Abstract
Noninvasive ventilation is effective in respiratory failure from various etiologies. This study aimed to analyze the efficacy of noninvasive positive pressure ventilation (NPPV) in pediatric cardiac patients. NPPV was used (1) as an alternative means of respiratory support in patients with hypoxemic or hypercarbic respiratory failure or with signs of respiratory distress that were considered to require intubation; or (2) as a preventive measure in patients with high risk for extubation failure. Between 2008 and 2011, there were 107 episodes of NPPV use in 82 patients. Their median age was 57 days (range 1 day to 18 years), and weight was 4.1 kg (range 1.7–68). Within the first hour of NPPV, partial pressure of carbon dioxide/fraction of inspired oxygen (PaO 2/FiO 2) was significantly increased, and arterial pCO 2, and respiratory rate were decreased. This decrease in respiratory rate and increase in PaO 2/FiO 2 continued during the first 24 h of therapy, and pCO2 was decreased during the first 6 h. In 59.8 % of cases, NPPV was successfully used without the need for tracheal intubation. The Aristotle Basic Complexity score, presence of infection, residual cardiac defect, and pH <7.36 in the first hour were independent predictors of NPPV failure. We conclude that NPPV improved oxygenation and decreased respiratory effort in pediatric cardiac patients, 59.8 % of whom eventually did not receive intubation. A high-complexity surgical score, presence of infection, residual cardiac defect, and pH <7.36 in the first hour are predictors of NPPV failure, which occurs in most patients >24 h after the onset of therapy.
Similar content being viewed by others
Introduction
Noninvasive positive pressure ventilation (NPPV) has been increasingly used as a treatment for various forms of respiratory failure. However, the role of NPPV remains unclear in hypoxemic respiratory failure due to acute respiratory distress syndrome and acute lung injury and in cases of postextubation respiratory failure [1, 3, 8]. Controversy exists regarding the indications for NPPV in different clinical settings as well as the choice of interface in relation to the patient’s age and respiratory pathology, the recommended initial ventilatory modality, and the monitoring of patients [2, 26, 28].
In children with cardiac diseases, data on the use of NPPV are limited. There are a few case reports on the successful use of NPPV in infants with diaphragmatic paralysis [4, 16, 21]. Results from studies with a small number of children after cardiac surgery show 64–88 % success of noninvasive ventilation, which is lower than that reported in other patient populations [1–3, 8, 27, 29]. This may be because of a young patient age, hemodynamic instability, a high incidence of postextubation failure, and the presence of a genetic syndrome.
In our unit, nasal continuous positive airway pressure (N-CPAP) has been extensively used in neonates. However, if an older child requires greater ventilatory support than “high-flow oxygen,” or if N-CPAP is not sufficient support for a neonate, the patient is intubated. The software for noninvasive ventilation with pressure support/control mode was installed on our ventilators in 2008. Since this time, NPPV has been progressively applied in our patients.
The aims of this study were to evaluate clinical efficacy and the characteristics of NPPV and to identify predictive factors for NPPV failure in pediatric cardiac patients.
Materials and Methods
Patients and Intervention
A prospective observational study was performed in the pediatric cardiac intensive care unit from 2008 to 2011. The study was approved by the hospital Ethics Committee. The need for informed consent was waived because the attending physician considered NPPV a routine form of ventilation. NPPV was used (1) as an alternative means of respiratory support in patients with hypoxemic or hypercarbic respiratory failure or in those with signs of respiratory distress who were considered likely to require intubation; or (2) as a preventive measure in patients with high risk for extubation failure (patients with several episodes of postextubation respiratory failure and/or patients who had prolonged artificial ventilation).
NPPV with pressure support and/or pressure control mode was applied by a flow-triggered pressure assist-control ventilator (Servo-I; Maquet, Solna, Sweden). The starting ventilatory mode and further adjustments of the ventilator pressures and rates were made according to clinical need, patient comfort, and blood gas analysis. A nasogastric tube was used in all patients. The interface was chosen according to the child’s age and size to achieve comfort and avoid significant air leaks. Colloid dressings were placed on major pressure points to minimize skin injury.
All patients were continuously monitored by means of electrocardiography and pulse oximetry, and we measured respiratory rate, invasive systemic blood pressure and central venous pressure, and central and peripheral temperature. Intermittent observations of chest movements and comfort level and auscultation of breath sounds were performed. Blood gas analysis was performed according to the protocol (before initiating NPPV and at 1, 3, 6, 12, and 24 h of NPPV).
Data Collection
For each NPPV application, the following variables were collected: age, sex, body weight, presence of genetic syndrome, cause of acute respiratory failure and indication for NPPV, underlying cardiac disease, Risk Adjusted Congenital Heart Surgery (RACHS) score, Aristotle Basic Complexity (ABC) score (when applicable), presence of a significant residual cardiac defect and infection, need for surgical or catheterization intervention, time elapsed from last extubation (when applicable), time from admission to the unit, and mode of respiratory support before NPPV.
Patients with multiple NPPV episodes were considered individually because each episode requiring NPPV presented new variables, thus potentially affecting outcome. Most of the patients had undergone cardiac surgery. Therefore, they were intubated before the use of NPPV. For the purpose of the study, we defined postextubation failure as acute respiratory failure within 48 h of extubation.
The following data were collected prospectively before initiating NPPV and at 1, 3, 6, 12, and 24 h of NPPV: heart rate, systemic blood pressure, respiratory rate, blood gas analysis, the ratio of partial pressure of arterial oxygen/fraction of inspired oxygen (PaO 2/FiO2), and ventilatory settings. Data reviewed also included the total NPPV duration, type of interface, complications attributed to NPPV, use of sedatives, NPPV outcome, mortality, and causes of death.
Outcome Measurements
Our primary end point was success or failure of NPPV, which was defined as avoidance of or need for reintubation. The secondary end points were improvement in vital signs and blood gas parameters. The variables analyzed for determining success or failure are listed in Table 3.
Statistical Analysis
Continuous data are presented as the median (ranges) and categorical data as counts (frequency variable). Serial measurements were compared with paired Student t test. Chi-square test and logistic regression analysis were used in the univariate analysis of NPPV success. A value of p ≤ 0.05 was considered significant. Variables with p ≤ 0.1 found in univariate analysis were then entered into a nominal logistic regression model for NPPV success. Statistical analysis was performed using JMP 5.0.1a software (SAS).
Results
Patients
During the study period, there were 107 episodes of NPPV use in 82 pediatric cardiac patients. Baseline characteristics of included cases are listed in Table 1. Underlying cardiac disease was cyanotic in 49 (45.7 %) events and noncyanotic in 58 (54.3 %) events. Ninety-three (86.9 %) of the NPPV episodes occurred after cardiac surgery. The most common cardiac surgical procedures were ventricular septal defect closure (n = 9), aortic coarctation and aortic arch repair (n = 9), pulmonary arterial banding (n = 7), and modified Blalock–Taussig shunt placement (n = 6). In nonsurgical cases, the main causes of respiratory failure were infection (n = 7), congestive heart failure (n = 4), prematurity (n = 1), spastic bronchitis (n = 1), and oversedation (n = 1).
The main etiologies that contributed to respiratory insufficiency were cardiac failure (n = 32), infection (n = 26), chronic lung disease (n = 17), muscle fatigue (n = 10), diaphragm paralysis (n = 5), long-term mechanical ventilation (n = 7), oversedation (n = 4), atelectasis (n = 3), stridor (n = 1), hemorrhagic shock (n = 1), and pulmonary hypertension (n = 1).
Tachypnea, dyspnea, hypoxemia, and hypercapnia were present in 64, 57, 39, and 44 cases, respectively. In 20 events, NPPV was used as a preventive measure for high-risk patients for extubation failure immediately after extubation. Before starting NPPV, N-CPAP and high flow oxygen were used in 51 (47.7 %) and 39 (36.4 %) patients, respectively.
The median time from admission to intensive care unit to NPPV implementation was 260 h (range 0–3,120), and the time from extubation to NPPV implementation (when applicable) was 12 h (range 0–450). Twenty-one patients required more than one NPPV course. A residual cardiac defect was present in 36 NPPV courses in 22 patients. Of these, 19 required surgical or catheterization intervention (Table 2).
NPPV Settings
Positive end-expiratory pressure (PEEP) was commenced at a median of 10 cm H2O (range 4–12), and the median of the maximum values was 10 cm H2O (range 4–14). Inspiratory positive airway pressure was started at a median of 20 cm H2O (range 10–27), and the median of the maximum values was 21 cm H2O (range 10–28).
Initial settings for respiratory rate were 25 breaths/min (range 10–36), and FiO 2 was 0.5 (range 0.25–1.0). Maximum settings for respiratory rate were 25 breaths/min (range 10–37) and FiO2 was 0.5 (range 0.3–1.0).
Interfaces
NPPV was applied by way of a nasopharyngeal tube, oronasal mask, or helmet in 87 (81.3 %), 17 (15.9 %), and 3 (2.8 %) patients, respectively.
Outcome
Within the first hour of NPPV, PaO2/FiO2 was significantly increased, and arterial pCO 2 (partial pressure of carbon dioxide) and respiratory rate were decreased compared with baseline values (before NPPV initiation) (Fig. 2). This decrease in respiratory rate and increase in PaO2/FiO2 continued during the first 24 h of therapy, and pCO2 was decreased during the first 6 h. No change in heart rate, systemic blood pressure, or pH was observed.
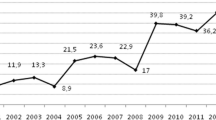
The median duration of NPPV for all patients was 37 h (range 2–372). In 64 (59.8 %) patients, NPPV was successfully used without the need for tracheal intubation; the duration of NPPV was 36 h (range 4–372). In 6 events, NPPV was successfully applied, but it was terminated because of planned corrective cardiac surgery (n = 3), withholding of life-supporting treatment (n = 2), and a switch to bubble N-CPAP with later surgical intervention (n = 1). In 43 (40.1 %) patients, intubation was required for 31 h (range 2–365) after NPPV implementation. In a subgroup of 73 postextubation failures, the success of NPPV was 56 % (Fig. 1).
Predictive Factors of NPPV Failure
Univariate analysis showed that the absence of improvement in PaO2/FiO2 at hours 6 and 12, pH <7.36 at hour 1, presence of infection and residual cardiac defect, and need for reintervention were predictive factors of NPPV failure (Table 3). RACHS and ABC scores were greater in failed NPPV courses. No relationship was found between outcome and age, sex, body weight, cyanotic vs. noncyanotic heart disease, and presence of Down syndrome. Logistic regression model analysis showed that ABC score, presence of infection and residual cardiac defect, and pH <7.36 in hour 1 were independent predictors of NPPV failure (r 2 = 0.37, Table 4).
Complications
Clinical tolerance of NPPV was good with one case of skin injury and no cases of abdominal distension or vomiting. The need for sedation during treatment was the same as that before NPPV initiation in 80 (74.8 %), increased in 16 (14.9 %), and decreased in 11 (10.3 %) patients. No patient had cardiorespiratory arrest with NPPV or before/during intubation. Nine patients died; all were intubated at the time of death. Causes of death were complications during extracorporeal membrane oxygenation (n = 1), sepsis (n = 1), bleeding from aortopulmonary collateral vessels (n = 1), and withholding of life-supporting treatment (n = 6).
Discussion
Although NPPV is increasingly used in the intensive care unit for children with various forms of respiratory failure, its efficacy, safety, and tolerability in pediatric cardiac patients has not been clearly established [1–3, 8, 26, 28]. Pediatric cardiac patients receiving NPPV represent a specific patient population because several mechanisms are involved in the process of respiratory failure [4, 25, 29]. These mechanisms include congestive heart failure, pulmonary hypertension, pulmonary disease, malnutrition, and chromosomal abnormalities. In patients after surgery acute lung injury due to extracorporeal bypass, diaphragm dysfunction and airway obstruction, may impair respiratory muscle mechanics. Acquired neuromuscular deficits related to critical illness or prolonged use of neuromuscular blockade, may also play a role [6, 17]. Although the etiology of respiratory failure is multifactorial, we identified the main cause of respiratory failure in each individual patient. The most commonly occurring causes of respiratory failure were cardiac failure, infection, and chronic lung disease, and less common causes were diaphragm paralysis and respiratory distress syndrome.
Decreased functional residual capacity, which is frequently present in patients with cardiac failure and after cardiac surgery, can be improved with continuous positive pressure. This improvement can be augmented by additional pressure support and/or pressure controlled breaths, which can help maintain good lung volume and decrease the load of the inspiratory muscles and the work of breathing [14].
NPPV can positively affect respiratory function as well as improve cardiac function [5, 12]. NPPV has been successfully used in adult cardiac postsurgical patients with hypoxemic acute respiratory failure [5, 12]. In patients with right-ventricular failure, positive pressure application may decrease right ventricular output [12]. However, taking into consideration a close ventricular interdependence in infants and children, a favorable effect on the left ventricle may overcome a negative effect of positive pressure ventilation on the right ventricle, particularly if adequate preload is provided.
Considering the complex interplay of numerous mechanisms involved in NPPV, we consider that pediatric cardiac patients may benefit from this respiratory support earlier in the progression of respiratory failure than other patients. Patients on NPPV should be closely monitored to detect hemodynamic deterioration, which would require tracheal intubation.
In our study, an improvement in breathing pattern and gas exchange was observed as early as 1 h after initiation of NPPV; PaO2/FiO2 was significantly greater; and arterial pCO2 and respiratory rate were lower compared with baseline values (Fig. 2). This decrease in respiratory rate and increase in PaO2/FiO2 remained during the first 24 h of NPPV. Similar findings have been observed in other studies [2, 9, 29]. In contrast, to studies in noncardiac pediatric patients with respiratory failure, NPPV did not improve heart rate in our patients [22, 28, 29]. We speculate that tachycardia in cardiac patients is related to cardiac failure and use of inotropes. No changes in systemic blood pressure and pH were observed during the study period.
The overall success rate of NPPV in our study was 59.8 %. The rate is within the range of the success rates reported for the use of NPPV in pediatric patients (57–97 %) [8, 20, 28] and lower than that reported in pediatric cardiac patients (64 % to 88 %) [2, 27, 29]. This discrepancy between studies may be due to the low age of our patients and greater complexity of cardiac diseases and surgical procedures compared with other studies. Several pediatric studies found that smaller children have a greater risk of failure [2, 15, 18]. However, age and weight did not predict a poor response to NPPV in our patient group. In pediatric studies, a greater incidence of noninvasive ventilation failure was reported in patients with severe conditions [3, 8, 18]. Our results are in concordance with these findings because the severity of cardiac condition, as assessed by the RACHS and ABC scores, was predictive for NPPV failure [2, 27, 29].
The presence of cyanotic versus noncyanotic cardiac disease did not affect our results. However, the presence of residual cardiac defects, as well as the need for surgical or catheterization intervention, were associated with failed NPPV. Furthermore, patients with a residual cardiac defect required multiple courses of NPPV. These findings are similar to the results of extubation after cardiac surgery in young children in whom poor heart function was the most common cause of failed extubation [13].
In the current study, the presence of infection was predictive of NPPV failure. In contrast, to the experience of failed noninvasive ventilation in patients with trisomy 21 [4], the presence of a syndrome in our patients was not linked to the results.
In our study, lack of improvement of PaO2/FiO2 in hours 6 and 12 and pH <7.36 in hour 1 were predictive for NPPV failure. In other studies, low PaO2/FiO2 [4, 18], high FiO2 [9], and low pH [7] after 1 h of noninvasive ventilation predicted failure.
In several pediatric studies [2, 19], most of the patients who did not have successful noninvasive ventilation were intubated within the first 24 h. In our study, the median time was 31 h when NPPV failure was determined to require invasive ventilation with intubation. Therefore, patients must be closely monitored even >24 h after initiation of NPPV, particularly those with risk factors for NPPV failure. The patients who were successfully weaned from NPPV had a median time of ventilation of 36 h.
In our study, 67.3 % of NPPV courses occurred after failure of extubation. The incidence of failed extubation after pediatric cardiac surgery is greater compared with that in the general pediatric population [6, 17]. These patients are particularly vulnerable to the increased metabolic demands imposed by spontaneous breathing, and cardiac output may be compromised by altered respiratory mechanics. Furthermore, these patients often have a combination of cardiovascular and respiratory failure.
The application of noninvasive ventilation as a new therapeutic method for postextubation respiratory failure has shown mixed results. A large multicenter trial [10] in adults showed a greater mortality rate in the noninvasive ventilation group, presumably due to delayed recognition of failure of noninvasive ventilation. Pediatric studies with postextubation respiratory failure showed a lower success rate than rates reported in other NPPV pediatric studies, which did not include postextubation cases [19, 28]. In contrast, in a study by Essouri et al. [8], respiratory failure after extubation formed the largest group. In addition, Pons et al. [24] studied postextubation respiratory failure after cardiac surgery in children and showed a similar success rate of noninvasive ventilation as studies with non-postextubation failures. In our subgroup of 73 cases with postextubation failure, success of NPPV was similar to overall success (56 vs. 59.8 %).
In many units, general guidelines for noninvasive ventilation settings start with PEEP at 4 to 5 cm H2O and further increase it as necessary up to a maximum of 10 cm H2O. Inspiratory positive airway pressure is started at 6–8 cm H2O and gradually increased. If the patient is not breathing sufficiently, a back-up rate is given [18, 19, 23]. In our patient group, ventilatory settings at NPPV initiation were greater than those reported in other studies [18–20, 23, 27]. PEEP was commenced at a median of 10 cm H2O, inspiratory positive airway pressure at 20 cm H2O, and respiratory rate at 25 breaths/min. This difference between studies can be explained by the complexity of respiratory failure and the young age of our patients. Inspiratory effort generated by the young children is often too small to be detected by the ventilator, thus resulting in the need for a back-up respiratory rate [11, 28]. Therefore, we set a high back-up rate to overcome the problems associated with an inadequate inspiratory trigger.
Noninvasive ventilation can be delivered by way of nasal, oronasal, and full-face masks and nasal pillows or cushions. The choice of the interface may be challenging in young children [11] because commercial masks remain limited, particularly for infants. One approach is to use a nasal mask as an oronasal mask. In our center, oropharyngeal tubes are mostly used in neonates and infants. However, meticulous “sealing” is important to overcome problems with air leaks.
NPPV was well tolerated in our study. In one patient, skin breakdown occurred. Because we used colloid dressings in places of compression, such a complication did not occur. No gastric distension was an issue.
Limitations of the Study
This study has the limitations of a noncontrolled study. However, we prospectively evaluated the results of NPPV in a large cohort of the pediatric cardiac patients according to the protocol.
Conclusions
NPPV improved oxygenation and decreased respiratory effort in pediatric cardiac patients, 59.8 % of whom eventually did not receive intubation. This method was safe and effective for use in young infants and in those after postextubation failure. High-complexity surgical score, presence of infection and residual cardiac defect, and pH <7.36 in the first hour are independent predictors of NPPV failure, which occurs in most patients >24 h after the onset of therapy.
References
Beers SL, Abramo TJ, Bracken A, Wiebe RA (2007) Bilevel positive airway pressure in the treatment of status asthmaticus in pediatrics. Am J Emerg Med 25:6–9
Bernet V, Hug MI, Frey B (2005) Predictive factors for the success of noninvasive mask ventilation in infants and children with acute respiratory failure. Pediatr Crit Care Med 6:660–664
Carrillo A, Gonzalez-Diaz G, Ferrer M, Martinez-Quintana ME, Lopez-Martinez A et al (2012) Noninvasive ventilation in community-acquired pneumonia and severe acute respiratory failure. Intensive Care Med 38:458–466
Chin K, Uemoto S, Takahashi K et al (2005) Noninvasive ventilation for pediatric patients including those under 1-year-old undergoing liver transplantation. Liver Transplant 11:188–195
Coimbra VR, Lara Rde A, Flores EG, Nozawa E, Auler JO Jr, Feltrim MI (2007) Application of noninvasive ventilation in acute respiratory failure after cardiovascular surgery. Arq Bras Cardiol 89:298–305
Cooper DS, Costello JM, Bronicki RA, Stock AC, Jacobs JP, Ravishankar C et al (2008) Current challenges in cardiac intensive care as follows: optimal strategies for mechanical ventilation and timing of extubation. Cardiol Young 1(Suppl 3):72–83
Dohna-Schwake C, Stehling F, Tschiedel E, Wallot M, Mellies U (2011) Noninvasive ventilation on a pediatric intensive care unit: feasibility, efficacy, and predictors of success. Pediatr Pulmonol 46:1114–1120
Essouri S, Chevret L, Durand P, Haas V, Fauroux B, Devictor D (2006) Noninvasive positive pressure ventilation: five years of experience in a pediatric intensive care unit. Pediatr Crit Care Med 7:329–334
Essouri S, Durand P, Chevret L, Haas V, Perot C, Clement A, Devictor D, Fauroux B (2008) Physiological effects of noninvasive positive ventilation during acute moderate hypercapnic respiratory insufficiency in children. Intensive Care Med 34:2248–2255
Esteban A, Frutos-Vivar F, Ferguson ND et al (2004) Noninvasive positive pressure ventilation for respiratory failure after extubation. N Engl J Med 350:2452–2560
Fauroux B, Leroux K, Desmarais G et al (2008) Performance of ventilators for noninvasive positive pressure ventilation in children. Eur Respir J 31:1300–1307
Guarracino F, Ambrosino N (2011) Noninvasive ventilation in cardio-surgical patients. Minerva Anestesiol 77:734–741
Harrison AM, Cox AC, Davis S, Piedmonte M, Drummond-Webb JJ, Mee RB (2002) Failed extubation after cardiac surgery in young children: prevalence, pathogenesis, and risk factors. Pediatr Crit Care Med 3:148–152
Imanaka H, Takeuchi M, Tachibana K, Takauchi Y, Nishimura M (2004) Changes in respiratory pattern during continuous positive airway pressure in infants after cardiac surgery. J Anesth 18:241–249
Joshi G, Tobias JD (2007) A five-year experience with the use of BiPAP in a pediatric intensive care unit population. J Intensive Care Med 22:38–43
Kovacikova L, Dobos D, Zahorec M (2009) Noninvasive positive pressure ventilation for bilateral diaphragm paralysis after pediatric cardiac surgery. Interact Cardiovasc Thorac Surg 8:171–172
Manrique AM, Feingold B, Di Filippo S, Orr RA, Kuch BA, Munoz R (2007) Extubation after cardiothoracic surgery in neonates, children, and young adults: one year of institutional experience. Pediatr Crit Care Med 8:552–555
Mayordomo-Colunga J, Medina A, Rey C, Díaz JJ, Concha A, Los Arcos M (2009) Predictive factors of non invasive ventilation failure in critically ill children: a prospective epidemiological study. Intensive Care Med 35:527–536
Mayordomo-Colunga J, Medina A, Rey C, Concha A, Menéndez S, Los Arcos M et al (2010) Non invasive ventilation after extubation in paediatric patients: a preliminary study. BMC Pediatr 5:10–29
Muñoz-Bonet JI, Flor-Macián EM, Brines J, Roselló-Millet PM, Cruz Llopis M, López-Prats JL, Castillo S (2010) Predictive factors for the outcome of noninvasive ventilation in pediatric acute respiratory failure. Pediatr Crit Care Med 1:675–680
Oktem S, Cakir E, Uyan ZS et al (2010) Diaphragmatic paralysis after pediatric heart surgery: usefulness of noninvasive ventilation. Int J Pediatr Otorhinolaryngol 74:430–431
Padman R, Lawless ST, Kettrick RG (1998) Noninvasive ventilation by way of bilevel positive airway pressure support in pediatric practice. Crit Care Med 26:169–173
Pons M, Cambra FJ (2003) Noninvasive ventilation. Ann Pediatr (Barc) 59:165–172
Pons MO, Marimbaldo IP, Matute SS, Argallo MB, Rico AP (2009) Aplicacion de ventilacion no invasiva en pacientes postoperados cardiacos. Estudio retrospectivo. Ann Pediatr 71:13–19. doi:10.1016/j.anpedi.2009.03.014
Rimensberger PC, Heulitt MJ, Meliones J, Pons M, Bronicki RA (2011) Mechanical ventilation in the pediatric cardiac intensive care unit. World J Pediatr Congenit Heart Surg 2:609–619
Ruza F (2010) Noninvasive ventilation in pediatric acute respiratory failure: a challenge in pediatric intensive care units. Pediatr Crit Care Med 11:750–751
Stucki P, Perez MH, Scalfaro P, de Halleux Q, Vermeulen F, Cotting J (2009) Feasibility of noninvasive pressure support ventilation in infants with respiratory failure after extubation: a pilot study. Intensive Care Med 35:1623–1627
Yañez LJ, Yunge M, Emilfork M et al (2008) A prospective, randomized, controlled trial of noninvasive ventilation in pediatric acute respiratory failure. Pediatr Crit Care Med 9:484–489
Zhang C-Y, Tan L-H, Shi S-S et al (2006) Noninvasive ventilation by way of bilevel positive airway pressure support in pediatric patients after cardiac surgery. World J Pediatr 4:297–302
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kovacikova, L., Skrak, P., Dobos, D. et al. Noninvasive Positive Pressure Ventilation in Critically Ill Children With Cardiac Disease. Pediatr Cardiol 35, 676–683 (2014). https://doi.org/10.1007/s00246-013-0837-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-013-0837-7