Abstract
Introduction
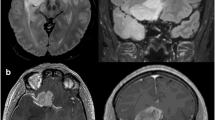
Despite the introduction of neuronavigational systems, radical tumor removal is still problematic in many neurosurgical procedures. Thus, direct intraoperative imaging for tumor resection control was implemented with an intraoperative magnetic resonance imaging (ioMRI) scanner installed in the operating room. Whereas most procedures with ioMRI were carried out in adults, we summarize 7 years of experience using ioMRI in children for interventional neurosurgical procedures or for tumor resection control.
Method
An open magnetic resonance scanner (Magnetom Open 0.2 T) was installed in the neurosurgical operating room. For tumor resection control, ioMRI was performed in 35 procedures. After the ioMRI scans were analyzed with respect to quality, the identification of residual tumor was considered by the attending neuroradiologist and neurosurgeon. If residual tumor tissue was present, a new three-dimensional (3D) dataset was acquired to update the neuronavigation; subsequently, the tumor resection was extended. In all these procedures, the results of the ioMRI were checked by an early postoperative high-field magnetic resonance imaging (MRI) study. In addition, ioMRI was carried out in ten other children to monitor interventional neurosurgical procedures.
Results
In all children, ioMRI was adequate both for tumor resection control and monitoring of interventional procedures. Primary radical removal of tumor was reached in 40% as confirmed by ioMRI, but in 60% of the patients, the tumor resection procedure was extended after residual tumor was detected using the new 3D dataset for navigational update. By using ioMRI, radical tumor removal improved up to 83% as confirmed by early postoperative MRI. Procedure-related complications were not seen in our series. For all MR-guided biopsies, histology findings could be confirmed, and aspiration of intracranial cysts or abscesses could be monitored online.
Conclusion
IoMRI using the open magnetom is suitable for detecting residual tumor tissue, can compensate for the phenomenon of brain shift using a new intraopertive 3D dataset for extended tumor resection, and is capable of monitoring interventional neurosurgical procedures. By using ioMRI for tumor resection control, the degree of tumor resection could be significantly improved.



Similar content being viewed by others
References
Albert FK, Forsting M, Sartor K, Adams HP, Kunze S (1994) Early postoperative magnetic resonance imaging after resection of malignant glioma: objective evaluation of residual tumor and its influence on regrowth and prognosis. Neurosurgery 34:45–61
Albright AL, Wisoff JH, Zeltzer PM, Boyett JM, Rorke LB, Stanley P (1996) Effects of medulloblastoma resections on outcome in children: a report from the Children's Cancer Group. Neurosurgery 38:265–271
Bowers DC, Krause TP, Aronson LJ, Barzi A, Burger PC, Carson BS, Weingart JD, Wharam MD, Melhem ER, Cohen KJ (2001) Second surgery for recurrent pilocytic astrocytoma in children. Pediatr Neurosurg 34:229–234
Bucci MK, Maity A, Janss AJ, Belasco JB, Fisher MJ, Tochner ZA, Rorke L, Sutton LN, Phillips PC, Shu HK (2004) Near complete surgical resection predicts a favorable outcome in pediatric patients with nonbrainstem, malignant gliomas: results from a single center in the magnetic resonance imaging era. Cancer 101:817–824
Fernandez C, Figarella-Branger D, Girard N, Bouvier-Labit C, Gouvernet J, Paz Paredes A, Lena G (2003) Pilocytic astrocytomas in children: prognostic factors—a retrospective study of 80 cases. Neurosurgery 53:544–553
Gwinn R, Cleary K, Medlock M (2000) Use of a portable CT scanner during resection of subcortical supratentorial astrocytomas of childhood. Pediatr Neurosurg 32:37–43
Kremer P, Forsting M, Ranaei G, Wuster C, Hamer J, Sartor K, Kunze S (2002) Magnetic resonance imaging after transsphenoidal surgery of clinically non-functional pituitary macroadenomas and its impact on detecting residual adenoma. Acta Neurochir (Wien) 144:433–443
Modha A, Vassilyadi M, George A, Kuehn S, Hsu E, Ventureyra EC (2000) Medulloblastoma in children—the Ottawa experience. Childs Nerv Syst 16:341–350
Nabavi A, Black PM, Gering DT, Westin CF, Mehta V, Pergolizzi RS Jr, Ferrant M, Warfield SK, Hata N, Schwartz RB, Wells WM III, Kikinis R, Jolesz FA (2001) Serial intraoperative magnetic resonance imaging of brain shift. Neurosurgery 48:787–797
Nimsky C, Ganslandt O, Gralla J, Buchfelder M, Fahlbusch R (2003) Intraoperative low-field magnetic resonance imaging in pediatric neurosurgery. Pediatr Neurosurg 38:83–89
Reinacher PC, van Velthoven V (2003) Intraoperative ultrasound imaging: practical applicability as a real-time navigation system. Acta Neurochir Suppl 85:89–93
Robertson PL, Zeltzer PM, Boyett JM, Rorke LB, Allen JC, Geyer JR, Stanley P, Li H, Albright AL, McGuire-Cullen P, Finlay JL, Stevens KR Jr, Milstein JM, Packer RJ, Wisoff J (1998) Survival and prognostic factors following radiation therapy and chemotherapy for ependymomas in children: a report of the Children’s Cancer Group. J Neurosurg 88:695–703
Stummer W, Novotny A, Stepp H, Goetz C, Bise K, Reulen HJ (2000) Fluorescence-guided resection of glioblastoma multiforme by using 5-aminolevulinic acid-induced porphyrins: a prospective study in 52 consecutive patients. J Neurosurg 93:1003–1013
Tronnier VM, Wirtz CR, Knauth M, Lenz G, Pastyr O, Bonsanto MM, Albert FK, Kuth R, Staubert A, Schlegel W, Sartor K, Kunze S (1997) Intraoperative diagnostic and interventional magnetic resonance imaging in neurosurgery. Neurosurgery 40:891–900
Wirtz CR, Knauth M, Staubert A, Bonsanto MM, Sartor K, Kunze S, Tronnier VM (2000) Clinical evaluation and follow-up results for intraoperative magnetic resonance imaging in neurosurgery. Neurosurgery 46:1112–1120
Wisoff JH, Boyett JM, Berger MS, Brant C, Li H, Yates AJ, McGuire-Cullen P, Turski PA, Sutton LN, Allen JC, Packer RJ, Finlay JL (1998) Current neurosurgical management and the impact of the extent of resection in the treatment of malignant gliomas of childhood: a report of the Children’s Cancer Group trial no. CCG-945. J Neurosurg 89:52–59
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kremer, P., Tronnier, V., Steiner, H.H. et al. Intraoperative MRI for interventional neurosurgical procedures and tumor resection control in children. Childs Nerv Syst 22, 674–678 (2006). https://doi.org/10.1007/s00381-005-0030-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-005-0030-2