Abstract
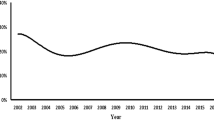
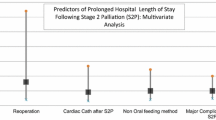
Patients with hypoplastic left heart syndrome (HLHS) can have associated genetic abnormalities. This study evaluated the incidence of genetic abnormalities among infants with HLHS and the short-term outcomes of this population during the first hospitalization. This is a retrospective analysis of the multi-center Pediatric Heath Information System database of infants with HLHS who underwent Stage I Norwood, Hybrid, or heart transplant during their first hospitalization from 2004 through 2013. We compared clinical data between infants with and without genetic abnormality, among the three most common chromosomal abnormalities, and between survivors and non-survivors. Multivariable analysis was completed to evaluate predictors of mortality among patients with genetic abnormalities. A total of 5721 infants with HLHS were identified; 282 (5%) had associated genetic abnormalities. The three most common chromosomal abnormalities were Turner (25%), DiGeorge (22%), and Downs (12.7%) syndromes. Over the study period, the number of patients with genetic abnormalities undergoing cardiac operations increased without any significant increases in mortality. Infants with genetic abnormalities compared to those without abnormalities had longer hospital length of stay and higher morbidity and mortality. Variables associated with mortality were lower gestational age, longer duration of vasopressor therapy, need for dialysis, and cardiopulmonary resuscitation; and complicated clinical course as suggested by necrotizing enterocolitis, septicemia. Presence of any genetic abnormality in infants with HLHS undergoing cardiac surgery is associated with increased mortality and morbidity. Timely genetic testing, appropriate family counseling, and thorough preoperative case selection are suggested for these patients for any operative intervention.

Similar content being viewed by others
References
Morris CD, Outcalt J, Menashe VD (1990) Hypoplastic left heart syndrome: natural history in a geographically defined population. Pediatrics 85:977–983
Ferencz C, Rubin JD, McCarter RJ, Brenner JI, Neill CA, Perry LW, Hepner SI, Downing JW (1985) Congenital heart disease: prevalence at livebirth. The Baltimore-Washington infant study. Am J Epidemiol 121:31–36
Lurie IW, Kappetein AP, Loffredo CA, Ferencz C (1995) Non-cardiac malformations in individuals with outflow tract defects of the heart: the Baltimore-Washington infant study (1981-1989). Am J Med Genet 59:76–84
Tennstedt C, Chaoui R, Körner H, Dietel M (1999) Spectrum of congenital heart defects and extracardiac malformations associated with chromosomal abnormalities: results of a seven year necropsy study. Heart 82:34–39
Loffredo CA, Chokkalingam A, Sill AM, Boughman JA, Clark EB, Scheel J, Brenner JI (2004) Prevalence of congenital cardiovascular malformations among relatives of infants with hypoplastic left heart, coarctation of the aorta, and d-transposition of the great arteries. Am J Med Genet A 124:225–230
Hinton RB, Martin LJ, Rame-Gowda S, Tabangin ME, Cripe LH, Benson DW (2009) Hypoplastic left heart syndrome links to chromosomes 10q and 6q and is genetically related to bicuspid aortic valve. J Am Coll Cardiol 53:1065–1071
Allen RH, Benson C, Haug LW (2005) Pregnancy outcome of fetuses with a diagnosis of hypoplastic left ventricle on prenatal sonography. J Ultrasound Med 24:1199–1203
Warburton D, Ronemus M, Kline J et al (2014) The contribution of de novo and rare inherited copy number changes to congenital heart disease in an unselected sample of children with conotruncal defects or hypoplastic left heart disease. Hum Genet 133:11–27
Bensemlali M, Bajolle F, Ladouceur M, Fermont L, Lévy M, Le Bidois J, Salomon LJ, Bonnet D (2016) Associated genetic syndromes and extracardiac malformations strongly influence outcomes of fetuses with congenital heart diseases. Arch Cardiovasc Dis 109:330–336
Carey AS, Liang L, Edwards J et al (2013) Effect of copy number variants on outcomes for infants with single ventricle heart defects. Circ Cardiovasc Genet. 6:444–451
Stasik CN, Goldberg CS, Bove EL, Devaney EJ, Ohye RG (2006) Current outcomes and risk factors for the Norwood procedure. J Thorac Cardiovasc Surg 131:412–417
Jacobs JP, O’Brien S, Chai P, Morell V, Lindberg HL, Quintessenza JA (2008) Management of 239 patients with hypoplastic left heart syndrome and related malformations from 1993 to 2007. Ann Thorac Surg 85:1691–1697
Patel A, Hickey E, Mavroudis C, Jacobs JP, Jacobs ML, Backer CL, Gevitz M, Mavroudis CD (2010) Impact of noncardiac congenital and genetic abnormalities on outcomes in hypoplastic left heart syndrome. Ann Thorac Surg 89:1805–1814
Tabbutt S, Ghanayem N, Ravishankar C et al (2012) Pediatric heart network investigators. risk factors for hospital morbidity and mortality after the Norwood procedure: a report from the pediatric heart network single ventricle reconstruction trial. J Thorac Cardiovasc Surg 144:882–895
Lara DA, Ethen MK, Canfield MA, Nembhard WN, Morris SA (2017) A population-based analysis of mortality in patients with Turner syndrome and hypoplastic left heart syndrome using the Texas Birth Defects Registry. Congenit Heart Dis 12:105–112
van Egmond H, Orye E, Praet M, Coppens M, Devloo-Blancquaert A (1988) Hypoplastic left heart syndrome and 45X karyotype. Br Heart J 60:69–71
Reis PM, Punch MR, Bove EL, van de Ven CJ (1999) Outcome of infants with hypoplastic left heart and Turner syndromes. Obstet Gynecol 93:532–535
Atton G, Gordon K, Brice G, Keeley V, Riches K, Ostergaard P, Mortimer P, Mansour S (2015) The lymphatic phenotype in Turner syndrome: an evaluation of nineteen patients and literature review. Eur J Hum Genet 23:1634–1639
Evans JM, Dharmar M, Meierhenry E, Marcin JP, Raff GW (2014) Association between Down syndrome and in-hospital death among children undergoing surgery for congenital heart disease: a US population-based study. Circ Cardiovasc Qual Outcomes 7:445–45219
Fudge JC Jr, Li S, Jaggers J, O’Brien SM, Peterson ED, Jacobs JP, Welke KF, Jacobs ML, Li JS, Pasquali SK (2010) Congenital heart surgery outcomes in Down syndrome: analysis of a national clinical database. Pediatrics 126:315–322
Marmon LM, Balsara RK, Chen R, Dunn JM (1984) Congenital cardiac anomalies associated with the DiGeorge syndrome: a neonatal experience. Ann Thorac Surg 38:146–150
O’Byrne ML, Yang W, Mercer-Rosa L, Parnell AS, Oster ME, Levenbrown Y, Tanel RE, Goldmuntz E (2014) 22q11.2 deletion syndrome is associated with increased perioperative events and more complicated postoperative course in infants undergoing infant operative correction of truncus arteriosus communis or interrupted aortic arch. J Thorac Cardiovasc Surg 148:1597–1605
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informal Consent
This is a retrospective study and formal consent is not required.
Research Involving Human and Animal Participants
This article does not contain any studies with animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zakaria, D., Tang, X., Bhakta, R. et al. Chromosomal Abnormalities Affect the Surgical Outcome in Infants with Hypoplastic Left Heart Syndrome: A Large Cohort Analysis. Pediatr Cardiol 39, 11–18 (2018). https://doi.org/10.1007/s00246-017-1717-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1717-3