Abstract
Background
Intraoperative MRI (ioMRI) has been gaining recognition because of its value in the neurosurgical management of cranial tumours. There is limited documentation of its value in children.
Objectives
To review the initial experience of a paediatric 3-Tesla ioMRI unit in the management of cranial tumours.
Materials and methods
Thirty-eight children underwent ioMRI during 40 cranial tumour resections using a 3-Tesla MR scanner co-located with the neurosurgical operating theatre. IoMRI was performed to assess the extent of tumour resection and/or to update neuronavigation. The intraoperative and follow-up scans, and the clinical records were reviewed.
Results
In 27/40 operations, complete resection was intended. IoMRI confirmed complete resection in 15/27 (56%). As a consequence, surgical resection was extended in 5/27 (19%). In 6/27 (22%), ioMRI was equivocal for residual tumour. In 13/40 (33%) operations, the surgical aim was to partially resect the tumour. In 7 of the 13 (54%), surgical resection was extended following ioMRI.
Conclusion
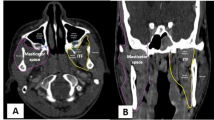
In our initial experience, ioMRI has increased the rate of complete resection, with intraoperative surgical strategy being modified in 30% of procedures. Collaborative analysis of ioMRI by the radiologist and neurosurgeon is vital to avoid errors in interpretation.






Similar content being viewed by others
References
Knauth M, Wirtz CR, Tronnier VM et al (1999) Intraoperative MR imaging increases the extent of tumor resection in patients with high-grade gliomas. AJNR 20:1642–1646
Pamir MN, Ozduman K, Dincer A et al (2009) First intraoperative, shared-resource, ultrahigh-field 3-Tesla magnetic resonance imaging system and its application in low grade glioma resection. J Neurosurg 112:57–69
Nimsky C, Ganslandt O, Von Keller B et al (2004) Intraoperative high-field-strength MR imaging: implementation and experience in 200 patients. Radiology 233:67–78
Maesawa S, Fuji M, Nakahara N et al (2009) Clinical indications for high-field 1.5 T intraoperative magnetic resonance imaging and neuro-navigation for neurosurgical procedures. Neurol Med 49:340–350
Hall WA, Martin A, Haiying L (1998) High-field strength interventional magnetic resonance imaging for pediatric neurosurgery. Pediatr Neurosurg 29:253–259
Kremer P, Tronnier V, Steiner HH et al (2006) Intraoperative MRI for interventional neurosurgical procedures and tumor resection control in children. Childs Nerv Syst 22:674–678
Levy R, Cox RG, Hader WJ et al (2009) Application of intraoperative high-field magnetic resonance imaging in pediatric neurosurgery. J Neurosurg Pediatr 4:465–466
Nimsky C, Ganslandt O, Gralla J et al (2003) Intraoperative low-field magnetic resonance imaging in pediatric neurosurgery. Pediatr Neurosurg 38:83–89
Abernethy LJ, Avula S, Hughes GM et al (2011) Intra-operative 3T MRI for paediatric brain tumours: challenges and perspectives. Pediatr Radiol. doi:10.1007/s00247-011-2280-3
Albright AL, Wisoff JH, Zeltzer PM et al (1996) Effects of medulloblastoma resections on outcome in children: a report from the Children’s Cancer Group. Neurosurgery 38:265–271
Wisoff JH, Boyett JM, Berger MS et al (1998) Current neurosurgical management and the impact of the extent of resection in the treatment of malignant gliomas of childhood: a report of the Children’s Cancer Group trial no. CCG-945. J Neurosurg Paediatr 89:52–59
Rodriguez D, Cheung MC, Housri N et al (2009) Outcomes of malignant CNS ependymomas: and examination of 2408 cases through the Surveillance, Epidemiology and End Results (SEER) database (1973–2005). J Surg Res 156:340–355
Knauth M, Aras N, Wirtz CR et al (1999) Surgically induced intracranial contrast enhancement: Potential source of diagnostic error in intraoperative MR imaging. AJNR 20:1547–1553
Due-Tønnessen BJ, Helseth E, Scheie D et al (2002) Long-term outcome after resection of benign cerebellar astrocytomas in children and young adults (0–19 years): report of 110 consecutive cases. Pediatr Neurosurg 37:71–80
Gunny RS, Hayward RD, Phipps KP et al (2005) Spontaneous regression of residual low-grade cerebellar pilocytic astrocytomas in children. Pediatr Radiol 35:1086–1091
Palma L, Celli P, Mariottini A (2004) Long-term follow-up of childhood cerebellar astrocytomas after incomplete resection with particular reference to arrested growth or spontaneous tumour regression. Acta Neurochir (Vienna) 146:581–588
Saunders DE, Phipps KP, Wade AM et al (2005) Surveillance imaging strategies following surgery and/or radiotherapy for childhood cerebellar low-grade astrocytoma. J Neurosurg 102:172–178
Dorwards IG, Jingquin L, Perry A et al (2010) Postoperative imaging surveillance in pediatric pilocytic astrocytomas. J Neurosurg Pediatr 6:346–352
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Avula, S., Mallucci, C.L., Pizer, B. et al. Intraoperative 3-Tesla MRI in the management of paediatric cranial tumours—initial experience. Pediatr Radiol 42, 158–167 (2012). https://doi.org/10.1007/s00247-011-2261-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-011-2261-6