglia origin. Trends Neurosci 13:281–285
Abbruzzese G, Berardelli A (2003) Sensorimotor integration in movement disorders. Mov Disord 18:231–240
McQuillen PS, Ferriero DM (2004) Selective vulnerability in the developing central nervous system. Pediatr Neurol 30:227–235
Huang BY, Castillo M (2008) Hypoxic-ischemic brain injury: imaging findings from birth to adulthood. Radiographics 28:417–439
Ferriero DM (2004) Neonatal brain injury. N Engl J Med 351:1985–1995
Barkovich AJ, Westmark K, Partridge C et al (1995) Perinatal asphyxia: MR findings in the first 10 days. AJNR 16:427–438
Penrice J, Cady EB, Lorek A et al (1996) Proton magnetic resonance spectroscopy of the brain in normal preterm and term infants, and early changes after perinatal hypoxia-ischemia. Pediatr Res 40:6–14
Grant PE, Yu D (2006) Acute injury to the immature brain with hypoxia with or without hypoperfusion. Radiol Clin North Am 44:63–77
Sébire G, Tabarki B, Saunders DE et al (2005) Cerebral venous sinus thrombosis in children: risk factors, presentation, diagnosis and outcome. Brain 128:477–489
Bartynski WS, Boardman JF (2007) Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. AJNR 28:1320–1327
Van Der Knaap MS, Valk J, Barkhof F (2005) Magnetic resonance of myelination and myelin disorders, 3rd edn. Springer, Berlin
Lee HF, Tsai CR, Chi CS et al (2009) Leigh syndrome: clinical and neuroimaging follow-up. Pediatr Neurol 40(2):88–93
Johnson JA, Le KL, Palacios E (2009) Propionic acidemia: case report and review of neurologic sequelae. Pediatr Neurol 40(4):317–320
Michel SJ, Given CA 2nd, Robertson WC Jr (2004) Imaging of the brain, including diffusion-weighted imaging in methylmalonic acidemia. Pediatr Radiol 34:580–582
Harting I, Neumaier-Probst E, Seitz A et al (2009) Dynamic changes of striatal and extrastriatal abnormalities in glutaric aciduria type I. Brain 132:1764–1782
Jan W, Zimmerman RA, Wang ZJ et al (2003) MR diffusion imaging and MR spectroscopy of maple syrup urine disease during acute metabolic decompensation. Neuroradiology 45(6):393–399
Vasconcelos MM, Silva KP, Vidal G et al (1999) Early diagnosis of pediatric Wernicke’s encephalopathy. Pediatr Neurol 20:289–294
Zuccoli G, Siddiqui N, Bailey A et al (2010) Neuroimaging findings in pediatric Wernicke encephalopathy: a review. Neuroradiology 52:523–529
Wilson RK, Kuncl RW, Corse AM (2006) Wernicke’s encephalopathy: beyond alcoholism. Nat Clin Pract Neurol 2:54–58
Burns CM, Rutherford MA, Boardman JP et al (2008) Patterns of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics 122:65–74
Brown WD (2000) Osmotic demyelination disorders: central pontine and extrapontine myelinolysis. Curr Opin Neurol 13:691–697
Steinborn M, Leiz S, Rüdisser K et al (2004) CT and MRI in haemolytic uraemic syndrome with central nervous system involvement: distribution of lesions and prognostic value of imaging findings. Pediatr Radiol 34:805–810
Hopkins RO, Fearing MA, Weaver LK et al (2006) Basal ganglia lesions following carbon monoxide poisoning. Brain Inj 20:273–281
Rovira A, Alonso J, Córdoba J (2008) MR imaging findings in hepatic encephalopathy. AJNR 29:1612–1621
Mirowitz SA, Westrich TJ, Hirsch JD (1991) Hyperintense basal ganglia on T1-weighted MR images in patients receiving parenteral nutrition. Radiology 181:117–120
Mirowitz SA, Westrich TJ (1992) Basal ganglial signal intensity alterations: reversal after discontinuation of parenteral manganese administration. Radiology 185:535–536
Andronikou S, Wilmshurst J, Hatherill M et al (2006) Distribution of brain infarction in children with tuberculous meningitis and correlation with outcome score at 6 months. Pediatr Radiol 36:1289–1294
Kalita J, Ranjan P, Misra UK et al (2003) Hemichorea: a rare presentation of tuberculoma. J Neurol Sci 208:109–111
Saitoh S, Wada T, Narita M et al (1993) Mycoplasma pneumoniae infection may cause striatal lesions leading to acute neurologic dysfunction. Neurology 43:2150–2151
Cambonie G, Houdon L, Rivier F et al (2000) Infantile bilateral striatal necrosis following measles. Brain Dev 22:221–223
Leheup BP, Feillet F, Roland J et al (1987) Lesions of the basal ganglia in mumps. Clinical and neuroradiological development in a case. Rev Neurol (Paris) 143:301–303
Yamamoto K, Chiba HO, Ishitobi M et al (1997) Acute encephalopathy with bilateral striatal necrosis: favourable response to corticosteroid therapy. Eur J Paediatr Neurol 1:41–45
Ho VB, Fitz CR, Chuang SH et al (1993) Bilateral basal ganglia lesions: pediatric differential considerations. Radiographics 13:269–292
Ono J, Shimizu K, Harada K et al (1998) Characteristic MR features of encephalitis caused by Epstein-Barr virus: a case report. Pediatr Radiol 28:569–570
Leber SM, Brunberg JA, Pavkovic IM (1995) Infarction of basal ganglia associated with California encephalitis virus. Pediatr Neurol 12:346–349
Mordekar S, Jaspan T, Sharrard M et al (2005) Acute bilateral striatal necrosis with rotavirus gastroenteritis and inborn metabolic predisposition. Dev Med Child Neurol 47:415–418
Toyoshima M, Maegaki Y, Yotsumata K et al (2007) Antiphospholipid syndrome associated with human herpesvirus-6 infection. Pediatr Neurol 37:449–451
Baum PA, Barkovich AJ, Koch TK et al (1994) Deep gray matter involvement in children with acute disseminated encephalomyelitis. AJNR 15:1275–1283
Rossi A (2008) Imaging of acute disseminated encephalomyelitis. Neuroimaging Clin N Am 18:149–161
Karagulle Kendi AT, Krenzel C, Ott FW et al (2008) Poststreptococcal dystonia with bilateral striatal enlargement: MR imaging and spectroscopic findings. AJNR 29:1276–1278
Author information
Authors and Affiliations
Corresponding author
Additional information
C.C. Quattrocchi and D. Longo contributed equally to this work.
Rights and permissions
About this article
Cite this article
Quattrocchi, C.C., Longo, D., Delfino, L.N. et al. MR differential diagnosis of acute deep grey matter pathology in paediatric patients. Pediatr Radiol 43, 743–761 (2013). https://doi.org/10.1007/s00247-012-2491-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-012-2491-2