Abstract
This study aimed specifically to identify the predictors of prolonged recovery after the arterial switch operation for transposition of the great arteries in infants. The clinical records of all infants admitted to the surgical intensive care unit (SICU) between January 2000 and March 2011 after an arterial switch operation were retrospectively reviewed. The cohort was divided into a prolonged recovery group that included all patients who exceeded the 75th percentile for duration of SICU stay and a standard recovery group that included all the remaining patients. Of the 102 patients in the final analysis, 31 experienced prolonged recovery. The median SICU stay was 18 days (range, 14–58 days) for the patients in the prolonged recovery group and only 8 days (range, 5–13 days) for the patients in the standard recovery group. After univariate analysis, a stepwise logistic regression model analysis was used to compare the demographic data as well as the pre-, intra-, and postoperative variables between the two groups. Of all the variables analyzed, high postbypass serum lactate level [odds ratio (OR), 2.610; 95 % confidence interval (CI), 1.464–4.653; p = 0.039], need for larger volume of resuscitation fluid (OR, 3.154; 95 % CI, 1.751–5.682; p = 0.018), and noninfectious pulmonary complication (OR, 2.844; 95 % CI, 1.508–5.363; p = 0.025) were identified as independent risk factors for prolonged recovery among infants undergoing an arterial switch operation for transposition of the great arteries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advances in surgical techniques and postoperative management have made it possible for children to benefit from surgical intervention to correct or palliate congenital heart disease [6, 11], even complex abnormal cardiac lesions [1, 6, 10] such as the transposition of the great arteries (TGA) [7, 15]. During the neonatal period, TGA is the most common cyanotic congenital heart disease, and without surgical intervention, survival is not expected.
Because of the current low operative mortality and excellent survival, the arterial switch operation (ASO) is now the standard, effective, and preferred surgical procedure for TGA [4, 13, 21]. Continued innovations for this operation strategy have occurred. Furthermore, the boundaries and juncture of the primary ASO in patients with TGA have been extending in past several decades [13, 23]. Therefore, a growing number of neonates and infants with TGA have undergone ASO for correction of the arterial malformation and have required postoperative intensive care [4].
Critical care in the surgical intensive care unit (SICU) is an important stage for successful implementation of the aforementioned operation. A previous study suggested that prolonged postoperative ICU time is independently associated with impaired cognitive function for children 8 years old [18]. Thus, prolonged recovery in the SICU after ASO has become a critically important issue in the reduction of postoperative morbidity and mortality. The defining factors associated with prolonged recovery may therefore be essential for improvement of immediate and long-term outcomes.
The current study aimed to identify perioperative factors that contribute to a prolonged recovery course after ASO for infants admitted to the SICU.
Materials and Methods
After approval by the local ethics committee, the study was conducted in an 18-bed SICU over an 11 year period (from January 2000 to March 2011) at a university children’s hospital located in Eastern China. Due to the retrospective nature of our study, the need for informed consent was waived.
The study enrolled 111 consecutive patients with TGA undergoing the switch operation. Of the 111 patients, 53 with TGA and intact ventricular septum (TGA/IVS) were routinely administered prostaglandin E1 (PE1, 5–10 ng/kg/min) to reopen the ductus arteriosus or to maintain its patency or mechanical ventilation if necessary after PE1 administration. They received ASO or rapid two-stage ASO as soon as possible. Preoperative balloon atrial septostomy was not used in our center. Therefore, nine patients with TGA/IVS had to receive emergency ASO because of severe hypoxia or cardiac dysfunction.
Nine patients were excluded from the study due to incomplete clinical data (3 patients), prematurity (1 patient), death after surgery (3 patients), or need for extracorporeal membrane oxygenation support in the immediate postoperative period (2 patients). All the patients admitted to the SICU received critical care immediately after surgery. None of these patients returned to bypass or had revision of the operation or coronary translocation.
Study Design and Data Definitions
The study population included all the patients who survived to SICU discharge. The patients’ demographic data together with their anatomic and perioperative clinical physiologic variables were collected retrospectively from medical records. The demographic and preoperative variables included age, weight, preoperative cardiac dysfunction, noncardiac anomaly, pulmonary artery hypertension, and pneumonias requiring mechanical ventilation (MV) support and saturation of oxygen. The preoperative serum urea nitrogen, creatinine, and blood glucose levels were analyzed after admission.
The intraoperative variables included emergency operation, American Society of Anesthesiology (ASA) classification, coronary artery anatomy patterns, cardiopulmonary bypass (CPB) time, operation time, need for defibrillation to resuscitate heart after circulatory arrest, ultrafiltrated volume, negative fluid balance during the operation, and postbypass serum lactate level. The postbypass serum lactate level was analyzed at the end of the surgery. In part, the postoperative variables were nosocomial pneumonia, noninfectious pulmonary complication, postoperative arrhythmia, postoperative pulmonary artery hypertension, and postponed sternal closure.
The patients with TGA/IVS were divided into an early switch group (n = 31; age, <3 weeks) and a late switch group (n = 19; age, ≥3 weeks) according to the previous method [13]. The definitions for the variables are presented in Table 1.
Postoperative day 1 (POD 1) was defined as the period between transfer from the operating room to the SICU and 7 a.m. on the morning after surgery. The SICU central venous pressure (CVP) was measured at admission by internal jugular catheter pressure tracing, whereas the left atrial pressure (LAP) was measured by an intracardiac atrial line pressure tracing. Arterial blood gas and hematocrit (Hct) were analyzed using the worst values on POD 1. The postoperative levels of serum alanine transaminase (ALT), serum aspartate aminotransferase (AST), blood glucose, total bilirubin, serum urea nitrogen, and creatinine were analyzed using the peak values on POD 1.
The POD 1 inotropic score was calculated by a previously described formula as follows: dopamine + dobutamine + (milrinone × 10) + (epinephrine × 100) using peak infusions rates measured in μg/kg/min [3, 5]. The volume of resuscitation fluid was calculated with the following formula: total intake resuscitation fluid on POD 1/weight of the patient on the day of the operation (ml/ kg).
Resuscitation fluid was retrospectively identified as any volume of the intake fluids (colloid, crystalloid, or blood products) and the medication infusion volumes. In the practice, volume was given at the discretion of the attending cardiac intensivist to maintain adequate circulatory parameters, namely, LAP 5–9 mmHg and aortic blood pressure 60–80 mmHg. All fluid was infused at a constant speed to avoid blood pressure rapid fluctuation. If LAP exceeded 9 mmHg, fluid infusion was <3 ml/kg, with appropriate diuretics after exclusion of cardiac dysfunction. If LAP was <5 mmHg, 5–10 ml/kg of fluid was infused within 20–30 min to complement volume. Two fluid exposure cohorts, high- and low-volume resuscitation fluid groups, were further created based on the 75th percentile for the volume of resuscitation administered. The MV period was from the time of arrival at the SICU to the time of successful extubation. The criteria for extubation were protocolized as in our previous study [24].
All the patients were transferred to wards when they met the criteria for discharge from the SICU, specifically, comfortable breathing with supplemental oxygen via a nasal cannula at 1 l/min or less; fractional inhaled oxygen at 0.3 or less; stable and normal hemodynamics, heart rate, and blood pressure; adequate tissue perfusion [27]; and consultation by a cardiac intensivist and a cardiovascular surgeon.
Because no consensus existed on the exact definition of prolonged recovery, the special patients in this study were classified into two groups according to the duration of their SICU stay: the prolonged recovery group and the standard recovery group. The prolonged recovery group included all the patients exceeding the 75th percentile for duration of SICU stay, and the standard recovery group included all the remaining patients.
Statistical Analysis
Descriptive data for continuous variables are presented as mean ± standard deviation or as median and range when appropriate, and descriptive statistics for categorical variables are presented as percentage or counts. First, univariate analysis was performed to compare demographic data, and pre-, intra-, and postoperative variables of the prolonged recovery patients with those of the standard recovery patients. Comparisons between the two groups were performed via the unpaired Student’s t test or the Mann–Whitney U test for continuous variables and the chi-square test for categorical variables. Then, logistic regression analysis was used to identify independent risk factors for prolonged recovery. The variables with a p value lower than 0.1 were enrolled in this regression model. A p value lower than 0.05 was considered statistically significant. Statistical analysis was performed via the Statistical Package for the Social Sciences (SPSS) version 16.0 (SPSS, Chicago, IL, USA) for Windows.
Results
Outcomes
During the study period, 102 infants with TGA who required a switch operation were enrolled in the study. The patients’ demographic characteristics are presented in Table 2, and the cardiac lesion types are shown in Table 3. The median age at the time of the switch operation was 25 days (range, 1–360 days), and the median weight was 3.8 kg (range, 2.5–10 kg). The overall median SICU stay for all the patients was 10 days (range, 5–58 days).
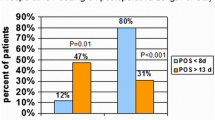
Of the 102 patients, 31 were identified as a prolonged recovery group. The median SICU stay was 18 days (range, 13–58 days) for the patients in the prolonged recovery group and only 8 days (range, 5–13 days) for the patients in the standard recovery group. The hospital stay for the patients in the prolonged recovery group was significantly longer than for the patients in the standard recovery group (p < 0.001). The median hospital stays for the two groups were respectively 24 days (range, 21–62 days) and 20 days (range, 13–54 days). In addition, the hospital length of stay did not differ significantly between the patients with TGA/IVS in the early switch group (11 days; range, 7–24 days) and those in the late switch group (14 days; range, 9–28 days) (p = 0.053).
Univariate Analysis
Demographic data and pre-, intra-, and postoperative variables were evaluated univariately as possible risk factors of prolonged recovery separately. In the analysis of demographic and preoperative variables, only low weight was associated with prolonged recovery (Table 3; p < 0.05). The intraoperative differences between the two groups are shown in Table 4. The significant intraoperative characteristics of the prolonged recovery group included long CPB time, variant coronary patterns, and level of postbypass serum lactate (all p < 0.05).
The postoperative characteristics associated with prolonged recovery are shown in Tables 5 and 6. They included inotropic score, time of MV, and Hct on POD 1 (all p < 0.05). In addition, the patients in the prolonged recovery group were more likely to have nosocomial pneumonias, noninfectious pulmonary complications, and the need for a large volume of resuscitation during the SICU stay (all p < 0.05).
Multivariate Analysis
Table 7 shows the overall analysis of the perioperative variables for the study population with prolonged recovery via logistic regression analysis. This multivariable regression model identified that the independent risk factors for prolonged SICU recovery were high postbypass serum lactate level (p = 0.039), need for a larger volume of resuscitation fluid (p = 0.018), and noninfectious pulmonary complication (p = 0.025) during the SICU stay. The most powerful predictor of prolonged recovery was the need for a larger volume of resuscitation fluid [odds ratio (OR), 3.154]. Noninfectious pulmonary complication was a modest predictor for prolonged recovery (OR, 2.844). In addition, postbypass lactate level also was found to be a significant predictor for prolonged recovery in the SICU (OR, 2.610). The cut-off value of postbypass lactate level for predicting prolonged recovery was 5.3 mmol/l. The patients with these variables had a higher probability of prolonged recovery in the SICU after the switch operation for TGA than the patients without these risk factors.
Discussion
In this retrospective study of infant patients undergoing a switch operation for TGA, we explored risk factors for prolonged recovery in the SICU. High postbypass serum lactate level, need for a larger volume of resuscitation fluid on POD 1, and noninfectious pulmonary complication were found to be independent risk factors associated with delayed recovery. In addition, the delayed recovery after ASO significantly increased the hospital length of stay in this study population.
In the final results, none of the preoperative variables was shown to be an independent risk factor for prolonged recovery. As expected and consistent with our results, Wheeler et al. [27] recently reported that only prematurity was independently associated with a prolonged ICU stay after ASO. Unfortunately, the premature neonate was excluded from the current study. Significant improvements in fetal diagnosis, intervention, and scientific preoperative management make it possible to reverse the insult of a detrimental stimulation (e.g., abnormal hemodynamics, acidosis, tissue hypoperfusion) on the structure or function of the heart and other organs before the operation [5, 6]. Moreover, the boundaries of primary ASO for patients with TGA have been extended [13]. Therefore, the benefit of choosing the best time to correct cardiac anisotrophy outweighed the negative effect of a poor status before the operation.
Notably, among the intraoperative variables, only high postbypass serum lactate level was significantly and independently associated with an increased probability of a prolonged recovery. The following reasons may to some extent helped to exclude other intraoperative variables as independent factors for prolonged recovery after ASO. First, the same cardiac surgical team performed the ASO at our center, so the strategy and procedure of surgery were similar in the two groups. Second, all the patients in both groups used the modified ultrafiltration strategy, which has been shown to facilitate patients’ recovery after ASO [14]. In addition, previous findings show that patients with common coronary variants have undergone ASO without additional worse complications than those with a usual coronary pattern [19, 22] and that patients with complex coronary arterial anatomy have a slightly longer hospital course [16]. There were a few complex coronary arterial anatomies, and optimized surgical techniques were used to relocate these challenging variations in our study. Therefore, coronary variant was not a factor for prolonged recovery in the multivariable analysis.
As expected, a set of postoperative events, including the need for a larger volume of resuscitation fluid and noninfectious pulmonary complications, was found to be associated with prolonged recovery. In the current study, a larger volume of resuscitation fluid was the strongest predictor for prolonged recovery of patients after ASO, but we cannot provide exact rationales to interpret this result.
Interestingly, Wernovsky et al. [26] reported that fluid overload contributed to morbidity after arterial switch surgery. The systemic inflammatory response to open heart surgery and CPB may contribute to endothelial injury and capillary leakage, leading to fluid leakage from the microcirculation. Therefore, in the earlier stage after ASO, volume expansion with colloid or crystalloid is necessary to maintain adequate preload and cardiac output. However, recent data suggest that the use of colloid for volume expansion has no survival advantage and possibly poses some detriment [8, 17].
Maintaining fluid balance, even a negative fluid balance for “permissive hypovolemia,” has been accepted as one of the important strategies for reducing the amount of pulmonary edema, preventing intravascular volume overload, and reducing multiple-organ dysfunction early after pediatric cardiac surgery [25]. In the clinical setting, transient myocardial dysfunction early after cardiac surgery is common, and it is necessary to use inotropic drugs to maintain mean arterial blood pressure above the age-appropriate lower limit. In addition, elevation of ventricular end-diastolic pressure from impaired myocardial function may further elevate postoperative periphery blood pressure and potentially lead to leakage of fluid from the microcirculation. The loss of fluid results in pleural effusion or ascites and even multiple membrane cavity effusion or anasarca. These all were a direct cause of a prolonged SICU stay.
Although speculative, the need for large-volume resuscitation in the early postoperative period after the ASO may represent the compounding effects of multiple risk factors that mediate a prolonged recovery in the SICU.
Noninfectious pulmonary complications occur commonly after pediatric open (32 %) and closed (20 %) heart surgery [12] and are reported to be associated with a prolonged ICU stay after cardiac surgery [2, 12]. Similarly, they were observed in 38.2 % of patients after ASO in the current study. Polito et al. [20] indicated that complex congenital heart surgery may promote the occurrence of such complications. The special patients in our study may have been responsible for the high ratio. The prolonged recovery group had a significantly higher incidence of noninfectious pulmonary complications than the standard recovery group, suggesting that the patients with these complications were more likely to have a prolonged SICU stay after ASO. The information regarding their contribution to the prolonged recovery was sparse. A previous study suggested that noninfectious pulmonary complications have strong influence on the overall ventilator duration for children after cardiac surgery [9]. Notably, the prolonged recovery patients had a long time of MV support in the current study. It can be speculated that this was a result of the pulmonary complications.
The limitations of the current study should also be acknowledged. First, this study was based on a single center, local practice patterns, and a small number of cases, which may limit the application of the current results to other institutions. Second, this was a retrospective study, which may have introduced potential classification bias and thus was subject to physician practice variations with regard to administration of fluid, use of inotropic agents, and parameters for extubation and discharge from the SICU. It is likely, however, that this variability was present randomly across the cohort, thus having minimal impact on the final analysis.
In conclusion, the current study found that the high postbypass serum lactate level, the need for a larger volume of resuscitation fluid on POD 1, and the noninfectious pulmonary complications were identified as independent risk factors for prolonged recovery after ASO in the SICU. A prospective multicenter study with a larger number of patients is necessary for further investigation of this important clinical problem.
References
Al Qethamy HO, El Oakley RM, Tageldin MM, Abdulhamed JM, Al Faraidi Y (2008) Late complex biventricular repair after bidirectional cavopulmonary shunt. J Card Surg 23:719–721
Bandla HP, Hopkins RL, Beckerman RC, Gozal D (1999) Pulmonary risk factors compromising postoperative recovery after surgical repair for congenital heart disease. Chest 116:740–747
Bradley SM, Simsic JM, McQuinn TC, Habib DM, Shirali GS, Atz AM (2004) Hemodynamic status after the Norwood procedure: a comparison of right ventricle-to-pulmonary artery connection versus modified Blalock-Taussig shunt. Ann Thorac Surg 78:933–941
DeBord S, Cherry C, Hickey C (2007) The arterial switch procedure for transposition of the great arteries. AORN J 86:211–226; quiz 227–230
Dibardino DJ, Allison AE, Vaughn WK, McKenzie ED, Fraser CD Jr (2004) Current expectations for newborns undergoing the arterial switch operation. Ann Surg 239:588–596 discussion 596–598
El-Zein C, Ilbawi MN (2008) Recent advances in neonatal cardiac surgery. World J Surg 32:340–345
Emani SM, Beroukhim R, Zurakowski D, Pigula FA, Mayer JE, del Nido PJ et al (2009) Outcomes after anatomic repair for d-transposition of the great arteries with left ventricular outflow tract obstruction. Circulation 120:S53–S58
Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R; SAFE Study Investigators (2004) A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 350:2247–2256
Fischer JE, Allen P, Fanconi S (2000) Delay of extubation in neonates and children after cardiac surgery: impact of ventilator-associated pneumonia. Intensive Care Med 26:942–949
Fudge JC Jr, Li S, Jaggers J, O’Brien SM, Peterson ED, Jacobs JP et al (2010) Congenital heart surgery outcomes in Down syndrome: analysis of a national clinical database. Pediatrics 126:315–322
Hartyánszky I, Lozsádi K, Király L, Prodán Z, Mihályi S, Bodor G et al (2005) Surgical management of preterm infants and low birth weight neonates with congenital heart disease. Orv Hetil 146:69–73
Ip P, Chiu CS, Cheung YF (2002) Risk factors prolonging ventilation in young children after cardiac surgery: impact of noninfectious pulmonary complications. Pediatr Crit Care Med 3:269–274
Kang N, de Leval MR, Elliott M, Tsang V, Kocyildirim E, Sehic I, et al (2004) Extending the boundaries of the primary arterial switch operation in patients with transposition of the great arteries and intact ventricular septum. Circulation 110:II123–II127
Kotani Y, Honjo O, Osaki S, Kawabata T, Ugaki S, Fujii Y et al (2008) Effect of modified ultrafiltration on postoperative course in neonates with complete transposition of the great arteries undergoing arterial switch operation. Circ J 72:1476–1480
Liu YL, Hu SS, Shen XD, Li SJ, Wang X, Yan J et al (2010) Midterm results of arterial switch operation in older patients with severe pulmonary hypertension. Ann Thorac Surg 90:848–855
McMahon CJ, el Said HG, Feltes TF, Watrin CH, Hess BA, Fraser CD Jr (2002) Preoperative identification of coronary arterial anatomy in complete transposition, and outcome after the arterial switch operation. Cardiol Young 12:240–247
Myburgh J, Cooper DJ, Finfer S, Bellomo R, Norton R, Bishop N et al (2007) Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med 357:874–884
Newburger JW, Wypij D, Bellinger DC, du Plessis AJ, Kuban KC, Rappaport LA et al (2003) Length of stay after infant heart surgery is related to cognitive outcome at age 8 years. J Pediatr 143:67–73
Pasquali SK, Hasselblad V, Li JS, Kong DF, Sanders SP (2002) Coronary artery pattern and outcome of arterial switch operation for transposition of the great arteries: a meta-analysis. Circulation 106:2575–2580
Polito A, Patorno E, Costello JM, Salvin JW, Emani SM, Rajagopal S et al (2011) Perioperative risk factors for prolonged mechanical ventilation after complex congenital heart surgery. Pediatr Crit Care Med 12:e122–e126
Prêtre R, Tamisier D, Bonhoeffer P, Mauriat P, Pouard P, Sidi D et al (2001) Results of the arterial switch operation in neonates with transposed great arteries. Lancet 357:1826–1830
Qamar ZA, Goldberg CS, Devaney EJ, Bove EL, Ohye RG (2007) Current risk factors and outcomes for the arterial switch operation. Ann Thorac Surg 84:871–879
Raja SG, Shauq A, Kaarne M (2005) Outcomes after arterial switch operation for simple transposition. Asian Cardiovasc Thorac Ann 13:190–198
Shi S, Zhao Z, Liu X, Shu Q, Tan L, Lin R et al (2008) Perioperative risk factors for prolonged mechanical ventilation following cardiac surgery in neonates and young infants. Chest 134:768–774
Venkataraman ST, Khan N, Brown A (2000) Validation of predictors of extubation success and failure in mechanically ventilated infants and children. Crit Care Med 28:2991–2996
Wernovsky G, Wypij D, Jonas RA, Mayer JE Jr, Hanley FL, Hickey PR et al (1995) Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants: a comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92:2226–2235
Wheeler DS, Dent CL, Manning PB, Nelson DP (2008) Factors prolonging length of stay in the cardiac intensive care unit following the arterial switch operation. Cardiol Young 18:41–50
Acknowledgments
This work was financially support by the Zhejiang Provincial Program for the Cultivation of High-Level Innovative Health Talents (QS) and the National Science and Technology Plan Projects (2012BAI04B05).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Liu, X., Shi, S., Shi, Z. et al. Factors Associated With Prolonged Recovery After the Arterial Switch Operation for Transposition of the Great Arteries in Infants. Pediatr Cardiol 33, 1383–1390 (2012). https://doi.org/10.1007/s00246-012-0353-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-012-0353-1