Abstract
Congenital coronary artery anomalies are a well-recognized risk factor for sudden cardiac death in children as well as young adults, mostly during or immediately after intense exertion on the athletic field. Because these malformations are amenable to surgical treatment, timely identification is crucial. Unfortunately, antemortem diagnosis is notoriously difficult, partly due to the absence of abnormal test results in routine investigations. We present a 15-year-old boy who collapsed during exercise due to ventricular fibrillation. Coronary abnormalities were initially not identified, but they were clearly visualized by means of an echocardiogram and confirmed by multislice computed tomography. We would like to emphasize that echocardiography is capable of accurately identifying congenital coronary anomalies when attention is paid to the correct diagnostic hallmarks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An 11-year-old boy was screened for congenital coronary artery anomalies after the sudden death of his older brother, who was 2 years older and had a left coronary artery (LCA) anomaly, with an origin from the wrong sinus and an interarterial course. Electrocardiography (EKG), echocardiography, magnetic resonance coronary angiography (MRA), and exercise tolerance testing were interpreted as normal. Four years later however, at the age of 15, he collapsed during exercise (soccer) due to ventricular fibrillation. Immediate defibrillation and resuscitation were successful. His EKG on admission showed no abnormalities. Immediately postresuscitation, left ventricular shortening fraction was reduced (17%) but returned to normal (38%) within 48 h after admission. Troponine levels peaked at 2.24 μg/L (ref. < 0.2 μg/L).
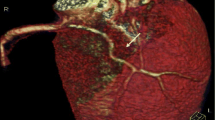
Echocardiography showed a typical cross-section of the right coronary artery (RCA) on the parasternal long-axis view, an important hallmark of an interarterial course of an anomalous coronary artery (Fig. 1a). Doppler flow imaging showed a stenotic origin of the right coronary artery from the left sinus of Valsalva and an interarterial, partially intramural, course between the aorta and pulmonary trunk (Fig. 2). Additionally, a small fistula from the right coronary artery to the superior caval vene was suspected. Multislice computed tomography (MSCT) and coronary angiography confirmed the echocardiographic findings (Fig. 3). The anomalies were successfully surgically corrected by unroofing the intramural portion of the right coronary artery.
Because coronary artery anomalies such as described here are associated with sudden cardiac death and are amenable to surgical treatment, timely identification is crucial. Unfortunately, antemortem diagnosis is notoriously difficult. About 50% of cases are discovered at autopsy [1]. Patients are often asymptomatic and routine investigations are within normal limits. Left ventricular wall motion as well as EKG testing, even during maximal exercise, show no abnormalities in most subjects. This further hampers diagnosing coronary artery disease, as illustrated by our patient. MRA and MSCT have proven to be useful diagnostic modalities. MSCT is preferable, as it is known to be the most accurate technique [3]. Coronary angiography is associated with possible complications related to its invasive nature.
Importantly, we would like to emphasize that echocardiography is capable of accurately identifying congenital coronary anomalies as well, when attention is paid to the correct diagnostic hallmarks [4]. To determine the origin of a coronary artery from the sinus of Valsalva, it is mandatory to carefully visualize color Doppler flow entering the coronary artery from the aorta (Fig. 2).
An interarterial course of a coronary artery between the aorta and pulmonary trunk is best visualized in both the parasternal long-axis view as well as the parasternal short-axis view as shown in Figs. 1a and b.
In our patient, the coronary abnormalities were initially not identified but were clearly visible on a new echocardiogram and confirmed by MSCT, both performed after resuscitation. Familial cases of congenital coronary artery anomalies do occur; they are, however, extremely rare [2].
References
Basso C, Maron BJ, Corrado D, Thiene G (2000) Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. J Am Coll Cardiol 35(6):1493–1501
Devanagondi R, Brenner J, Vricella L, Ravekes W (2008) A tale of two brothers: anomalous coronary arteries in two siblings. Pediatr Cardiol 29(4):816–819
Montaudon M, Latrabe V, Iriart X, Caix P, Laurent F (2007) Congenital coronary arteries anomalies: review of the literature and multidetector computed tomography (MDCT)-appearance. Surg Radiol Anat 29(5):343–355
Pelliccia A, Spataro A, Maron BJ (1993) Prospective echocardiographic screening for coronary artery anomalies in 1,360 elite competitive athletes. Am J Cardiol 72(12):978–979
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Marcus, K.A., Lemson, J., Backx, A. et al. Anomalous Coronary Artery from the Wrong Sinus in a 15-Year-Old Boy. Pediatr Cardiol 30, 205–207 (2009). https://doi.org/10.1007/s00246-008-9334-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-008-9334-9