Abstract
Neonates with single-ventricle physiology are at increased risk of developing gastrointestinal morbidities. Feeding protocols in this patient population have been shown to decrease feeding complications after the Norwood procedure, but no data exist to determine the effectiveness of a feeding protocol in patients undergoing the hybrid procedure. Goal of this study was to examine the impact of a standardized feeding protocol on the incidence of overall postoperative gastrointestinal morbidity after the hybrid procedure. Retrospective chart review was performed on neonates undergoing the hybrid procedure. Neonates were divided into two groups, pre-feeding protocol (pre-FP), which encompassed the years 2002–2008, and post-feeding protocol (post-FP), which encompassed the years 2011–2014. Preoperative, operative, and postoperative data were collected. T test or Fisher’s exact test was used for analysis. p < 0.05 was considered significant. Seventy-three neonates were in the pre-FP and 52 neonates were in the post-FP. There were no significant differences between the pre-FP and the post-FP in cardiac diagnosis (62 HLHS, 11 other vs. 39 HLHS, 13 other, respectively). Pre-FP underwent hybrid procedure later than the post-FP (9.1 ± 5.8 vs. 5.7 ± 3.4 days, respectively, p < 0.01) and achieved full enteral feeds earlier than the post-FP (3.2 + 2.9 vs. 7.8 + 3.9 days, respectively, p < 0.01). The incidence of necrotizing enterocolitis was higher in the pre-FP versus post-FP [11.0 % (8/65) vs. 5.8 % (3/49), respectively, p = 0.36]. Though not significant, the incidence of necrotizing enterocolitis decreased by almost 50 % after initiating a feeding protocol in patients undergoing the hybrid procedure. This is consistent with previous studies showing beneficial results of a feeding protocol in this complex patient population.
Similar content being viewed by others
Introduction
Neonates with single-ventricle physiology (SVP) are at increased risk of gastrointestinal complications such as necrotizing enterocolitis (NEC) during their initial hospitalization regardless of initial surgical palliative procedure [11, 18, 23, 24]. The causes for these gastrointestinal complications are likely multifactorial, but the underlying physiology undoubtedly plays a role [6, 24, 25]. Mortality rates in infants who develop NEC without congenital heart disease (CHD) have been reported to be in the 5–12 % range, but mortality is even higher in infants with CHD [8, 18, 20, 23]. Thus, NEC is a significant cause of morbidity and mortality in patients with CHD, particularly in neonates with SVP.
Recently, the initiation of feeding protocols has been reported to decrease gastrointestinal complications in neonates with SVP undergoing the Norwood procedure [4, 13, 31]. The hybrid procedure is an alternative to the Norwood procedure for initial palliation of patients with SVP [15, 35]. Despite the fact that the hybrid procedure is less invasive than the Norwood procedure, the incidence of NEC after the hybrid procedure appears to be similar or higher to previously published results [11, 12, 20, 23]. However, the prior reports in patients undergoing the hybrid procedure occurred before there was a specific feeding protocol in place for these patients [25].
The goal of this study was to examine the gastrointestinal outcomes pre- and post-initiation of a feeding protocol in patients undergoing the hybrid procedure.
Methods
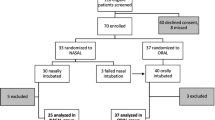
IRB approval was obtained for this retrospective chart review study performed at a tertiary pediatric hospital. All neonates who underwent the hybrid procedure for palliation of complex CHD from April 2002 through April 2008, pre-feeding protocol (pre-FP) and December 2011 through November 2014, post-feeding protocol (post-FP), were reviewed. Feeding protocols are presented in Appendix 1 and 2. In general, the protocol introduced followed similar formats that have been previously published with changes based on institutional preferences [4, 13]. The earlier cohort has been previously described and this group acted as a control group of convenience [23]. The 3-year gap between the two cohorts consisted of the planning and initiating of a fully implemented feeding protocol. Patients were excluded from the study if they underwent the initial procedure at >30 days of life, were transferred to our institution at >2 weeks of age (feeding and radiology records were incomplete), were transferred out of our institution at <5 days post-procedure (before full enteral feeds were established), or had multiple congenital anomalies preventing enteral feeding [23].
Demographic, perinatal, perioperative, clinical, and procedural data were collected for the two groups. NEC was defined as Bells Stage II or above [3]. By utilizing Bell’s Stage II and above (moderate-to-severe NEC), the subjective discrepancy of whether a patient merely had feeding intolerance versus early-stage NEC was minimized. In addition, this allowed for a more objective measurement (pneumatosis on radiograph) in combination with clinical presentation to aid in the diagnosis.
Pregnancy and perinatal factors analyzed included maternal age, prenatal care (documentation of any prenatal evaluation by an obstetrician and/or a prenatal ultrasound), prenatal diagnosis of CHD, mode of delivery (vaginal vs. cesarean section), Apgar scores, and resuscitation in the delivery room (defined as requiring supplemental oxygen, continuous positive airway pressure, positive pressure ventilation, intubation, chest compressions, and/or resuscitation medications). In addition, patient demographics, such as gender, gestational age, birth weight, and CHD diagnosis, were also reviewed.
Pre-procedure and procedure variables analyzed included ventilation at any time before the procedure, ventilation at the time of procedure, use of subambient oxygen, maximum dose of prostaglandin infusion (μg/kg/min), presence of umbilical venous and arterial catheters, enteral feeding before procedure (including formula vs. human milk), inotrope use, maximum inotrope score in μg/kg/min (dobutamine + dopamine + 100 × epinephrine + 100 × norepinephrine + 10 × milrinone) [33, 34], and laboratory analysis of blood values, including lowest pH, highest hematocrit, lowest platelet count, highest lactate, renal insufficiency (creatinine of >1.5 mg/dL), and liver insufficiency (aspartate transaminase or alanine aminotransferase of >250 U/L), need for urgent balloon atrial septostomy before hybrid procedure, and age at hybrid procedure.
Post-procedure and intensive care unit course were also reviewed to analyze variables, such as inotrope use, maximum inotrope score, length of time on ventilator (h), average oxygen saturation and diastolic blood pressure for the first 24 h post-procedure, time to initiate enteral feeds (days), time to reach full enteral feeds (120 mL/kg/day), abdominal radiograph findings, abdominal and feeding findings, NEC diagnosis, culture proven infection (blood, trachea, urine, or wound), length of hospitalization, and mortality.
Patients were divided into pre-FP and post-FP groups. T test or Fisher’s exact test was used for analysis as appropriate. p < 0.05 was considered significant.
Results
The pre-FP consisted of 73 patients and the post-FP consisted of 52 patients. Prenatal, demographic, and CHD diagnosis are presented in Table 1. Maternal age and gestational age were significantly lower in the pre-FP versus post-FP. In addition, the incidence of prenatal diagnosis of CHD was significantly lower in the pre-FP. There were no other variables with significant differences in this category.
Perinatal and pre-procedure variables are presented in Table 2. The pre-FP was more likely to be intubated prior to the hybrid procedure and have a higher lactate and maximum inotrope score than the post-FP. Umbilical venous catheters were less used in the pre-FP, and the maximum prostaglandin dose was higher in the pre-FP. Other perinatal and pre-procedure variables were not significantly different between the two groups.
Procedure and post-procedure variables are presented in Table 3. Age at hybrid was significantly older in the pre-FP. Inotrope use was less frequent post-hybrid procedure, and time to full feeds was shorter in the pre-FP. Though not significant, the incidence of abdominal distension, gastrostomy tubes, and necrotizing enterocolitis was higher in the pre-FP versus post-FP.
Discussion
Gastrointestinal morbidities remain a concern in SVP patients undergoing palliation in the neonatal time period. NEC remains the most concerning gastrointestinal morbidity in this patient population. Previous studies have reported improved gastrointestinal outcomes after instituting a feeding protocol in SVP neonates undergoing the Norwood procedure [4, 13, 20]. No data exist describing the impact of a feeding protocol in SVP patients undergoing the hybrid procedure. In this study, though not significant, the incidence of abdominal distension, gastrostomy placement, and NEC were reduced in the post-FP compared to the pre-FP.
Adequate nutritional support is an important part of care in critically ill pediatric patients [5, 22]. Despite improvement in mortality for SVP, gastrointestinal morbidities remain a significant issue in the neonatal time period [16, 20, 24]. Multiple issues may prevent timely and adequate nutritional support when in the intensive care unit, including, but not limited to, multiple interruptions in feeds due to hemodynamic or procedural concerns, fluid restrictions, individual practice variation, and other unknown factors [19, 27, 29]. Feeding protocols have been shown to be beneficial for patients in the critical care setting by overcoming many of these obstacles [1, 26, 30]. As stated above, this has also been shown to be the case in SVP undergoing the Norwood procedure, and similar results are now reported in this paper after the hybrid procedure [4, 13].
The hybrid procedure is an alternative palliative procedure for patients with SVP [2, 15]. Though the hybrid procedure is not as extensive a surgical procedure compared to the Norwood procedure, it is associated with diastolic reversal of flow in the descending aorta similar to the Norwood procedure with a modified Blalock–Taussig shunt [9, 25]. This abnormal flow pattern may subsequently affect the celiac and superior mesenteric blood flows in neonates with SVP, regardless whether they have undergone the Norwood or hybrid procedure [10, 17, 21]. This abnormal mesenteric flow pattern may theoretically put these patients at increased risk of gastrointestinal morbidities such as feeding intolerance or NEC. Risk factors for NEC in patients undergoing the Norwood procedure have been previously noted to be lower weight, later attainment of full feedings, increased positive blood cultures, greater risk of mortality (PRISM) score, and a larger Blalock–Taussig shunt when indexed to body weight [16, 20].
The incidence of NEC in the hybrid population was previously reported to be 11 % prior to a feeding protocol being instituted [23]. Older reports document a median incidence of NEC to be 18 % (range 11–20 %) in patients undergoing the Norwood procedure [16]. This is consistent with more recent reports documenting the incidence of NEC status post Norwood procedure of 11 % by Braudis et al. [4] and 15 % by del Castillo et al. (Bell Stage ≥ II) [13] prior to a feeding protocol being started. After instituting a feeding protocol, Braudis et al. reported 0 % occurrence of NEC. However, that report excluding high-risk patients such as neonates born less than 35 weeks gestational age or having weight less than 2 kg. They also excluded neonates who died during the hospitalization. This report included those patients and thus may partially explain the differences in incidence of NEC between these two studies. del Castillo reported a decrease in NEC in their post-FP to 4.3 % (Bell Stage ≥ II), which is similar to 5.8 % in this study. Though not significant, this was close to a 50 % decrease in the incidence of NEC in the post-FP. To obtain statistical significance, an “n” of 108 patients in the post-FP would have been required necessitating 3–4 additional years of data collection. This was not thought to be practically feasible. The etiology of NEC is no doubt multifactorial, but these data suggest that a feeding protocol may have some beneficial results concerning this issue.
Similarly, additional gastrointestinal issues such as abdominal distension and gastrostomy tube use decreased in the post-FP group, though not significantly. However, other gastrointestinal issues such as emesis, bloody stool, and time to initiate enteral feeds were essentially unchanged. Furthermore, length of hospital stay and overall mortality were unchanged between groups. The time to reach full feeds was 7.8 ± 3.9 days in the post-FP, which was statistically longer than the pre-FP of 3.3 ± 2.9 days. This is likely due to the more cautious advancement of feeds in the post-FP, whereas previously, advancement of feeds was at physician’s discretion and may have occurred rapidly. However, this is consistent with the 9 days by Braudis et al. [4] and the 7 days by Toms et al. [31] to reach full enteral feeds in their SVP patients. Incidence of inotrope use was also statistically higher in the post-FP. There is no set protocol in the intensive care unit regarding inotrope use in these patients. Prophylactic use may have been more prevalent in the recent cohort, and we cannot rule out that his may have also lessened gastrointestinal issues in this population.
The preoperative and operative variables were not totally analogous between the two groups. Maternal age and gestational age of the neonate were older in the post-FP. This is consistent with trends of an older maternal age in the general population as well as the goal of delivery as close to term as possible [7]. In addition, the data suggest that the pre-FP were possibly more ill than the post-FP preoperatively. The pre-FP was more likely to be intubated before the hybrid procedure, have a higher inotrope score, and have a higher lactate level. This may be due to the fact that the pre-FP was less likely to have a prenatal diagnosis of a CHD. Thus, these patients probably presented in extremis and required stabilization of hemodynamics before proceeding to the hybrid procedure [28, 32]. This would also explain the older age at hybrid procedure in the pre-FP. That being said, other signs of end organ function/dysfunction such lowest pH, incidence of liver and renal insufficiency, and ability to feed enterally prior to the hybrid procedure were similar between the groups. It is not known how these differences may have affected the gastrointestinal issues postoperatively.
There are multiple limitations to this study. This was a retrospective study with all the inherent problems associated with such a design. The two groups were not totally analogous, and this may have affected the post-procedure variables. Significance was not found in the main gastrointestinal outcomes, only qualitative changes. This is probably due to the relatively small “n” able to be analyzed, though it is the largest reported to date. The time frame evaluated was over 12 years, so changes in preoperative, operative, and postoperative care may have also affected the post-procedure variables [14, 15]. However, despite the time frame evaluated, many of the preoperative and operative variables were similar between the two groups. In addition, hemodynamic parameters such as diastolic blood pressures and systemic oxygen saturation were comparable between groups, suggesting that the groups may not have been too disparate.
In conclusion, though not significant, the incidence of necrotizing enterocolitis decreased by almost 50 % after initiating a feeding protocol in SVP undergoing the hybrid procedure. This is consistent with previous studies showing beneficial results of a feeding protocol in this complex patient population.
References
Adam S (2000) Standardization of nutritional support: Are protocols useful? Intensive Crit Care Nurs 16:283–289
Akintuerk H, Michel-Behnke I, Valeske K et al (2002) Stenting of the arterial duct and banding of the pulmonary arteries: basis for combined Norwood stage I and II repair in hypoplastic left heart. Circulation 105:1099–1103
Bell MJ, Ternberg JL, Feigin RD et al (1978) Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 187:1–7
Braudis NJ, Curley MA, Beaupre K et al (2009) Enteral feeding algorithm for infants with hypoplastic left heart syndrome poststage I palliation. Pediatr Crit Care Med 10:460–466
Briassoulis G, Zavras N, Hatzis T (2001) Malnutrition, nutritional indices, and early enteral feeding in critically ill children. Nutrition 17:548–557
Carlo WF, Kimball TR, Michelfelder EC, Border WL (2007) Persistent diastolic flow reversal in abdominal aortic Doppler-flow profiles is associated with an increased risk of necrotizing enterocolitis in term infants with congenital heart disease. Pediatrics 119:330–335
Costello JM, Pasquali SK, Jacobs JP et al (2014) Gestational age at birth and outcomes after neonatal cardiac surgery: an analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Circulation 129:2511–2517
Cozzi C, Aldrink J, Nicol K, Nicholson L, Cua C (2013) Intestinal location of necrotizing enterocolitis among infants with congenital heart disease. J Perinatol 33:783–785
Cozzi C, Stines J, Luce WA et al (2013) Diastolic flow parameters are not sensitive in predicting necrotizing enterocolitis in patients undergoing hybrid procedure. Congenit Heart Dis 8:234–239
Cozzi CT, Galantowicz M, Cheatham JP et al (2015) Ultrasound assessment of mesenteric blood flow in neonates with hypoplastic left heart before and after hybrid palliation. Cardiol Young 25:1074–1079
Cua CL, Thiagarajan RR, Gauvreau K et al (2006) Early postoperative outcomes in a series of infants with hypoplastic left heart syndrome undergoing stage I palliation operation with either modified Blalock–Taussig shunt or right ventricle to pulmonary artery conduit. Pediatr Crit Care Med 7:238–244
Davies RR, Carver SW, Schmidt R, Keskeny H, Hoch J, Pizarro C (2013) Gastrointestinal complications after stage I Norwood versus hybrid procedures. Ann Thorac Surg 95:189–195 (discussion 195–196)
del Castillo SL, McCulley ME, Khemani RG et al (2010) Reducing the incidence of necrotizing enterocolitis in neonates with hypoplastic left heart syndrome with the introduction of an enteral feed protocol. Pediatr Crit Care Med 11:373–377
Galantowicz M, Cheatham JP (2005) Lessons learned from the development of a new hybrid strategy for the management of hypoplastic left heart syndrome. Pediatr Cardiol 26:190–199
Galantowicz M, Cheatham JP, Phillips A et al (2008) Hybrid approach for hypoplastic left heart syndrome: intermediate results after the learning curve. Ann Thorac Surg 85:2063–2070 (discussion 2070–2071)
Golbus JR, Wojcik BM, Charpie JR, Hirsch JC (2011) Feeding complications in hypoplastic left heart syndrome after the Norwood procedure: a systematic review of the literature. Pediatr Cardiol 32:539–552
Harrison AM, Davis S, Reid JR et al (2005) Neonates with hypoplastic left heart syndrome have ultrasound evidence of abnormal superior mesenteric artery perfusion before and after modified Norwood procedure. Pediatr Crit Care Med 6:445–447
Hebra A, Brown MF, Hirschl RB et al (1993) Mesenteric ischemia in hypoplastic left heart syndrome. J Pediatr Surg 28:606–611
Heyland D, Cook DJ, Winder B, Brylowski L, Van deMark H, Guyatt G (1995) Enteral nutrition in the critically ill patient: a prospective survey. Crit Care Med 23:1055–1060
Jeffries HE, Wells WJ, Starnes VA, Wetzel RC, Moromisato DY (2006) Gastrointestinal morbidity after Norwood palliation for hypoplastic left heart syndrome. Ann Thorac Surg 81:982–987
Johnson JN, Ansong AK, Li JS et al (2011) Celiac artery flow pattern in infants with single right ventricle following the Norwood procedure with a modified Blalock–Taussig or right ventricle to pulmonary artery shunt. Pediatr Cardiol 32:479–486
Kelleher DK, Laussen P, Teixeira-Pinto A, Duggan C (2006) Growth and correlates of nutritional status among infants with hypoplastic left heart syndrome (HLHS) after stage 1 Norwood procedure. Nutrition 22:237–244
Luce WA, Schwartz RM, Beauseau W et al (2011) Necrotizing enterocolitis in neonates undergoing the hybrid approach to complex congenital heart disease. Pediatr Crit Care Med 12:46–51
McElhinney DB, Hedrick HL, Bush DM et al (2000) Necrotizing enterocolitis in neonates with congenital heart disease: risk factors and outcomes. Pediatrics 106:1080–1087
Miller TA, Minich LL, Lambert LM, Joss-Moore L, Puchalski MD (2014) Abnormal abdominal aorta hemodynamics are associated with necrotizing enterocolitis in infants with hypoplastic left heart syndrome. Pediatr Cardiol 35:616–621
Petrillo-Albarano T, Pettignano R, Asfaw M, Easley K (2006) Use of a feeding protocol to improve nutritional support through early, aggressive, enteral nutrition in the pediatric intensive care unit. Pediatr Crit Care Med 7:340–344
Rogers EJ, Gilbertson HR, Heine RG, Henning R (2003) Barriers to adequate nutrition in critically ill children. Nutrition 19:865–868
Satomi G, Yasukochi S, Shimizu T, Takigiku K, Ishii T (1999) Has fetal echocardiography improved the prognosis of congenital heart disease? Comparison of patients with hypoplastic left heart syndrome with and without prenatal diagnosis. Pediatr Int 41:728–732
Spain DA, McClave SA, Sexton LK et al (1999) Infusion protocol improves delivery of enteral tube feeding in the critical care unit. JPEN J Parenter Enteral Nutr 23:288–292
Sulzbach-Hoke LM, Gift AG (1995) Use of quality management to provide nutrition to intubated patients. Clin Nurse Spec CNS 9:248–251
Toms R, Jackson KW, Dabal RJ, Reebals CH, Alten JA (2015) Preoperative trophic feeds in neonates with hypoplastic left heart syndrome. Congenit Heart Dis 10:36–42
Tworetzky W, McElhinney DB, Reddy VM, Brook MM, Hanley FL, Silverman NH (2001) Improved surgical outcome after fetal diagnosis of hypoplastic left heart syndrome. Circulation 103:1269–1273
Wernovsky G, Wypij D, Jonas RA et al (1995) Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92:2226–2235
Yates AR, Dyke PC 2nd, Taeed R et al (2006) Hyperglycemia is a marker for poor outcome in the postoperative pediatric cardiac patient. Pediatr Crit Care Med 7:351–355
Yerebakan C, Murray J, Valeske K et al (2015) Long-term results of biventricular repair after initial Giessen hybrid approach for hypoplastic left heart variants. J Thorac Cardiovasc Surg 149:1112–1120 (discussion 1120e2–1122e2)
Author’s Contribution
Simsic, Backes, and Cua contributed to concept/design. Carpenito, Prusinski, Kirchner, Miao, and Luce analysed the data. Carpenito, Prusinski, Kirchner, Simsic, Miao, Luce, Cheatham, Galantowicz, Backes, and Cua revised and approved the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Appendices
Appendix 1

Appendix 2

Rights and permissions
About this article
Cite this article
Carpenito, KR., Prusinski, R., Kirchner, K. et al. Results of a Feeding Protocol in Patients Undergoing the Hybrid Procedure. Pediatr Cardiol 37, 852–859 (2016). https://doi.org/10.1007/s00246-016-1359-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1359-x