Abstract
Extracorporeal shock wave lithotripsy (ESWL) is a safe and efficient treatment option for urinary stone disease. The overall stone-free rate (SFR) varies significantly. This study aimed to assess the influence of stone size, location, stone density, and skin-to-stone distance (SSD), on the outcome of ESWL. We assessed whether pre-treatment non-contrast-enhanced CT scan (NCCT) confers significant advantages compared to kidney-ureter-bladder film (KUB) only. We reviewed the medical records of 307 cases (165 men, 142 women) with renal and ureteral stones treated consecutively at our institution with ESWL between 2020 and 2023. 44 of these underwent a NCCT. The outcome of ESWL was defined in two ways: visible stone fragmentation on KUB, and the need for further treatment. Overall success of fragmentation was 85% (261 patients). 61% of patients (n = 184) didn’t need any further treatment. Stone size and location correlated significantly with treatment outcomes regarding the need for further treatment (p = 0.004) and stone fragmentation (p = 0.016), respectively. Unlike mean SSD (p = 0.462), the mean attenuation value (MAV) significantly correlated with the need for retreatment (p = 0.016). MAV seems to be a better predictor of treatment success (AUC of the ROC curve: 0.729), compared to stone size (AUC: 0.613). The difference between groups (with and without NCCT) in both treatment outcomes did not reach statistical significance. During decision-making, information regarding SSD and MAV can be useful in more dubious scenarios. However, it appears that their inclusion doesn’t provide substantial advantages when compared to relying solely on KUB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extracorporeal shock wave lithotripsy (ESWL) stands as a non-invasive, safe, and effective treatment choice for renal and ureteral stones. The success of ESWL depends on the procedure itself (namely the efficacy of the lithotripter and performance of ESWL), patients’ habitus, and stone characteristics (size, location, and composition). ESWL can reach Stone Free Rates (SFRs) of around 80% [1]. A recent meta-analysis reported ESWL as being less effective than percutaneous nephrolithotomy (PNL) and retrograde intrarenal surgery (RIRS) [2]; for urinary stones < 1 cm, there is no discernible difference in SFRs between ESWL and flexible ureteroscopy [1]. The higher rate of secondary procedures is the main obstacle for ESWL, compared to RIRS or PNL [3]. If patients are not selected adequately, SFRs can decrease, making retreatment potentially necessary. This consequently increases medical costs and unnecessary exposure to shock waves and radiation. What may fail in the selection of patients for ESWL is an incomplete stone evaluation. When patients are proposed for ESWL directly through their emergency room visit in our institution, most of them are evaluated through ultrasound and kidneys, ureters, and bladder film (KUB). This usually allows the patient to be quickly referred for an ESWL treatment. Stone disease is therefore not completely characterized regarding stone composition and inner structure, and also the patient’s habitus regarding skin-to-stone distance and surrounding anatomy. Still, it is possible through KUB to measure the largest stone size and to identify stone location, which are characteristics that also have a predictive value of treatment failure.
In the past decade, most studies have focused on assessing the impact of characteristics evaluated through non-contrast-enhanced CT scans (NCCT) on stone fragmentation. To date, eight studies have concurrently assessed renal and ureteral stone disease using NCCT [4,5,6,7,8,9,10,11]. Factors such as stone size, stone density, and skin-to-stone distance (SSD) are recognized as significant correlates of treatment success. However, there remains a lack of standardization in defining treatment outcomes across most studies. While some define treatment success as achieving a stone-free status [8, 11,12,13,14,15] others define it as visible stone fragmentation on KUB [16], with follow-up periods ranging from two weeks to three months. Moreover, there is variability in the definition of a complete ESWL treatment, with some authors considering up to three ESWL treatments as treatment success, while others define success with just one treatment. Table 1 presents a review of the literature.
We aim to investigate the possible predicting factors of ESWL success obtained with two different imaging modalities (KUB or NCCT). We correlate these variables with different treatment outcomes, namely stone fragmentation on KUB after treatment, and the need for retreatment after one session of ESWL.
Methods
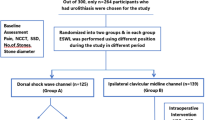
We evaluated in this retrospective study 307 consecutive ESWL treatments of renal and ureteral stone disease, between January 2020 and April 2023. We included patients with ureteral and kidney stones and excluded the ones who had more than one stone to treat. Data analysis was made after authorization from the Ethics Committee of Unidade Local de Saúde de Santo António (130-DEFI/122-CE). Stone size was measured by obtaining the maximum length of the stone on KUB. NCCT images were analyzed in a standard bone window (window width-1.120 and window level-300) [16]. We obtained the mean attenuation value (MAV), which defines stone density, by measuring the mean HU of the region of the stone excluding adjacent soft tissue. SSD was measured as defined by Nahas et al. [19], including the value of SSD at 0º, 45º and 90º. The mean SSD was calculated as the average value of those three measurements.
All lithotripsy treatments were performed using Siemens’ MODULARIS Variostar®. In the course of ESWL, patients received analgesia with paracetamol and remifentanil, and were subjected to a maximum of 3,000 shocks, with a frequency of 60 shocks/minute for obese patients and 90 shocks/minute for the remaining patients. The intensity varied according to the location of the stone. The power was incrementally increased during the procedure to allow renal vasoconstriction and patient comfort. In patients with various comorbidities, a lower intensity level was used, along with control of arterial pressure along the treatment. Stones were targeted through bi-planar fluoroscopy at regular intervals. Patients were discharged on the same day after the procedure.
Patients were followed up on an outpatient basis, with a KUB and urology consultation within one month after treatment. In this consult, determination of SFRs, and review of symptoms and complications were made by the attending physician. If necessary, a new treatment was proposed, namely a new session of ESWL, RIRS, or PNL.
We extracted from patients’ records characteristics to be correlated with treatment outcome, namely age, sex, weight, body mass index (BMI), presence or not of a JJ stent, stone size, and location. In patients with NCCT, MAV and SSD at 0º, 45º, and 90º were also included. We defined two variables as treatment outcomes: stone disintegration on KUB at one-month follow-up and need for retreatment.
Univariate (chi-square, t-test, and Mann-Whitney test when appropriate) and multivariate (binary logistic regression) analyses were performed to define factors significantly correlated with treatment outcomes. All tests were two-sided and we defined the p-value as < 0.05 to reject the null hypothesis. Multivariate analysis was performed including variables with marginal association with treatment outcome (p < 0.20). Receiver operating characteristic (ROC) curves were generated for factors considered to significantly predict ESWL outcome based on multivariate analysis. Statistical analyses were performed using IBM SPSS Statistics Version 29.0.1.0 (IBM Corp., New York, U.S.A.).
Results
A total of 307 ESWL treatments were included (165 men, 142 women), being 254 patients in total. Median age was 52 years (range 19–83 years) and BMI was 26.1 kg/m² (range 16.7–28.8 kg/m²). Median stone size was 9 mm (range 3–24 mm). From the analyzed cases, 44 patients underwent a NCCT because they presented with obstructive pyelonephritis in the emergency department (n = 23), had previous follow-up with NCCT in urology consultation (n = 9), had previous evaluation from an external or family physician (n = 10), or there were doubts in the evaluation of X-Ray images (because of bone calcifications) (n = 2). In this cohort, the median SSD was 114 mm (range 68–173 mm) and MAV 748 HU (median 270–1185 HU). 56 (18%) of the cases were caliceal stones, 102 (33%) were in the renal pelvis, and 149 (49%) were ureteral. Because only a small number of patients were able to provide the calculus for analysis (n = 35), we opted not to include information on stone composition. Regarding SFRs, 126 (41%) cases had no residual fragments (RFs). Nine and 14 cases had RFs of < 2 mm (3%) and between 2 and 4 mm (6%), respectively. 158 cases had RFs of > 4 mm (51%). The rate of complications was 21,5%, as described in Table 2.
In terms of treatment outcome, stone fragmentation was observed in 261 treatments (85%). Among this subset, 77 (30%) still required additional interventions, ESWL in 60 cases (77%), RIRS in 14 cases (18%), and PNL in three cases (4%). The retreatment rate was 37% (n = 115), with 73 undergoing another session of ESWL (23%). Moreover, 13% of cases needed a different treatment modality besides ESWL, with 39 undergoing RIRS (12%) and three undergoing PNL (1%). To summarize, out of the 254 patients enrolled in this study, 212 (83.5%) successfully managed their urinary stone disease solely with ESWL.
Regarding stone fragmentation, only stone location showed a significant correlation to stone fragmentation (p = 0.016). In the NCCT cohort, stone density (MAV) tended to be higher in cases with unsuccessful stone fragmentation, without reaching statistical significance (p = 0.064). There was no correlation between having done a CT scan before treatment and this treatment outcome (p = 0.531). Stone size correlated significantly with the need for retreatment (p = 0.004). In the NCCT cohort, unlike mean SSD (p = 0.462), MAV showed a significant correlation with no need for retreatment (p = 0.016). There was no correlation between having done a CT scan and this treatment outcome (p = 0.236). The results of the univariate analysis are summarized in Table 3.
Discussion
This is the first study to correlate stone characteristics with two different treatment outcomes. The absence of standardized criteria defining a successful ESWL treatment might account for the varying data observed in prior studies. Our findings notably diverge when comparing the two treatment outcome categories. The only significant variable in our study that could predict stone disintegration was stone location. Nakasato et al., in a retrospective study of 260 patients with renal and ureteral stones, also encountered this correlation, with a better outcome in stones located in the ureter than renal stones [10]. Nevertheless, this latest study defined treatment success as an SFR of < 4 mm at twelve weeks, not solely stone fragmentation. Most published research does not emphasize stone location as a major predictor of stone disintegration; it appears to be more relevant when related to the stone clearance rate. Stones located in the lower renal pole, when treated, tend to leave fragments that remain in the calyx and cause recurrent stone formation. The reported SFR for lower pole calculi is 25–95% [29], compared to the SFR of 32% in our study.
The second outcome defined in our work, the retreatment rate, is probably even more relevant for treatment selection. Stone fragmentation is an important factor when evaluating the effectiveness of ESWL but does not translate to its overall success. This is because even in cases where fragmentation is successful, additional interventions may be necessary if residual fragments exceed 4 mm and the patient continues to experience symptoms. Upon analyzing our findings, 30% (77 cases) of the cohort with successful fragmentation still needed further intervention. The definition of retreatment is, however, different between studies. The overall success of ESWL in our study increases from 63 to 83.5%, if we set the retreatment outcome including or excluding another session of ESWL, respectively. There is a trend towards a higher success rate in studies that consider treatment to be successful when they include one to three ESWL sessions (Table 1).
Our findings indicate that the maximum stone size measured on KUB can predict the need or retreatment, aligning with the majority of literature. It’s worth noting that we measured size on KUB rather than NCCT, which may lead to discrepancies in results due to its lower sensitivity. However, other studies have also measured stone size in KUB and had similar results. One such example is the study by Ng et al. in which 2489 patients were assessed using ultrasound and KUB alone. A statistically significant correlation (p < 0.001) was also found between size and treatment success (stone-free status after one session at three months of follow-up) [13]. The study by Perks et al. measured stone size with KUB and NCCT, with similar results in terms of correlation to stone fragmentation [20].
NCCT is a widely accepted imaging method to characterize stone disease; the information obtained through this method, namely stone density, size, and SSD, has been widely studied and related to ESWL efficacy. The preliminary studies of Joseph et al. [17] and Pareek et al. [4] first described a significant correlation between stone disintegration and MAV. After these, a relevant part of the discussion in the literature was related to the standardization of MAV measurement [6]. We adopted the same method as Müllhaupt et al., defining regions of interest just smaller than the stone in magnified images [16]. Different measuring methods can justify distinct results in the literature. As in the study by Müllhaupt et al., our study did not show any correlation between MAV and stone disintegration. However, when the defined treatment outcome was the need for retreatment, a significant correlation was found, with a cut-off value of 827 HU. This result is similar to the one described by Wiesenthal et al., in which the treatment outcome was also defined as a single-treatment success, with a cut-off value of 900 MAV [7].
The measuring method of SSD did not vary among studies [19]. In our results, SSD could not predict treatment outcomes in both its definitions. Although the majority of literature supports the predictive value of SSD in treatment success, some studies align with our findings. Yl et al. conducted a retrospective study of 115 patients with renal stones who underwent more than one ESWL session. They found no correlation between SSD and an SFR of < 3 mm at one-month follow-up (p = 0.501) [22]. Another example is the study by Kang et al., also with a retrospective nature, that evaluated 399 patients with ureteral stones who underwent a single ESWL session [25].
An important consideration is whether NCCT is strictly necessary for treatment decision. It is generally accepted that NCCT allows for a superior assessment of stone disease. However, good patient selection also seems to be possible using KUB alone, namely assessing stone size. In our study, the sensitivity and specificity of MAV as a predictor of treatment success is higher compared to stone size alone; the AUC of the ROC curve is 0.729, compared to the AUC of stone size, 0.613. However, the difference between groups in both treatment outcomes did not reach statistical significance. Also, the predicting value of stone size demonstrated in our study seems to be lower compared to the results of other studies. In the prospective study by Wang et al. that included 80 patients with renal stones, both stone size and stone density were significant predictors of treatment outcome (SFR ≤ 4 mm in NCCT at three months). The AUC for stone size was higher than stone density (0.855 and 0.768, respectively) [18]. Another example is the retrospective study by Park et al., which included 115 patients with renal stones. Here, the AUC between stone density and size did not differ significantly (stone density: 0.874; stone size: 0.827, p = 0.388) [22]. On the other hand, in the prospective study from Yoshida et al., which included 62 patients with renal and proximal ureteral stones, MAV had a better negative predictive value than maximal diameter (78.6% compared to 66.7%), being treatment failure residual fragments bigger than 3 mm after three ESWL sessions [6]. Tanaka et al. analyzed 75 patients retrospectively and described MAV as the only independent predictor of ESWL success (AUC of 0.692) [9]. These conflicting results leave room for discussion about whether it is mandatory to assess patients with NCCT for treatment selection.
Our study is not without limitations. Its retrospective nature implies a lack of standardization in assessing patients before treatment, particularly in terms of imaging. This comparison was, nevertheless, one of the aims of this study. NCCT images were acquired using different devices, with collimation adapted to each patient, differing from some prospective studies. Patients were assessed by different physicians using KUB images, usually less sensitive for detecting residual fragments. However, this reflects the usual practice among urologists; we believe that studies should be tailored to the reality of clinical practice.
Conclusions
The selection of treatment for renal and ureteral stones should prioritize stone location and size, as widely accepted in the scientific community. The choice of imaging modalities for patient evaluation seems to have advantages both ways. In linear cases, KUB offers a fast, easily accessible imaging modality for treatment decision, with a proven value in the prediction of treatment outcome. NCCT provides more precise information for clinicians and patients, which can be useful in cases at high risk of disintegration failure, minimizing unnecessary exposure to shock waves and radiation.
Data availability
Data is provided within the manuscript.
References
Lv G, Qi W, Gao H, Zhou Y, Zhong M, Wang K et al (2022) Safety and efficacy of extracorporeal shock wave lithotripsy vs. flexible ureteroscopy in the treatment of urinary calculi: a systematic review and meta-analysis. 9, Front Surg. https://doi.org/10.3389/fsurg.2022.925481
Chung DY, Kang DH, Cho KS, Jeong WS, Jung H, Do, Kwon JK et al (2019) Comparison of stone-free rates following shock wave lithotripsy, percutaneous nephrolithotomy, and retrograde intrarenal surgery for treatment of renal stones: A systematic review and network meta-analysis. PLoS One. 2019;14(2). https://doi.org/10.1371/journal.pone.0211316
Rassweiler J, Rieker P, Rassweiler-Seyfried MC (2020) Extracorporeal shock-wave lithotripsy: is it still valid in the era of robotic endourology? Can it be more efficient? Current Opinion in Urology, vol 30. Lippincott Williams and Wilkins, pp 120–129. https://doi.org/10.1097/MOU.0000000000000732
Pareek G, Armenakas NA, Fracchia JA (2003) Hounsfield units on computerized tomography predict stone-free rates after extracorporeal shock wave lithotripsy. Journal of Urology. May 1;169(5):1679–81. https://doi.org/10.1097/01.ju.0000055608.92069.3a
Gupta NP, Ansari MS, Kesarvani P, Kapoor A, Mukhopadhyay S (2005) Role of computed tomography with no contrast medium enhancement in predicting the outcome of extracorporeal shock wave lithotripsy for urinary calculi. BJU Int 95(9):1285–1288. https://doi.org/10.1111/j.1464-410X.2005.05520.x
Yoshida S, Hayashi T, Ikeda J, Yoshinaga A, Ohno R, Ishii N et al (2006) Role of volume and attenuation value histogram of urinary stone on noncontrast helical computed tomography as predictor of fragility by extracorporeal shock wave lithotripsy. Urology 68(1):33–37. https://doi.org/10.1016/j.urology.2006.01.052
Wiesenthal JD, Ghiculete D, John D’A, Honey R, Pace KT (2010) Evaluating the importance of mean stone density and skin-to-stone distance in predicting successful shock wave lithotripsy of renal and ureteric calculi. In: Urological Research. 2010. pp. 307–13. https://doi.org/10.1007/s00240-010-0295-0
Shah K (2010) Predicting effectiveness of extracorporeal shockwave lithotripsy by Stone Attenuation Value. J Endourol 1169–1173. https://doi.org/10.1089/end.2010.0124
Tanaka M, Yokota E, Toyonaga Y, Shimizu F, Ishii Y, Fujime M et al (2013) Stone attenuation value and cross-sectional area on computed tomography predict the success of shock wave lithotripsy. Korean J Urol 54(7):454–459. https://doi.org/10.4111/kju.2013.54.7.454
Nakasato T, Morita J, Ogawa Y (2015) Evaluation of Hounsfield Units as a predictive factor for the outcome of extracorporeal shock wave lithotripsy and stone composition. Urolithiasis. Feb 1;43(1):69–75. https://doi.org/10.1007/s00240-014-0712-x
Celik S, Bozkurt O, Kaya FG, Egriboyun S, Demir O, Secil M et al (2015) Evaluation of computed tomography findings for success prediction after extracorporeal shock wave lithotripsy for urinary tract stone disease. Int Urol Nephrol Jan 1;47(1):69–73. https://doi.org/10.1007/s11255-014-0857-0
Pace KT, Weir MJ, Tariq N, John D’R, Honey A (2000) Low success rate of repeat shock wave lithotripsy for ureteral stones after failed initial treatment. J Urol Vol 164:1905–1907. https://doi.org/10.1016/S0022-5347(05)66914-5
Ng CF, Wong A, Tolley D (2007) Is extracorporeal shock wave lithotripsy the preferred treatment option for elderly patients with urinary stone? A multivariate analysis of the effect of patient age on treatment outcome. BJU Int 100(2):392–395. https://doi.org/10.1111/j.1464-410X.2007.06909.x
Patel T, Kozakowski K, Hruby G, Gupta M (2009) Skin to Stone Distance is an independent predictor of Stone-Free Status following shockwave lithotripsy. J Endourology Pp 1383–1385. https://doi.org/10.1089/end.2009.0394
Elawady H, Mahmoud MA, Samir M (2022) Can we successfully predict the outcome for extracorporeal shock wave lithotripsy (ESWL) for medium size renal stones? A single-center experience. Urol J 89(2):235–239. https://doi.org/10.1177/03915603211016355
Müllhaupt G, Engeler DS, Schmid HP, Abt D (2015) How do stone attenuation and skin-to-stone distance in computed tomography influence the performance of shock wave lithotripsy in ureteral stone disease? BMC Urol 15(1). https://doi.org/10.1186/s12894-015-0069-7
El-Nahas AR, El-Assmy AM, Mansour O, Sheir KZ (2007) A prospective multivariate analysis of factors Predicting Stone disintegration by extracorporeal shock Wave lithotripsy: the Value of High-Resolution Noncontrast Computed Tomography. Eur Urol 51(6):1688–1694. https://doi.org/10.1016/j.eururo.2006.11.048
EAU Guidelines (2023) Edn. presented at the EAU Annual Congress Milan 2023. ISBN 978-94-92671-19-6
Perks AE, Schuler TD, Lee J, Ghiculete D, Chung DG, D’A Honey RJ et al (2008) Stone Attenuation and skin-to-Stone Distance on Computed Tomography predicts for Stone Fragmentation by Shock Wave lithotripsy. Urology 72(4):765–769. https://doi.org/10.1016/j.urology.2008.05.046
Joseph P, Mandal AK, Singh SK, Sankhwar SN, Sharma SK (2002) Computerized tomography attenuation value of renal calculus: can it predict successful fragmentation of the calculus by extracorporeal shock wave lithotripsy? A preliminary study. J Urol 167:1968–1971. https://doi.org/10.1016/s0022-5347(05)65064-1
Park Y, Il, Yu JH, Sung LH, Noh CH, Chung JY (2010) Evaluation of possible predictive variables for the outcome of shock wave lithotripsy of renal stones. Korean J Urol 51(10):713–718. https://doi.org/10.4111/kju.2010.51.10.713
Kang DH, Cho KS, Ham WS, Chung DY, Kwon JK, Choi YD et al (2006) Ureteral stenting can be a negative predictor for successful outcome following shock wave lithotripsy in patients with ureteral stones. Investig Clin Urol 57(6):408–416. https://doi.org/10.4111/icu.2016.57.6.408
Wang LJ, Wong YC, Chuang CK, Chu SH, Chen CS, See LC et al (2005) Predictions of outcomes of renal stones after extracorporeal shock wave lithotripsy from stone characteristics determined by unenhanced helical computed tomography: a multivariate analysis. Eur Radiol 15(11):2238–2243. https://doi.org/10.1007/s00330-005-2742-9
Ng CF, Siu DYW, Wong A, Goggins W, Chan ES, Wong KT (2009) Development of a Scoring System from Noncontrast Computerized tomography measurements to improve the selection of Upper Ureteral Stone for extracorporeal shock Wave lithotripsy. J Urol 181(3):1151–1157. https://doi.org/10.1016/j.juro.2008.10.161
Choi JW, Song PH, Kim H (2012) Predictive factors of the outcome of extracorporeal shockwave lithotripsy for ureteral stones. Korean J Urol 53(6):424–430. https://doi.org/10.4111/kju.2012.53.6.424
Wu H, Wang J, Lu J, Wang Y, Niu Z (2016) Treatment of renal stones ≥ 20 mm with extracorporeal shock wave lithotripsy. Urol Int 96(1):99–105. https://doi.org/10.1159/000441424
Waqas M, Saqib I, ud din, Jamil MI, Khan MA, Akhter S (2018) Evaluating the importance of different computed tomography scan-based factors in predicting the outcome of extracorporeal shock wave lithotripsy for renal stones. Investig Clin Urol 59(1):25–31. https://doi.org/10.4111/icu.2018.59.1.25
Yoon JH, Park S, Kim SC, Park S, Moon KH, Cheon SH et al (2021) Outcomes of extracorporeal shock wave lithotripsy for ureteral stones according to ESWL intensity. Transl Androl Urol 10(4). https://doi.org/10.21037/tau-20-1397
Alić J, Heljić J, Hadžiosmanović O, Kulovac B, Lepara Z, Spahović H et al (2022) The efficiency of extracorporeal shock Wave lithotripsy (ESWL) in the treatment of distal Ureteral stones: an unjustly forgotten option? Cureus. https://doi.org/10.7759/cureus.28671
Acknowledgements
Special thanks to Cláudia Machado, radiology technician performing ESWL in Unidade Local de Saúde de Santo António, for giving technical insights to the manuscript.
Funding
Open access funding provided by FCT|FCCN (b-on).
Author information
Authors and Affiliations
Contributions
Beatriz Oliveira (B.O.), Bernardo Teixeira (B.T.), and Vítor Cavadas (V.C.) contributed to the study conception and design. Material preparation, data collection and analysis were performed by B.O., Nuno Vinagre (N.V.), and Martinha Magalhães (M.M.). The first draft of the manuscript was written by B.O. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
This study was approved by the Ethics Committee of Unidade Local de Saúde de Santo António (130-DEFI/122-CE). The study was performed by the ethical standards as laid down in the 1964 Declaration of Helsinki.
Conflict of interest
The authors have no conflicts of interest to report.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oliveira, B., Teixeira, B., Magalhães, M. et al. Extracorporeal shock wave lithotripsy: retrospective study on possible predictors of treatment success and revisiting the role of non-contrast-enhanced computer tomography in kidney and ureteral stone disease. Urolithiasis 52, 65 (2024). https://doi.org/10.1007/s00240-024-01570-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00240-024-01570-7