Abstract
It is unclear whether residual anterograde pulmonary blood flow (APBF) at the time of Fontan is beneficial. Pulsatile pulmonary flow may be important in maintaining a compliant and healthy vascular circuit. We, therefore, wished to ascertain whether there was hemodynamic evidence that residual pulsatile flow at time of Fontan promotes clinical benefit. 106 consecutive children with Fontan completion (1999–2018) were included. Pulmonary artery pulsatility index (PI, (systolic pressure–diastolic pressure)/mean pressure)) was calculated from preoperative cardiac catheterization. Spectral analysis charted PI as a continuum against clinical outcome. The population was subsequently divided into three pulsatility subgroups to facilitate further comparison. Median PI prior to Fontan was 0.236 (range 0–1). 39 had APBF, in whom PI was significantly greater (median: 0.364 vs. 0.177, Mann–Whitney p < 0.0001). There were four early hospital deaths (3.77%), and PI in these patients ranged from 0.214 to 0.423. There was no correlation between PI and standard cardiac surgical outcomes or systemic oxygen saturation at discharge. Median follow-up time was 4.33 years (range 0.0273–19.6), with no late deaths. Increased pulsatility was associated with higher oxygen saturations in the long term, but there was no difference in reported exercise tolerance (Ross), ventricular function, or atrioventricular valve regurgitation at follow-up. PI in those with Fontan-associated complications or the requiring pulmonary vasodilators aligned with the overall population median. Maintenance of pulmonary flow pulsatility did not alter short-term outcomes or long-term prognosis following Fontan although it tended to increase postoperative oxygen saturations, which may be beneficial in later life.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
In the current era, the standard surgical pathway for functional univentricular heart (fUVH) palliation comprises a sequence of three-staged interventions [1] to create a total cavopulmonary connection (TCPC), transforming the prognosis for children with complex fUVH [2]. An incremental improvement in survival has been matched by impressive late functional outcomes, with over 90% of survivors remaining in New York Heart Association (NYHA) classes I–II at follow-up [3,4,5]. Despite this success, the inherent limitations of this circuit are becoming increasingly pronounced as the population of survivors grows, with substantial disease burden [6, 7] and a decline in freedom from late adverse events [8].
The absence of pulsatile pulmonary perfusion markedly deranges systemic hemodynamics. This paradoxical state of systemic venous hypertension and chronic low cardiac output [9, 10] has pernicious effects on multiple organ systems [11], mediating a progressive, and frequently indolent, circulatory demise—the Fontan ‘paradox’ [10]. There is no universally efficacious treatment for the failing Fontan, aside from targeted surgical or catheter-based interventions for isolated problems. Thus, cardiac transplantation represents the only viable definitive long-term option; this is far from a practical solution with a shortage of donor allografts and the high morbidity and mortality that follows a previous Fontan procedure [12]. As a result, we need to develop novel therapies to effectively manage long-term complications and minimize the inherent inefficiencies of the Fontan circuit.
Total pulmonary vascular resistance (PVR) is a primary determinant of cardiac output after the Fontan procedure [13,14,15]. As PVR increases, a functional decline in the Fontan circulation is expected [16]. In turn, low PVR is contingent on good pulmonary artery (PA) dimensions [17], a well-developed and compliant pulmonary vascular bed [18], along with other factors such as good systemic ventricular mechanics. There is evidence to suggest that elevated PVR after Fontan may reflect inadequate preparation during earlier staging operations [19].
During the interim bidirectional Glenn (BDG) procedure, a clinical decision is often made whether to exclude or preserve additional sources of pulmonary flow [20]. Currently, conflicting data exist regarding the potential utility or harmfulness of maintaining forward flow through a patent (banded, or natively stenotic) pulmonary outflow tract [21,22,23]. This anterograde pulmonary blood flow (APBF) may be an important trophic stimulus for the pulmonary arterial tree, with reports of improved PA growth where APBF is preserved [24,25,26,27]. However, concerns remain that accessory pulmonary flow may compromise ventricular volume unloading [28], thereby mitigating some of the advantageous changes mediated by the classical BDG [29].
Chronic privation of pulsatile pulmonary flow is detrimental for endothelial function, capillary recruitment, and pulmonary vascular development, all which impact PVR, as seen in both canine [30] and rabbit [31] models. Thus, the argument for preserving pulsatile pulmonary flow is compelling. However, we do not yet know whether this leads to improved hemodynamic outcome in Fontan patients. We have previously shown the utility of maintaining residual APBF following BDG [32], but there is no evidence of studies which correlate this with clinical outcome after the Fontan. We, therefore, hypothesized in the present study that pulsatile perfusion is integral for the maintenance of a compliant and low resistance pulmonary vascular bed.
Methods
We conducted a single-center retrospective study, involving serial follow-up of each patient who underwent Fontan palliation at University Hospitals Bristol NHS Foundation Trust. Demographic data, clinical data, including primary anatomic diagnoses, cardiac surgical history, inpatient reports, and relevant cardiac investigations, were retrieved from electronic medical records. Formal ethical committee approval was waived given the retrospective anonymized study design, and written informed consent was not required.
Patient Selection
From January 1999 to December 2018, 183 patients underwent Fontan completion at our institution. Following exclusion of patients with incomplete cardiac catheterization data (n = 29), and those lost during follow-up from other centers (n = 48), 106 patients were included in the analysis.
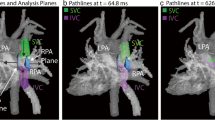
Evaluation of Pulmonary Artery Pulsatility
Pulmonary hemodynamics were evaluated using routine preoperative cardiac catheterization data. Transpulmonary gradient (PA mean pressure − left atrial pressure) was recorded and a pulmonary artery pulsatility index (PI) calculated for each patient, as follows:
PI = (systolic pressure − diastolic pressure)/mean pressure, where all values pertain to PA indices.
The study population was subsequently divided into three, based on pulsatility magnitude. The ‘low PI’ subgroup included patients with PI value < 0.334, ‘medium PI’ between and including 0.334–0.666, and ‘high pulsatility’ > 0.666.
Pulmonary artery size was not routinely measured at our centre during the time period of this retrospective study, and, accordingly, Nakata indices have not been included. Similarly, data concerning the presence or absence of pulmonary collaterals were sparse in available documentation and have consequently not been recorded in this current analysis.
Clinical Outcome Measures
Standard cardiac surgical outcomes included in-hospital mortality, postoperative ventilation time, duration of chest tube drainage, length of pediatric intensive care unit stay (PICU) and total hospital stay, systemic arterial oxygen saturation (SaO2), and medications at discharge.
Longitudinal follow-up included assessment of ventricular function, graded as per echocardiography: 1, severely reduced; 2, moderately reduced; 3, mildly reduced; 4, acceptable or preserved; and 5, normal or excellent. Similarly, atrioventricular valve regurgitation (AVVR) was graded as 1, severe; 2, moderate regurgitation; 3, mild regurgitation; 4, trivial regurgitation; 5, no regurgitation.
Exercise tolerance was graded using the NYHA functional classification, or Ross for children which provides a NYHA-equivalent score [33]. Oxygen saturation by pulse oximetry (at 1-year and last follow-up) and medication support (diuretics and vasodilatory therapy) were also recorded. Intermediate (within one year) and late (after one year) Fontan failure was defined as follows: (i) Fontan takedown or pathway revision, (ii) transplantation, and (iii) in-hospital or Fontan complication-associated mortality, as adapted from The Society of Thoracic Surgeons’ criteria [34, 35].
Statistical Analysis
Data were analyzed using GraphPad Prism v.8.4.1 software. Two distinct analytical approaches were adopted: (i) Spectral analysis, where PI was charted as a continuum against clinical outcome data, and (ii) subgroup analysis, based on relative pulsatility (low, medium, or high), to identify any non-linear relationships between PI and the defined outcomes measures. Categorical variables are expressed as frequency (%). Continuous data are summarized as either mean ± standard deviation (SD) or median and range values, after testing for normality (Shapiro–Wilk) and equality of variance (F-statistic).
For spectral analysis, the Pearson (continuous data) and Spearman (categorical data) rank coefficients (r) were calculated to assess correlation between PI and outcome measures. Analysis of variance (ANOVA) (parametric) and Kruskal–Wallis (non-parametric) tests were employed for PI subgroup analysis, as appropriate. All tests were two tailed, and statistical significance accepted for p-value < 0.05.
Results
Baseline Patient Characteristics
106 subjects were included in our final analysis, of which 66 were male (62.3%). The most common diagnosis was double-inlet left ventricle (18%). Patient demographics and principal diagnoses are summarized in Table 1.
The median age at Fontan completion was 4.90 years (range 1.83–17.6 years). Prior procedures included systemic-to-PA shunt (n = 37, 34.9%) and pulmonary artery banding (n = 27, 25.4%), with four patients (3.77%) undergoing both shunt and banding during initial palliation. 27 patients had a natively stenosed pulmonary outflow tract to protect the pulmonary circuit from volume overload, and bidirectional Glenn (BDG) served as the initial palliation in 15 of these patients. Although we included the hypoplastic left heart syndrome (HLHS) group, it is clear that none of these will have had pulsatile forward flow.
All patients underwent BDG prior to TCPC, at a median age of 0.822 years (range 0.140–11.7 years). Maintenance of anterograde flow was considered on a case-to-case basis. While there was no specific protocol in place, residual forward flow was occluded where there was any indication of volume overloading of the systemic ventricle; this clinical decision required multidisciplinary input and close communication between the medical and surgical teams. At the time of Fontan, 39 patients (36.8%) had residual APBF, but none after the Fontan operation, and a fenestrated Fontan was performed in 11 cases (10.4%). Pre-operative echocardiography showed excellent or preserved ventricular function in 88.5%; however, 54.5% had evidence of at least mild AVVR. Median SaO2 at preoperative assessment was 81% (range 57–92%).
Cardiac Catheterization Data
The median pulsatility index (PI) prior to Fontan completion was 0.236 (range 0–1). Notably, as expected, PI was significantly greater in individuals with persistent APBF versus those without (median PI: 0.364 vs. 0.177), as per Mann–Whitney U test (U = 599.5, p < 0.0001).
Patients were stratified into three groups according to PI, as follows: low (PI < 0.334, n = 76), medium (0.334 ≤ PI < 0.667, n = 19), and high (PI ≥ 0.667, n = 11) pulsatility. Of the 11 patients who underwent Fontan with fenestration, 10 (90.9%) were in the low PI subgroup.
The mean TPG was 4.23 mmHg (± 2.10), and this somewhat tended to increase with PI. (Pearson r = 0.166, p = 0.0921 = non-significant). Subgroup analysis did not delineate any significant difference in TPG between the three PI groups (ANOVA, p = 0.116).
Early Outcomes
There were four early hospital deaths following the Fontan operation, with an early mortality of 3.77%. PI ranged between 0.214 and 0.423 in these subjects. Table 2 outlines the dominant cardiac diagnosis and cause of death.
There was no correlation between PI and any of the standard cardiac surgery outcome measures (Fig. 1) including (a) ventilatory time, (b) duration of chest drainage, (c) PICU, and (d) total hospital stay, as per Pearson r. Although there were some trends, there was no statistically significant difference for the spectral analysis of ventilatory time r = − 0.0948, p = 0.351, for duration of chest drainage r = 0.123 p = 0.229, for PICU stay r = − 0.0984 p = 0.333, for total hospital stay r = − 0.0386 p = 0.697, for oxygenation at discharge r = 0.0794 p = 0.430. This remained consistent on subgroup analysis, as described below.
Analysis of standard surgical outcome measures as a function of pulsatility. Results from subgroup analysis are shown, with Kruskal–Wallis p values; a Ventilation time, b Chest drainage duration, c PICU stay, d Total hospital stay, e SaO2 at discharge. Abbreviations—PI pulsatility index; PICU pediatric intensive care unit; SaO2 systemic arterial oxygen saturation
The median SaO2 at discharge was 95% (range: 70–100%). As expected, this was significantly higher than at preoperative assessment (Mann–Whitney U = 499, p < 0.0001). There was no correlation between PI and SaO2 at discharge (Pearson r = 0.0794, p = 0.4301), and no notable inter-group differences either (Kruskal–Wallis, p = 0.1159) (Fig. 1e). Two patients with fenestrated Fontan had complicated postoperative courses, one due to acute ischaemic stroke and one due to prolonged bilateral pleural effusions. However, upon comparing median values, outcomes of those with fenestration were congruent with the remainder of the low PI subgroup.
Long-Term Outcomes
The median follow-up time was 4.33 years (range 0.0273–19.6 years). No further deaths were reported, with an overall survival of 93.6% in this cohort.
Five patients (4.72%) developed complications within the first year, three of whom required surgical or catheter-based intervention; one developed severe congestive heart failure at seven months, necessitating cardiac transplantation. The two others developed Fontan failure at two months postoperatively, due to (i) complete occlusion of the left pulmonary artery, managed by balloon dilatation with stenting, and (ii) right ventricular dysfunction secondary to arrhythmia, requiring fenestration. Table 3 summarizes the pertinent clinical information of these cases.
At last follow-up, echocardiographic assessment revealed excellent or preserved ventricular function in 92.7% and at least mild AVVR in 55.5%. Changes in ventricular function and AVVR were calculated as the net difference between preoperative and most recent echocardiograph gradings. There was no linear correlation relationship between PI and changes in ventricular function or AVVR. The median change in ventricular function and AVVR in all three PI subgroups was 0; however, those with medium PI tended towards improved ventricular function (Kruskal–Wallis, p = 0.0723), but this trend was not replicated with AVVR. (Table 4). MRI data were available for 55 patients (51.9%) and were reported as either left ventricular indices (n = 24), right ventricular indices (n = 12) or combined left and right ventricular indices (n = 19). Given this incomplete and heterogeneous dataset, formal analysis was not completed.
The cohort demonstrated good exercise tolerance during follow-up, with 96.9% falling into class I–II of the NYHA or Ross classification. Formal analysis of the CPET data was not performed as the data were limited (n = 19, 17.9% of cohort). At 1-year follow-up, the median systemic arterial oxygenation was 95% (range 77–100%). In patients who had completed more than one postoperative year, the last recorded SaO2 was 95% (range 82–100%) at a median of 6.3 years follow-up (range 1.19–17.77 years). While there was a tendency toward improved oxygenation with increased pulsatility, this was not statistically significant on spectral or subgroup analysis (Fig. 2). Clinical outcomes of those with fenestrated Fontan aligned with the remainder of the low PI subgroup and with the overall population median.
Long-term oxygenation status at 1-year and last follow-up. Spectral analysis is presented on the left-hand side, at a 1-year and c last follow-up, with calculation of Pearson r and associated p value. Light gray represents data points from the ‘low PI,’ medium gray from the ‘medium PI,’ and dark gray from the ‘high PI’ group. On the right, results from subgroup analysis are shown, at b 1-year and d last follow-up, with Kruskal–Wallis p values
During the follow-up period, a further 11 patients (13.2%) developed Fontan-associated complications (Table 5). These included intractable arrhythmias (atrial, n = 3; ventricular, n = 1), Fontan-associated liver disease (n = 4), protein-losing enteropathy (n = 2), and arterial collaterals (n = 1). Of note, two patients who developed atrial arrhythmias had underwent fenestrated Fontan. The median time at onset of late complications was 6.06 years; however, four patients out of 11 (36.4%) developed complications at or after 10 years.
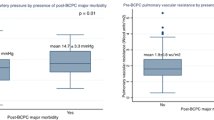
The median PI in those with intermediate- or late-Fontan-associated complications (n = 16, PI = 0.225) and those receiving (i) pulmonary vasodilator therapy (n = 7, PI = 0.1364), (ii) carvedilol (n = 7, PI = 0.20), or (iii) diuretics (n = 10, PI = 0.144) largely aligned with the overall population median (0.236), and included individuals from all three (low, medium, and high) PI subgroups (Fig. 3). While the absolute median PI values were lower in these patient subsets, the event rate was too small for statistical significance.
PI and adverse long-term outcomes. Distribution of Pulsatility Index (PI) in Patients with Fontan-associated complications, and those requiring pulmonary vasodilator or diuretic therapy at last follow-up. Median and interquartile range (IQR) are plotted. Abbreviations—FAD Fontan-associated disease or complications; PI pulsatility index
Of those with fenestrated Fontan, three patients (27.2%) were prescribed carvedilol in the long term, and one prescribed both carvedilol and diuretics (9.09%), indicating a significant associated morbidity.
Discussion
Despite its unprecedented success, the inherent haemodynamic aberrancies of the Fontan circulation align with a time-related decrement in functional status [36], an ongoing risk of severe complications, and a life expectancy that remains significantly lower than the biventricular population [37]. Crucially, impaired pulmonary endothelial function, due to loss of pulsatile perfusion, may play a dominant pathophysiologic role in the development of elevated PVR in Fontan patients. We have, however, shown that maintenance of pulmonary artery pulsatility with some form of forward flow at the time of the Fontan does not alter the short-term outcomes, or long-term prognosis but is associated with increased postoperative oxygen saturations.
The benefits of pulsatile blood flow are prominent in the literature. In lungs isolated from neonatal rabbits, increased pulsatility levels mediated a reduction in vascular resistance [38]. This finding has been corroborated in a chronic porcine model of BDG [39], where partial ligation of the PA (micropulsatile group with APBF) was associated with a significantly lower PVR, compared to animals who underwent complete PA ligation. Notably, flow pulsatility positively correlated with maximal vasodilatory response to acetylcholine, and attenuated the development of pulmonary hypertension; this implies a direct role of pulsatility in preserving endothelial function and demonstrates the underlying functional sensitivity of the vascular endothelium to shear stress magnitude [40].
This prompts several considerations for our study: first, the need to determine the optimal level of auxiliary APBF to both minimize risk of ventricular volume overload and, concurrently, retain sufficient pulsatility to preserve pulmonary endothelial function. To complicate matters further still, this figure is unlikely to remain static, given the continued somatic growth of the child during the palliation process. Next, where pulmonary artery banding restricts anterograde outflow to subcritical levels, blood flow becomes increasingly laminar in character. Similarly, hemodynamics resulting from a systemic-to-PA shunt, or where significant aortopulmonary collaterals have developed [41], may more closely mirror the arterial, rather than venous, waveform and possess a pulsatile character. On this premise, our study design refrained from arbitrarily classifying subjects as ‘pulsatile’ and ‘nonpulsatile’ based on preconceived notions regarding APBF. Nevertheless, analysis of our cohort found that pulsatility index was significantly greater in those with residual anterograde flow (p < 0.0001).
This present study did not elicit any significant differences in early or late clinical outcomes based upon PA pulsatility at the time of Fontan. Although the median PI in those requiring long-term vasodilator or diuretic therapy was notably lower than the cohort average (0.136, 0.144, and 0.236, respectively), the event rate was too low for robust statistical analysis. One of the main practical challenges of our study design was the retrospective assessment of pulsatility. We elected to use the equation: Pulsatility Index (PI) = (PA systolic pressure–PA diastolic pressure)/PA mean pressure, as adapted from the doppler-derived blood velocity formula which is routinely employed in other clinical fields, including obstetrics [42] and stroke medicine [43]. A literature search identified one previous record of this equation in assessing pulmonary blood flow pulsatility, in a study attempting to differentiate between pulmonary arterial and chronic pulmonary thromboembolic hypertension using PI [44]. We viewed this to be more appropriate and physiologically sound than other indices; in particular, the novel pulmonary artery pressure index (PAPi) = (PA systolic pressure/PA diastolic pressure)/right atrial pressure [45], which holds prognostic relevance in right heart failure, would likely be an unreliable measure in the setting of AVVR, as commonly observed in our patients.
The lack of (i) unanimous criteria to quantify and (ii) a robust method to assess pulsatility is problematic. Other centers have adopted echocardiographic [46] or CMR-based [47] assessments of PA pulsatility index, using the doppler-derived formula alluded to above, where PI = (peak systolic velocity – end diastolic velocity)/time averaged velocity. Echocardiography would likely be technically challenging, due to the acoustic interference from lung tissue, and may be limited by poor reproducibility [48]. However, CMR is a particularly appealing tool with the potential to not only analyze the complex flow dynamics but also provide detailed anatomic and functional information about the single ventricle. Indeed, it has previously been demonstrated that pulsatile flow is dependent on energy, rather than pressure, gradient [49], with pulsatile flow transmitting 2.4 times the amount of energy as nonpulsatile flow at the same mean pressure [50]. As CMR can assess flow velocities, in addition to pressure indices, a prospective study employing MRI-derived PI would likely enable superior quantification of pulsatility: an interesting arena for future-related work.
This study was limited by its retrospective nature. Likewise, the functionally univentricular heart represents a highly heterogeneous group of complex defects, and therefore, the effects of pulsatile pulmonary flow on one specific anatomic substrate might not be generalizable to a morphologically different single ventricle. Inclusion of those patients with HLHS might also introduce bias since none of these would have forward flow at any point. They were retained in order to provide larger groups for comparison, and with larger numbers of patients in each group, they might be omitted in a future study. Analysis of larger subgroups of UVH patients, over a longer timeframe, is necessary to elucidate specific defects which may respond more favorably to pulsatile blood flow; this would ultimately enable evidence-based risk stratification and management.
Availability of Data and Materials
This manuscript reports original results. Individual participant data will not be made available at a later date.
References
Baumgartner H, Bonhoeffer P, De Groot NM, de Haan F, Deanfield JE, Galie N et al (2010) ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 31(23):2915–2957
O’Leary PW (2002) Prevalence, clinical presentation and natural history of patients with single ventricle. Prog Pediatr Cardiol 16(1):31–38
d’Udekem Y, Iyengar AJ, Cochrane AD, Grigg LE, Ramsay JM, Wheaton GR et al (2007) The Fontan procedure: contemporary techniques have improved long-term outcomes. Circulation 116(11 Suppl):I157–I164
Tweddell JS, Nersesian M, Mussatto KA, Nugent M, Simpson P, Mitchell ME et al (2009) Fontan palliation in the modern era: factors impacting mortality and morbidity. Ann Thorac Surg 88(4):1291–1299
Dabal RJ, Kirklin JK, Kukreja M, Brown RN, Cleveland DC, Eddins MC et al (2014) The modern Fontan operation shows no increase in mortality out to 20 years: a new paradigm. J Thorac Cardiovasc Surg 148(6):2517–23.e1
Pundi KN, Johnson JN, Dearani JA, Li Z, Hinck CA, Dahl SH et al (2015) 40-year follow-up after the Fontan operation: long-term outcomes of 1,052 patients. J Am Coll Cardiol 66(15):1700–1710
Atz AM, Zak V, Mahony L, Uzark K, D’Agincourt N, Goldberg DJ et al (2017) Longitudinal outcomes of patients with single ventricle after the Fontan procedure. J Am Coll Cardiol 69(22):2735–2744
d’Udekem Y, Iyengar AJ, Galati JC, Forsdick V, Weintraub RG, Wheaton GR et al (2014) Redefining expectations of long-term survival after the Fontan procedure: twenty-five years of follow-up from the entire population of Australia and New Zealand. Circulation 130(11 Suppl 1):S32–S38
Gewillig M (2005) The Fontan circulation. Heart 91:839–46
Rychik J (2016) The relentless effects of the Fontan paradox. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 19(1):37–43
Clift P, Celermajer D (2016) Managing adult Fontan patients: where do we stand? Eur Respir Rev 25(142):438–450
Zimmermann WH, Cesnjevar R (2009) Cardiac tissue engineering: implications for pediatric heart surgery. Pediatr Cardiol 30:716–23
Knott-Craig CJ, Danielson GK, Schaff HV, Puga FJ, Weaver AL, Driscoll DD (1995) The modified Fontan operation. An analysis of risk factors for early postoperative death or takedown in 702 consecutive patients from one institution. J Thorac Cardiovasc Surg 109(6):1237–43
Gentles TL, Mayer JE Jr, Gauvreau K, Newburger JW, Lock JE, Kupferschmid JP et al (1997) Fontan operation in five hundred consecutive patients: factors influencing early and late outcome. J Thorac Cardiovasc Surg 114(3):376–391
Egbe AC, Connolly HM, Miranda WR, Ammash NM, Hagler DJ, Veldtman GR et al (2017) Hemodynamics of Fontan failure: the role of pulmonary vascular disease. Circ Heart Fail. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004515
Gewillig M, Brown SC (2016) The Fontan circulation after 45 years: update in physiology. Heart 102:1081–6
Ovroutski S, Ewert P, Alexi-Meskishvili V, Holscher K, Miera O, Peters B et al (2009) Absence of pulmonary artery growth after Fontan operation and its possible impact on late outcome. Ann Thorac Surg 87(3):826–831
Gewillig M, Brown SC, Heying R, Eyskens B, Ganame J, Boshoff DE et al (2010) Volume load paradox while preparing for the Fontan: not too much for the ventricle, not too little for the lungs. Interact Cardiovasc Thorac Surg 10(2):262–265
Khambadkone S, Li J, de Leval MR, Cullen S, Deanfield JE, Redington AN (2003) Basal pulmonary vascular resistance and nitric oxide responsiveness late after Fontan-type operation. Circulation 107(25):3204–3208
Davies RR, Pizarro C (2015) Decision-making for surgery in the management of patients with univentricular heart. Front Pediatr. https://doi.org/10.3389/fped.2015.00061
Kobayashi J, Matsuda H, Nakano S, Shimazaki Y, Ikawa S, Mitsuno M et al (1991) Hemodynamic effects of bidirectional cavopulmonary shunt with pulsatile pulmonary flow. Circulation 84(5 Suppl):Iii219–Iii225
McElhinney DB, Marianeschi SM, Reddy VM (1998) Additional pulmonary blood flow with the bidirectional Glenn anastomosis: does it make a difference? Ann Thorac Surg 66(2):668–672
Berdat PA, Belli E, Lacour-Gayet F, Planche C, Serraf A (2005) Additional pulmonary blood flow has no adverse effect on outcome after bidirectional cavopulmonary anastomosis. Ann Thorac Surg 79(1):29–36; discussion-7
Uemura H, Yagihara T, Kawashima Y, Okada K, Kamiya T, Anderson RH (1995) Use of the bidirectional Glenn procedure in the presence of forward flow from the ventricles to the pulmonary arteries. Circulation 92(9 Suppl):Ii228–Ii232
Caspi J, Pettitt TW, Ferguson TB Jr, Stopa AR, Sandhu SK (2003) Effects of controlled antegrade pulmonary blood flow on cardiac function after bidirectional cavopulmonary anastomosis. Ann Thorac Surg 76(6):1917–21; discussion 21–2
Yoshida M, Yamaguchi M, Yoshimura N, Murakami H, Matsuhisa H, Okita Y (2005) Appropriate additional pulmonary blood flow at the bidirectional Glenn procedure is useful for completion of total cavopulmonary connection. Ann Thorac Surg 80(3):976–981
Gray RG, Altmann K, Mosca RS, Prakash A, Williams IA, Quaegebeur JM et al (2007) Persistent antegrade pulmonary blood flow post-Glenn does not alter early post-Fontan outcomes in single-ventricle patients. Ann Thorac Surg 84(3):888–93; discussion 93
Zhang T, Shi Y, Wu K, Hua Z, Li S, Hu S et al (2016) Uncontrolled antegrade pulmonary blood flow and delayed Fontan completion after the bidirectional Glenn procedure: real-world outcomes in China. Ann Thorac Surg 101(4):1530–1538
Seliem MA, Baffa JM, Vetter JM, Chen SL, Chin AJ, Norwood WI Jr (1993) Changes in right ventricular geometry and heart rate early after hemi-Fontan procedure. Ann Thorac Surg 55(6):1508–1512
Mandelbaum I, Burns WH (1965) Pulsatile and nonpulsatile blood flow. Jama 191:657–660
Raj JU, Kaapa P, Anderson J (1992) Effect of pulsatile flow on microvascular resistance in adult rabbit lungs. J Appl Physiol 72(1):73–81
Chen Q, Tulloh R, Caputo M, Stoica S, Kia M, Parry AJ (2015) Does the persistence of pulsatile antegrade pulmonary blood flow following bidirectional Glenn procedure affect long term outcome? Eur J Cardiothorac Surg 47(1):154–8; discussion 8
Ross RD, Daniels SR, Schwartz DC, Hannon DW, Shukla R, Kaplan S (1987) Plasma norepinephrine levels in infants and children with congestive heart failure. Am J Cardiol 59(8):911–914
Wallace MC, Jaggers J, Li JS, Jacobs ML, Jacobs JP, Benjamin DK et al (2011) Center variation in patient age and weight at Fontan operation and impact on postoperative outcomes. Ann Thorac Surg 91(5):1445–1452
Stewart RD, Pasquali SK, Jacobs JP, Benjamin DK, Jaggers J, Cheng J et al (2012) Contemporary Fontan operation: association between early outcome and type of cavopulmonary connection. Ann Thorac Surg 93(4):1254–60; discussion 61
Fontan F, Kirklin JW, Fernandez G, Costa F, Naftel DC, Tritto F et al (1990) Outcome after a “perfect” Fontan operation. Circulation 81(5):1520–1536
Khairy P, Fernandes SM, Mayer JE Jr, Triedman JK, Walsh EP, Lock JE et al (2008) Long-term survival, modes of death, and predictors of mortality in patients with Fontan surgery. Circulation 117(1):85–92
Kaapa P, Usha Raj J, Hillyard R, Anderson J (1991) Segmental vascular resistance during pulsatile and steady perfusion in 3- to 5-wk-old rabbit lungs. Am J Physiol 261(2 Pt 2):H506–H513
Henaine R, Vergnat M, Bacha EA, Baudet B, Lambert V, Belli E et al (2013) Effects of lack of pulsatility on pulmonary endothelial function in the Fontan circulation. J Thorac Cardiovasc Surg 146(3):522–529
Joannidès R, Bellien J, Thuillez C (2014) Pulsatile stress, arterial stiffness, and endothelial function. In: Safar ME, O’Rourke MF, Frohlich ED (eds) Blood pressure and arterial wall mechanics in cardiovascular diseases. Springer London, London, pp 107–21
Fredenburg TB, Johnson TR, Cohen MD (2011) The Fontan procedure: anatomy, complications, and manifestations of failure. Radiographics 31(2):453–463
Olofsson P, Laurini RN, Marsal K (1993) A high uterine artery pulsatility index reflects a defective development of placental bed spiral arteries in pregnancies complicated by hypertension and fetal growth retardation. Eur J Obstet Gynecol Reprod Biol 49(3):161–168
Rimoy GH, Bhaskar NK, Rubin PC (1991) Reproducibility of Doppler blood flow velocity waveform measurements: study on variability within and between day and during haemodynamic intervention in normal subjects. Eur J Clin Pharmacol 41(2):125–129
Palecek T, Jansa P, Ambroz D, Hlubocka Z, Horak J, Skvarilova M et al (2011) Are pulmonary artery pulsatility indexes able to differentiate chronic pulmonary thromboembolism from pulmonary arterial hypertension? An echocardiographic and catheterization study. Heart Vessels 26(2):176–182
Morine K, Kiernan M, Kapur N, Baumgartner R, Pham D, Denofrio D (2013) Pulmonary artery pulsatility index as a novel marker of right ventricular failure following LVAD surgery. J Cardiac Fail 19(8):S17
Shabanian R, Mirzaaghayan MR, Dadkhah M, Hosseini M, Rahimzadeh M, Akbari Asbagh P et al (2015) Echocardiographic assessment of pulmonary arteries pulsatility index in Fontan circulation. J Cardiovasc Ultrasound 23(4):228–232
Klimes K, Abdul-Khaliq H, Ovroutski S, Hui W, Alexi-Meskishvili V, Spors B et al (2007) Pulmonary and caval blood flow patterns in patients with intracardiac and extracardiac Fontan: a magnetic resonance study. Clin Res Cardiol 96(3):160–167
Brown DW, Powell AJ, Geva T (2010) Imaging complex congenital heart disease—functional single ventricle, the Glenn circulation and the Fontan circulation: a multimodality approach. Prog Pediatr Cardiol 28(1):45–58
Undar A, Fraser CD Jr (2002) The alphabet of research on pulsatile and nonpulsatile (continuous flow) perfusion during chronic support. Artif Organs 26(9):812–813
Shepard RB, Simpson DC, Sharp JF (1966) Energy equivalent pressure. Arch Surg 93(5):730–740
Funding
The British Heart Foundation and the Cardio-vascular theme of NIHR Bristol Biomedical Research Centre supported this work. The funders played no role in the design of the study, in the collection, analysis, and interpretation of data, or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant affiliations or financial involvement with any commercial organization with a financial interest in or financial conflict with the subject matter discussed in the manuscript. No writing assistance was sought to produce this manuscript.
Ethical Approval
Formal ethical Committee approval was waived given the retrospective anonymized study design.
Informed Consent
Written informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kalia, K., Walker-Smith, P., Ordoñez, M.V. et al. Does Maintenance of Pulmonary Blood Flow Pulsatility at the Time of the Fontan Operation Improve Hemodynamic Outcome in Functionally Univentricular Hearts?. Pediatr Cardiol 42, 1180–1189 (2021). https://doi.org/10.1007/s00246-021-02599-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02599-w