Abstract
A modified Fontan procedure is performed to palliate single ventricle malformations. This hemodynamic arrangement sets systemic venous pressure unphysiologically high which predisposes the patient to severe long-term complications. As a means of self-care, exercise may ease transpulmonary flow. We investigated the effects of 6-month exercise prescription on pediatric Fontan patients. Eighteen stable Fontan patients (14 ± 2.6 years, 160.4 ± 11.3 cm, and 51.4 ± 14.4 kg) were recruited. Baseline fitness was assessed by physical activity questionnaire, body composition, cardiorespiratory performance, and muscle fitness tests. Exercise prescription was individually tailored for a 6-month training period at home. At entrance to the study, Fontan patients had lower than normal maximal oxygen uptake (VO2max) of 28. ± 5.9 ml/kg/min (61 ± 11% of normal). VO2max significantly correlated with weekly amount of habitual exercise and muscle mass of the lower limbs (p < 0.001 for both). After 6 months of training, the patients had improved their anaerobic threshold of 18 ± 3.5 vs 20 ± 4.8 ml/kg/min, p = 0.007, and workload tolerance of 119 ± 39 vs 132.4 ± 44 W, p = 0.001. At EUROFIT tests, the patient muscle fitness was below age-matched reference, but correlations existed between VO2max and lower limb muscle tests. Our patients with Fontan hemodynamics were able to positively respond to an exercise program by enhancing submaximal performance which should be beneficial for getting through daily activities. Future studies should correlate whether hemodynamic findings at Fontan completion influence physical activity and exercise reserves, and whether these predict predisposition to chronic complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of patients born with a univentricular heart necessitates a major stepwise palliative heart surgery where the goal is to connect the systemic veins directly into the pulmonary arteries and to use the single ventricle as a pump for the aorta. Although lifesaving, the Fontan procedure results in a pulmonary circulation very different from physiological conditions, with a progressive risk of attrition over time. Without the subpulmonary ventricle, the systemic venous pressure increases 2- to 3-fold in comparison with physiologic normal [1].
In addition, the lack of a pulsatile flow within the pulmonary arterial tree results in impaired pulmonary artery growth and increased pulmonary vascular resistance [2, 3]. As a consequence, increased pulmonary vascular resistance will lead to reduced ventricular preload and cardiac output. Very little can be done by pharmacological means to optimize the function of the successfully accomplished Fontan creation. The chronically increased systemic venous pressure will in most cases eventually lead to overt organ failure [4, 5].
Fontan-operated patients have frequently been described with limited exercise tolerance [6, 7] and investigations have been directed to elucidate whether regular exercise training could improve the patient’s well-being and hemodynamic function and improve their prognosis. Previous studies suggest that aerobic training and lower limb-focused strength training may be a beneficial way to improve the aerobic capacity of Fontan patients, but their significance to the outcome and functional well-being of the patient needs to be investigated [8, 9].
The aim of this study was to evaluate whether after a comprehensive baseline assessment, a personal exercise prescription would improve the aerobic performance of Fontan patients. We hypothesized that in single ventricle patients, maximal cardiopulmonary exercise capacity can be increased by regular aerobic training and bodyweight exercise focusing on lower limbs.
Methods
Study Design
We performed a prospective clinical trial evaluating the efficacy of 6-month exercise prescription for Finnish 8–17-year-old Fontan-operated patients taken care of at the ambulatory Pediatric University clinics in Finland. To mitigate anatomical bias, Fontan patients with both left ventricle and right ventricle as the systemic pump were enrolled. In addition, all patients needed to be self-acting and without any obvious end-organ injury. Exclusion criteria were neurological impediment, short stature, disturbed motor skills, pacemaker therapy, and failing Fontan. Accordingly, 4 patients were not accepted to the study. Baseline measurements were made in spring 2018 and final measurements were held in end of year 2018. Prior to training, the patient’s baseline status was measured by body composition, cardiopulmonary exercise test, and muscle strength tests. After the 6-month intervention period, the same measurements were repeated (Fig. 1). All data collection and measurements took place at the Helsinki University Hospital.
Patient and Public Involvement
The study protocol (Fig. 1) was advocated by the local Ethics committee and accepted by the Pediatric Research Center. Clinical data of 25 patients from cities in Finland were reviewed before contacting the families by phone to outline the study design. Prior to the first visit, the patients and the caregivers were contacted by phone, the willingness to participate was inquired, and if in favor, a signed informed consent form was obtained before enrolling the family to the study. At enrollment, the study protocol was brushed up with the patient and caregiver, and the patient’s disposition and opinion were factored in when self-exercises were tailored. After baseline measurements, two patients failed to follow the study protocol and withdrew from the study. The final study population consisted of 16 children or adolescents of 8–18 years of age (Table 1).
EUROFIT Tests
The patients performed a EUROFIT test [10] for balance, coordination, and muscle strength with European reference values for children and adolescents aged 9–17 years. The strength of the legs, abdominal muscles, hip flexors, and upper body was measured with squats, sit-ups, and push-ups. The number of repetitions in 30 s was recorded. Standing long jump was used to measure the explosive power of the legs and time spent for a 10 times 5-m shuttle run test evaluated running speed and coordination compared to patients’ own baseline tests.
Cardiopulmonary Exercise Testing (CPX)
Cardiopulmonary exercise testing was performed using a bicycle spiroergometer (Ergoselect 200P, Ergoline GmbH, Bitz, Germany) with pediatric pedals. The ramp of resistance was determined and increased at 1 min steps 15 W/1 min or 20 W/1 min according to the height of the individual. The exercise was continued until the respiratory quotient (RQ) was at least 1.0 and the subjective level 17–19/20 on the Borg scale for perceived exertion. Work rate was expressed as the peak work rate (Watt) as well as % of the predicted value according to Harkel et al. [11] Arterial O2 saturation was assessed non-invasively with two pulse oxymeters (MysignS oximeter, Envitec GmbH, Wismar, Germany).
Breath-by-breath gas analysis was performed using Vyntus CPX (Carefusion 234 GmbH, Hoechberg, Germany). For measurement of respiratory gases, a tightly attached face mask (Rudolph series 7910, Hans Rudolph, Kansas City, MI, USA) was used; the dead spaces of the used mask were added to the program. The ventilatory anaerobic compensation threshold was assessed at the point of slope change of V′CO2 exceeding V′O2, increase of V′E/V′O2 compared to V′E/V′CO2, and increase of PetO2 versus PetCO2 (partial pressures of O2 and CO2 in expiratory air) [12].
Body Composition
Bioelectrical impedance analyses (BIA) were used to estimate patients’ fat percentage and fat-free muscle mass [13]. The body BIA measurement was made in a fasted state after a visit to the toilet with a Biacorpus rx4000 meter suitable for pediatric patients (measurement data based on established data exploited by BodyComposition Version 9.0 Professional software, MediCal HealthCare GmbH, Germany [14]). For calculations, the combined muscle mass of the legs was indexed against the patient's weight, both expressed as kilograms.
Exercise Prescription
At admission, patients received a questionnaire previously used in children when investigating habitual physical activity and the risk factors of coronary artery disease (the Finnish LASERI study) [15]. To further evaluate the patients’ subjective exercise tolerance, we added the following questions in addition to the standard ones: (1) Can you keep the same running pace as your classmates or teammates? (2) Do you get breathless more easily during sport than your classmates or teammates?
The initial interview and measurements were used as guide for planning the individualized exercise program. The 6-month exercise prescription included a home-based workout program and a daily step goal. The latter was set according to the patient’s maximal oxygen uptake (VO2max) value in the baseline tests, which was compared to the mean of the steps in the healthy age group [16].
For the home-based workouts, 80 instructional videos with varying intensity level and focusing on the lower body were filmed and uploaded to a cloud server. Each patient received a personal file with an exercise program consisting of 6–8 exercises to be performed 1–2 times a week. For progressivity, the workout program was upgraded every 2 months. Each patient received a wrist-held ZeFit4activity tracker (MyKronoz, Switzerland) and filled in a diary to record the number of daily steps, workouts, and other physical activity during the day. The weekly summaries from the activity tracker were extracted and the diaries were reviewed at the end of the study.
Statistical Analysis
The statistical analyses between the baseline and after the 6-month intervention period were calculated using nonparametric t-tests. The Mann–Whitney test was used to compare continuous variables between left and right systemic ventricle. Correlations were assessed with Pearson’s correlation coefficient between VO2 max and daily amount of activity, lower limb muscle mass, 10 × 5 m shuttle run, standing broad jump, and squats. All data were presented as mean ± standard deviation, and statistical significance was set at p < 0.05. The statistical analyses were performed using GraphPad Prism (Prism 8, version 8.4.2).
Results
Physical Activity Before Exercise Intervention
According to the LASERI questionnaire, 75% of subjects exercised at least 30 min once a week. Almost all subjects (80%) felt able to participate in all the sport activities they wanted and one third of subjects (31%) regularly engaged in guided exercise, such as a sports club, at least once a week. Compared to their peers, 68% of the subjects found running more difficult and slower. The most important factor-limiting performance was shortness of breath, reported by 31% of subjects. Overall, most subjects (93%) felt themselves healthy and energetic or mostly healthy and energetic. At entrance to the study, patients on average reported weekly physical activity of 3 ± 1.5 h.
The baseline investigations demonstrated a statistically significant correlation between weekly physical activity and VO2max (p < 0.0091, Pearson r = 0.628) (Fig. 2A). In addition, the muscle mass of the legs also demonstrated statistically significant correlation with the results of VO2max (p < 0.0161, Pearson r = 0.590) (Fig. 2B).
In the cardiopulmonary exercise test, all patients exceeded a respiratory quotient value of 1, which was interpreted as the maximum test. Maximal oxygen consumption (VO2max) was 28.3 ml/kg/min ± which is 61 ± 11% of the height- and gender-adjusted reference value [11]. The maximum heart rate (86% of age maximum, 205–0.5 × age) and load endurance (77% of expected reference) were also lower than normal (Table 2) [11].
Impact of 6-Month Exercise Prescription
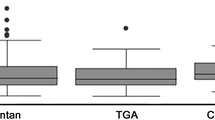
Sixteen patients successfully completed the 6-month training period. There were no major adverse events during the exercise intervention, and all measurements were completed without complications. However, 30% of patients reported fatigue that occasionally affected their ability to concentrate at school. During the 6-month study period, all patients exceeded their daily step goal p < 0.001 (Fig. 3). There was no statistically significant difference in daily steps between the 8–14 and 15–18 age groups (12,197 ± 2458 vs 9793 ± 1910 steps/day, p = 0.071) or for the frequency of domestic strength and coordination training (0.9 ± 0.5 vs 1.5 ± 0.7 workouts/week, p = 0.192). In addition to their scheduled program, patients exercised 4 ± 2.6 additional hours per week.
After the 6-month intervention period, VO2max and peripheral O2 saturation had remained unchanged at 29.4 ± 7.2 ml/kg/min and 93 ± 3 %, respectively (N = 16). However, the anaerobic threshold increased to 20 ± 4.8 ml/kg/min (p < 0.0079) and maximum workload to 132.4 ± 44.4 W (p < 0.0012, Table 2). In addition, the VE/VCO2 slope also decreased from the baseline (32.8 ± 7.6 vs 30.0 ± 5.0, p = 0.049) (Table 2).
At initial measurements, the results from standing broad jump and 10 × 5 m shuttle run were 41% and 62% of reference values, respectively [10]. After 6 months of training, only squats demonstrated significant improvement (p < 0.001) (Table 2). At baseline testing, standing broad jump and 10 × 5 shuttle run test correlated with VO2max (r = 0.613 and r = 0.630, respectively) and following the 6-month intervention period, all three leg muscle tests correlated with VO2max significantly. The correlation between lower limb muscle mass and VO2max was sustained after the intervention period.
Discussion
Our study demonstrated that the 6-month exercise intervention in pediatric Fontan-operated patients increased weekly physical activity and improved submaximal cardiopulmonary performance, workload tolerance and lower limb strength.
Fontan surgery aims at producing hemodynamic conditions that provide the child with competence for natural daily life activities at the expense of limited reserves of cardiac output. However, when the Fontan circulation works well, it allows in active young subjects a better maximal oxygen uptake [17], and in some offers almost equal performance compared to their healthy peers [18]. Consistently, our data on exercise intervention are encouraging and suggest that the patients were able to gain an improved capacity for the daily grind.
Recent exercise studies to improve the performance of Fontan patients have included endurance and resistance training programs and combination of these two. The duration of interventions has varied from 6 weeks to 6 months, and the intensity of training at 60–90% of the VO2max. Some workout programs have been carried out under a controlled environment and some have been done at home and depended on the patient’s own motivation [19,20,21]. Despite these efforts, the results have been modest in terms of improving the peak oxygen consumption or lung function [10] Corroborating with these previous observations, we found that in our study patients, having fat and lean muscle mass in the normal range, the 6-month exercise program had an insignificant effect on VO2max, which remained at 61–63% of age-matched reference value [22].
Previous observations in young adult patients have demonstrated that peripheral muscles promote Fontan circulation and that indexed systemic flow correlates with lower leg muscle mass [23]. Accordingly, our patients received an individualized exercise prescription at an intensity level of 40–60% of their VO2max including exercises for endurance, lower limb muscle strength, and resilience of the musculoskeletal system. We tested the impact of the multifaceted exercise intervention by cardiopulmonary exercise testing [24], bioimpedance measurement to estimate lower limb muscle mass [25], and EUROFIT test to measure dynamic and explosive muscle strength, speed, and coordination [10]. At initial presentation, previous physical activity, lower limb muscle mass, standing broad jumps, and 10 × 5 m shuttle run showed statistically significant correlations with VO2max. Following the 6-month exercise prescription, all these tests and squat repeats per 30 s correlated with VO2max.
Maximal oxygen consumption, exercise duration, and maximum load attained during cardiopulmonary exercise test predict prognosis of heart failure patients in biventricular circulation [12, 26]. In the present exercise study, the VO2max remained unchanged, but the workload attained by the test objects significantly increased, and the VE/VCO2 slope decreased. Meanwhile oxygen consumption is an important surrogate of cardiac output the VE/VCO2 slope is a surrogate for cardiopulmonary capacity since it is a measure of ineffective ventilation [27]. The causes of a high VE/VCO2 slope are poor fitness, increased dead space ventilation, ventilation-perfusion mismatching, and an enhanced chemosensitivity-associated ventilation change [28]. Accordingly, reduction of the VE/VCO2 slope during the study may indeed indicate physical fitness and improvement in ventilation control and peripheral circulation.
Increased cardiopulmonary performance during exercise may play a role in pulmonary vascular remodeling by facilitating transpulmonary flow, thereby impacting on Fontan hemodynamics. Accordingly, it should be investigated whether the child’s natural physically active lifestyle correlates with a well-functioning Fontan circulation, or whether hemodynamic factors after Fontan completion are more important in designating gratification gained from exercise. In addition to a cardiopulmonary or 6-min walk test [24, 29], we believe that lower limb muscle fitness tests and bioimpedance measurements are useful and cost-effective ways to assess the physical condition of Fontan patients. More studies are needed to investigate the potential benefits of a physically active lifestyle on the development of long-term Fontan outcome.
Limitations
Based on previously published data on pediatric patients we anticipated that to detect any response to a regular exercise protocol would call for an extended time span during which confirming adherence may be difficult. We appreciated that in the pediatric age group the parents’ contribution in fulfilling the exercise targets is expected to be significant. To improve quality of the data gathered we gave every patient a diary with spaces for categorized entries, a wrist-held activity tracker with a feature of tabulating daily data and asked the families for permission for motivation contacts by telephone. Our method also allowed evaluation of the hours on the go of the test subjects which demonstrated delightful activation in comparison to the habits before the test period.
As commonly observed, our patients showed chronotropic incompetence [30], which persisted, and an only minor improvement in peak blood pressure despite exercise intervention. With the improved submaximal cardiopulmonary performance and reduced VE/VCO2 slope, we speculate that our intervention positively influenced ventricular filling, which may have derived from better transpulmonary flow. During the 6 months, the pediatric patients showed natural growth. However, we saw insignificant changes in proportional body fat content and lower extremity muscle mass, or standing broad jump and shuttle run as functional variables. Despite some patients becoming exhausted from the exercises, all individuals achieved the daily step goal set for them. Accordingly, we expect that any demotivation during intervention should have attenuated our findings of improvement. Finally, some of our patients may have ventured technically better after performing the test once already and being self-confident after the training period.
Conclusions
We have demonstrated that in pediatric patients with Fontan circulation, an individually planned and multifaceted exercise prescription increases endurance and performance without adverse effects. Our study demonstrated that physical activity and lower limb strength correlate with maximum VO2 and that regular physical activity steps up submaximal exercise performance. Our findings suggest that in single ventricle patients, appropriate peripheral muscle mass boosts cardiopulmonary performance, which may be of great importance for maintaining function and postponing chronic complications. We believe that Fontan patients should receive exercise counseling from medical professionals to support well-being and commonplace performance, since everyday activities are often in the aerobic range.
Change history
16 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00246-022-02871-7
References
Myers CD, Ballman K, Riegle LE, Mattix KD, Litwak K, Rodefeld MD (2010) Mechanisms of systemic adaptation to univentricular Fontan conversion. J Thorac Cardiovasc Surg 140(4):850-856.e6. https://doi.org/10.1016/j.jtcvs.2010.04.015
Gewillig M, Brown SC (2016) The Fontan circulation after 45 years: update in physiology. Heart 102(14):1081–1086. https://doi.org/10.1136/heartjnl-2015-307467
Frescura C, Thiene G (2014) The new concept of univentricular heart. Front Pediatr 2:62. https://doi.org/10.3389/fped.2014.00062/full
Alsaied T, Bokma JP, Engel ME et al (2017) Predicting long-term mortality after Fontan procedures: a risk score based on 6707 patients from 28 studies: ALSAIED et al. Congenit Heart Dis 12(4):393–398. https://doi.org/10.1111/chd.12468
Downing TE, Allen KY, Glatz AC et al (2017) Long-term survival after the Fontan operation: twenty years of experience at a single center. J Thorac Cardiovasc Surg 154(1):243-253.e2. https://doi.org/10.1016/j.jtcvs.2017.01.056
Fernandes SM, McElhinney DB, Khairy P, Graham DA, Landzberg MJ, Rhodes J (2010) Serial cardiopulmonary exercise testing in patients with previous Fontan surgery. Pediatr Cardiol 31(2):175–180. https://doi.org/10.1007/s00246-009-9580-5
Ohuchi H, Negishi J, Noritake K et al (2015) Prognostic value of exercise variables in 335 patients after the Fontan operation: a 23-year single-center experience of cardiopulmonary exercise testing. Congenit Heart Dis 10(2):105
André LG, Gewillig M (2010) What limits cardiac performance during exercise in normal subjects and in healthy Fontan patients? Int J Pediatr 2010:1–8. https://doi.org/10.1155/2010/791291
Cordina R, d’Udekem Y (2019) Long-lasting benefits of exercise for those living with a Fontan circulation. Curr Opin Cardiol 34(1):79–86. https://doi.org/10.1097/HCO.0000000000000582
Tomkinson GR, Carver KD, Atkinson F et al (2018) European normative values for physical fitness in children and adolescents aged 9–17 years: results from 2 779 165 Eurofit performances representing 30 countries. Br J Sports Med 52(22):1445–1456. https://doi.org/10.1136/bjsports-2017-098253
Ten Harkel AD, Takken T, Van Osch-Gevers M, Helbing WA (2011) Normal values for cardiopulmonary exercise testing in children. Eur J Cardiovasc Prev Rehabil 18(1):48–54. https://doi.org/10.1097/HJR.0b013e32833cca4d
Balady GJ, Arena R, Keteyian SJ et al (2010) Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation 122(2):191–225. https://doi.org/10.1161/CIR.0b013e3181e52e69
Chula de Castro JA, de Lima TR, Silva DAS (2017) Body composition estimation in children and adolescents by bioelectrical impedance analysis: a systematic review. J Bodywork Mov Ther 22(1):134–146. https://doi.org/10.1016/j.jbmt.2017.04.010
Kreissl A, Jorda A, Truschner K, Skacel G, Greber-Platzer S (2019) Clinically relevant body composition methods for obese pediatric patients. BMC Pediatr 19(1):84. https://doi.org/10.1186/s12887-019-1454-2
Raitakari OT, Juonala M, Viikari JSA (2005) Obesity in childhood and vascular changes in adulthood: insights into the cardiovascular risk in young Finns study. Int J Obes 29:S101–S104. https://doi.org/10.1038/sj.ijo.0803085
Tudor-Locke C, Craig CL, Beets MW et al (2011) How many steps/day are enough? for children and adolescents. Int J Behav Nutr Phys Act 8(1):78. https://doi.org/10.1186/1479-5868-8-78
Rato J, Sousa A, Cordeiro S, Mendes M, Anjos R (2020) Sports practice predicts better functional capacity in children and adults with Fontan circulation. Int J Cardiol 306:67–72. https://doi.org/10.1016/j.ijcard.2019.11.116
Cordina R, du Plessis K, Tran D, d’Udekem Y (2018) Super-Fontan: is it possible? J Thorac Cardiovasc Surg 155(3):1192–1194. https://doi.org/10.1016/j.jtcvs.2017.10.047
Sutherland N, Jones B, Westcamp Aguero S et al (2018) Home- and hospital-based exercise training programme after Fontan surgery. Cardiol Young 28(11):1299–1305. https://doi.org/10.1017/S1047951118001166
Hedlund ER, Lundell B, Söderström L, Sjöberg G (2018) Can endurance training improve physical capacity and quality of life in young Fontan patients? Cardiol Young 28(3):438–446. https://doi.org/10.1017/S1047951117002360
Scheffers LE, Berg LEMV, Ismailova G, Dulfer K, Takkenberg H, Helbing W (2020) Physical exercise training in patients with a Fontan circulation: a systematic review. Eur J Prev Cardiol. https://doi.org/10.1177/2047487320942869
Longmuir PE, Corey M, Faulkner G, Russell JL, McCrindle BW (2015) Children after Fontan have strength and body composition similar to healthy peers and can successfully participate in daily moderate-to-vigorous physical activity. Pediatr Cardiol 36(4):759–767. https://doi.org/10.1007/s00246-014-1080-6
Cordina R, Celermajer DS, d’Udekem Y (2018) Lower limb exercise generates pulsatile flow into the pulmonary vascular bed in the setting of the Fontan circulation. Cardiol Young 28(5):1–733. https://doi.org/10.1017/S104795111800015X
Udholm S, Aldweib N, Hjortdal VE, Veldtman GR (2018) Prognostic power of cardiopulmonary exercise testing in Fontan patients: a systematic review. Open Heart 5(1):e000812. https://doi.org/10.1136/openhrt-2018-000812
Powell AW, Wittekind SG, Alsaied T et al (2020) Body composition and exercise performance in youth with a Fontan circulation: a bio-impedance based study. J Am Heart Assoc 9(24):e018345. https://doi.org/10.1161/JAHA.120.018345
Keteyian SJ, Patel M, Kraus WE et al (2016) Variables measured during cardiopulmonary exercise testing as predictors of mortality in chronic systolic heart failure. J Am Coll Cardiol 67(7):780–789. https://doi.org/10.1016/j.jacc.2015.11.050
Cahalin LP, Chase P, Arena R et al (2013) A meta-analysis of the prognostic significance of cardiopulmonary exercise testing in patients with heart failure. Heart Fail Rev 18(1):79–94. https://doi.org/10.1007/s10741-012-9332-0
Ollila L, Heliö T, Sovijärvi A et al (2017) Increased ventilatory response to exercise in symptomatic and asymptomatic LMNA mutation carriers: a follow-up study. Clin Physiol Funct Imaging 37(1):8–16. https://doi.org/10.1111/cpf.12260
Sen S, Bandyopadhyay B, Eriksson P, Chattopadhyay A (2012) Functional capacity following univentricular repair—midterm outcome. Congenit Heart Dis 7(5):423–432. https://doi.org/10.1111/j.1747-0803.2012.00640.x
Takken T, Hulzebos HJ, Blank AC, Tacken MHP, Helders PJM, Strengers JLM (2007) Exercise prescription for patients with a Fontan circulation: current evidence and future directions. Netherlands Heart J 15(4):142–147
Acknowledgements
We thank Professor Juha Sinisalo for his valuable critical comments during the preparation of the manuscript.
Funding
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital. This work has received valuable support from Kirsti and Tor Johansson’s Foundation for Heart and Cancer Research, the Foundation for Paediatric Research, and the Finnish Foundation for Cardiovascular Research. We received no support from any organization for the submitted work and have no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; we have no other relationships or activities that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Contributions
HP: communication with the families; designing, scheduling, coordination, and performing of the patient measurements; data recording and calculations; coordinating manuscript versions and commentary. OR: work supervision and study design; patient recruitment; communication with the families; interpretation of the data; manuscript commenting. NR: cardiopulmonary exercise testing (cpx) with HP; cpx data extraction and reporting. SL: bioimpedance measurements and data tabulation. HT: data discussions and manuscript commenting. PP: head of cpx laboratory; cpx data extraction and reporting; author of the cpx section. OP-A: conceiving the research idea, study design, research grant holder; work supervision; patient recruitment and communication with the families; data interpretation; corresponding investigator, senior author, and guarantor of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original article has been revised due to author first and last name mixed up.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pyykkönen, H., Rahkonen, O., Ratia, N. et al. Exercise Prescription Enhances Maximal Oxygen Uptake and Anaerobic Threshold in Young Single Ventricle Patients with Fontan Circulation. Pediatr Cardiol 43, 969–976 (2022). https://doi.org/10.1007/s00246-021-02806-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02806-8