Abstract
Background
Head and neck cancer is the most common cancer in males and fifth most common in females in India. Inadequate screening programs and non-availability of local healthcare resources leads to late diagnosis and most cases present at an advanced stage. Surgical extirpation often results in complex, large defects. The concept of chimerism is useful in dealing with such extensive defects.
Methods
Between July 2013 and May 2017, all patients who underwent primary reconstruction of head and neck defects following cancer extirpative surgery, with ALT-AMT chimera flap at a tertiary care cancer centre were included in this study. The patient data of age, sex, etiology, defect size, flap size, perforator configuration, anastomotic details, donor site closure, and complications was retrospectively collected as per the designated proforma from the hospital electronic record, departmental case record forms and the first author’s personal logs, and analyzed.
Results
Chimeric flaps based on the lateral circumflex femoral artery i.e. ALT plus AMT provide the desired qualities to address the complex defects. All thirteen patients had a large intraoral mucosal defect. Nine cases had a large extra oral skin defect. The average size of ALT was (112.5 cm2 area) and of AMT was (94.9 cm2 area). The combined area of ALT AMT was 28.5 X 9 = 256.5 cm2. All AMT pedicles were joining the ALT pedicle. 1 AMT was lost and all donor sites needed skin grafting.
Conclusion
Chimeric ALT + AMT is a valuable option when complex, large, multidimensional and multicomponent defects need to be reconstructed. The advantage of utilising a single donor site and two independent flaps with a single microvascular anastomosis.
Level of Evidence: Level IV, therapeutic study
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Head and neck cancer is the second most common cancer in developing countries [1]. It is the most common cancer of males in India and the fifth most common in females [2]. Inadequate screening programs and non-availability of local healthcare resources leads to late diagnosis and most cases presenting at an advanced stage. Surgical extirpation often results in large, complex, and anatomically nonadjacent defects, and demands a flexible flap with multi-planar, easily configurable multiple paddles with easy and superior maneuverability (http://globocan.iarc.fr/Pages/fact_sheets_population.aspx) which in turn provides greater contouring potential to line mucosa, surface skin and / or fill cavities. This often translates into superior cosmetic and functional results.
Several reconstructive options might be available for reconstruction of such complex defects like two local cutaneous, pedicled fascio-cutaneous flaps or a pedicled flap along with a microvascular free flap or two free flaps. Local and pedicled flaps are not desirable owing to lack of versatility in design and limited soft tissue availability. Multiple free flaps add to the operative time, donor morbidity and leads to the search of an alternative option [3].
The antero-lateral thigh flap (ALT) has become the workhorse flap for soft tissue reconstruction in head neck surgeries because of familiar anatomy, multiple perforator availability, and feasibility of chimerism with tensor fascia lata flap (TFL), antero-medial thigh flap (AMT) and vastus lateralis (VL) / rectus femoris (RF) muscle. Here, we are presenting our experience of reconstructing such extensive defects where we have used ALT with AMT as a chimera. The objective of this report is to assess the therapeutic efficacy, including the feasibility and predictability of reconstructing large multiplanar defects of the head and region using chimeric ALT AMT flaps.
Materials and methods
Between July 2013 and May 2017, a total of 13 patients (12 male, 1 female) underwent primary reconstruction of head and neck defects following cancer extirpative surgery, with ALT-AMT chimera flap at a tertiary care cancer centre. (Table 1). The patient data of age, sex, etiology, defect size, flap size, perforator configuration, anastomotic details, donor site closure, and complications was retrospectively collected as per the designated proforma from the hospital electronic record, departmental case record forms and the first author’s personal logs, and analyzed. Patients were discharged 5–10 days following the surgery and postoperatively followed up twice weekly for first 2 weeks, fortnightly for a month and then 3 monthly for an year and 6 monthly thereafter.
Surgical technique
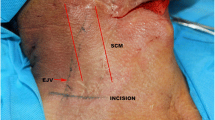
Standard markings were done for ALT axis and perforator mapping. Hand held Doppler (8 MHz) was used for locating perforators on thigh pre-operatively. Initial incision was 7 to 8 cm long, 2.5 cm medial to the ALT perforator doppler marking. This initial incision was purposely kept straight and non-commital which kept the AMT territory intact if needed. It also allowed proximal or distal extension depending on perforator availability. The ALT perforator was identified at the point where it was entering the deep fascia. Then according to the three dimensional requirement of the defect, the size of flap paddles and the need of chimerism, perforators were identified and selected and skin paddles marked. The order of preference was given as mentioned:
-
1.
If only one paddle (isolated mucosal defects) was required and the perforator was available and satisfactory, ALT flap was harvested. It could be harvested with or without vastus lateralis muscle to fill soft tissue defect and maxillary cavity.
-
2.
If two ALT perforators were available and two paddle were required (mucosa + skin defects), the ALT paddle was divided to provide suitable inset.
-
3.
If only one ALT perforator was available where 2 paddles were required along with large soft tissue requirement as well, then the AMT perforator was searched and identified, and chimeric ALT-AMT flap was harvested.
-
4.
If AMT was not available then the incision was extended proximally curving posteriorly and TFL perforator was dissected and a chimeric ALT-TFL flap was harvested (as it has more donor site graft related complications at TFL site than ALT-AMT flap).
This report details the ALT AMT chimeric flaps done as per above protocol. The AMT perforators were identified by medial dissection over the rectus femoris muscle. Once the ALT and AMT perforators are identified, the flap paddles were planned. (Figure 1) The strength or size of perforators and thickness of the medial and lateral flaps were the factors taken into consideration for deciding which flap paddle is to be utilized for mucosa, skin or as cavity filler Figs 2, 3 and 4.
Left buccal mucosa squamous cell carcinoma (SCC) (Defect – Left hemimandibulectomy with subtotal palatectomy with ITF clearance with outer skin) reconstructed with ALT AMT flap (a) Left buccal mucosa SCC (b) Defect Left hemimandibulectomy with subtotal palatectomy with ITF clearance with outer skin (c) ALT AMT flap (d) After inset
The perforators were dissected in a freestyle manner, from perforator to pedicle for both ALT and AMT, irrespective of the septocutaneous or musculocutaneous course. Attempt was made to preserve all the nerves to vastus lateralis and rectus femoris and also to preserve the muscles in every case. AMT and ALT pedicles were meeting in all cases, so only one microvascular anastomosis was required. The pedicle was dissected upto lateral circumflex femoral artery (LCFA) or profunda femoris artery (PFA) till the desired length was achieved. These flaps were inset as planned and part of the flap was used as filler, as required. Microvascular anastomosis was done after inset. The flap was monitored by pinprick every 2 hourly for 24 h and 6 hourly for 5 days thereafter. Anticoagulants were used for deep venous thrombosis prophylaxis for 5 days. Orals were started after 5th postoperative day and then the patients were discharged as per postoperative recovery and complications if any.
Results
All 13 patients had a large intra oral mucosal defect. 9 cases had a large extra oral skin defect.(Table 1) The defects ranged from through and through buccal mucosa defects, palatal defects and infrastructural maxillectomy defects with extra oral skin defects. 3 cases were post previous radiotherapy. All AMT pedicles were joining the ALT pedicle. In 9 cases, the ALT perforator was arising from descending branch and from oblique branch in 4 patients. 8 perforators had a septo-cutaneous course while 5 had musculo-cutaneous course. Only 1 set of microvascular anastomosis were needed in all cases. (Table 2).
The ALT component of flap was used for inner lining in 4 patients and for outer lining in 2 patients, while the AMT component was used for inner lining in 3 patients, as filler in 1 patient and for outer lining in 3 patients. The average size of ALT harvested was 15 X 7.5 cm = 112.5 cm2 area and from AMT we harvested 13 X 7.3 cm = 94.9 cm2 area. The combined area of ALT AMT was 28.5 X 9 = 256.5 cm2. (Table 3) The largest flap which could be harvested individually was 25 X 13 cm with effective area of 325 cm2. But, with chimersim largest flap which could be harvested was 45 X 13 cm with effective area of 585 cm2.
Table 3: Showing increase in effective area of combined flaps.
The donor sites were covered with a split thickness skin graft (STSG). There was no significant graft site morbidity, patients could mobilize completely after graft take. But no objective evaluation of leg function was performed. 1 arterial thrombotic event occurred with loss of AMT flap only, ALT flap was salvaged. Another AMT, used for skin lining, had partial necrosis and needed a pectoralis major myocuteneous flap, same patient had some native skin necrosis too. 2 cases dehiscence of flap inset.AMT allowed additional amount of skin and adequate subcutaneous tissue to be transferred to the defect.
The minimum follow up was 6 months after surgery and maximum follow up was 18 months with median of 9 months. Eight patients were deceased at 12 months, 3 patients had recurrence and kept on palliation, 2 patients were doing well at 18 months followup.
Discussion
In India, majority of head and neck cancers present as locally advanced Stage III/IV disease [4]. As the incidence and diagnosis of oral cancer increase, excision of the head and neck cancers frequently yield large, complex three dimensional defects which test the limits of the reconstructive surgeons and thereby obligates imaginative planning and surgical astuteness. Since its description in 1984 by Song et al. [5], ALT flap has become the preferred flap for reconstruction in varied settings. Other good options for these extensive defects are the flaps on scapular parascapular axis but these require change in position. Deep inferior epigastric artery/ vertical rectus abdominis flaps, second free flap are also other feasible options in this situation.
The thigh has revealed itself to be a mine of reconstructive options [6] and particularly the lateral circumflex femoral (LCF) axis allows the use of skin (ALT, AMT, TFL), muscle (TFL, VL) in various combinations. ALT, TFL and AMT flaps can be harvested in a chimeric fashion [7] in cases requiring large skin cover with or without filler.
AMT flap has been found to have a variable vascularity with the perforator not being found in 21% cases in a study by Selber et al. [8]. When present, it might be originating from descending branch of LCFA, superficial femoral artery or profunda femoris artery. [9]. We have made it a protocol to do a doppler evaluation of perforators of both ALT and AMT but even the presence of the Doppler signal doesn’t guarantee amenability to plan a chimeric flap and the perforators need to be traced before the flap can be committed. To circumvent the problem of variability of perforators, initially a single incision taken about 2.5 cms ahead of the septum allows harvest of a flap on either ALT and / or AMT or the TFL perforator. The authors used no imaging owing to logistic issues but they recommend the use of pre-operative CT-Angiography for planning chimeras as this would avoid intraoperative uncertainty and prevent surprises.
Bandi et al. [10] have described the use of ALT- Rectus femoris chimeric flap for reconstruction of various defects. But the study did not include gait analysis even though the muscle forms an important part of the knee extending mechanism and removing it carries a theoretical risk of compromising the same.
Lin et al. [11] have described the following factors in favor of chimeric flaps over double free flaps namely, the need for more than one pair of recipient vessels or a flow-through flap (in the limbs), morbidity of the second flap harvest and the additional time for second anastomosis. These hold true in the head neck reconstruction too. Additionally, it allows higher efficiency in terms of maximal use of the available tissue at the donor site. AMT allowed additional amount of thick skin, with an additional vascular source. Separate and adequately long pedicle of AMT allows it to move and rotate independently from the ALT for better contouring of the construct. This is especially useful when the mucosal and skin defect are in different axis. It also adds an extra perforator and vascular source to the overall flap volume. It adds extra skin, soft tissue bulk and volume to the flap when needed. Separate components of the chimera enable easy movement of tissues in different orientations and dimensions. It allows independent insetting of each component, covers large surface areas, restore volume and contour, use a single recipient vascular site, have a single donor site morbidity, and provision of monitoring the flap, especially in cases where the flap is buried [12]. In cancer patients with debilitated body habitus, AMT flap provides welcome bulk for filler.
ALT-AMT chimera flaps have also been described for coverage of large abdominal [13], chest wall [14] and lower limb defects [15]. Chimeric flaps may be used when the sheer requirement of the lining tissue is more; or in the different parts of the field or even as one of the paddles de-epithelialized fully or partially to provide bulk and add volume, while the other forms the lining.
The largest flap which could be harvested individually was 25 X 13 cm with effective area of 325 cm2. But, with chimersim, the largest flap which could be harvested was 45 X 13 cm with effective area of 585 cm2. This large flap was almost impossible to harvest without chimerism. AMT territory is slightly more thicker than ALT and used to give fill the cavity wherever required according to the defects.
Scapular—parascapular flap with or without thoracodorsal perforator flap can also be a very good alternative in this situation but will require position change. Divided vertical deep inferior epigastric artery flap can also be a vital solution in these cases as per body habitus and perforator availability. Second free flap is always an option and the decision is more of surgeon’s preference [16].
Small sample size, retrospective nature of study, with suboptimal follow up on functional aspect of donor sites are the main limitations of this article. But, this article can be useful by providing an alternate chimeric combination of ALT with AMT whenever feasible and required and this ALT-AMT can also be additional armamentarium.
Conclusion
Although the chimeric ALT + AMT flap is a valuable option when complex, large, multi-dimensional and multi-component defects need to be reconstructed. The advantages of utilizing a single donor site and two independent flaps with a single microvascular anastomosis with reduced total operative time. But the vascular anatomy variability, donor site morbidty should be considered with utilization of this option.
Data Availability
Data will be made available by the author when requested.
References
NICPR (2017) National Institute of Cancer Prevention and Research Program
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127(12):2893–2917. https://doi.org/10.1002/ijc.25516
Longo B, Nicolotti M, Ferri G, Belli E, Santanelli F (2013) Sagittal split osteotomy of the fibula for modelling the new mandibular angle. J Craniofac Surg 24:71–74
Jiang C, Guo F, Li N, Liu W, Su T, Chen X et al (2014) Multipaddled Anterolateral Thigh Chimeric Flap for Reconstruction of Complex Defects in Head and Neck. PLoS ONE 9(9):e106326
Shah SB, Sharma S, D’Cruz AK (2016) Head and neck oncology: The Indian scenario. South Asian J Cancer 5(3):104–105. https://doi.org/10.4103/2278-330X.187572
Song YG, Chen GZ, Song YL (1984) The free thigh flap: A new free flap concept based on the septocutaneous artery. Br J Plast Surg 37:149–159
Acartürk TO (2011) Femur-vastus intermedius-anterolateral thigh osteomyocutaneous composite chimeric free flap: A new free flap for the reconstruction of complex wounds. J Reconstr Microsurg 27:187–194
Huang WC, Chen HC, Jain V, Kilda M, Lin YD et al (2002) Reconstruction of through-and-through cheek defects involving the oral commissure, using chimeric flaps from the thigh lateral femoral circumflex system. Plast Reconstr Surg 109:433–441
Yu P, Selber J (2011) Perforator patterns of the anteromedial thigh flap. Plast Reconstr Surg 128:151e-e157
Koshima I, Hosoda M, Inagawa K, Moriguchi T, Orita Y (1996) Free medial thigh perforator-based flaps: New definition of the pedicle vessels and versatile application. Ann Plast Surg 37:507–515
Hallock GG (2017) The Chimera Flap: A quarter century odyssey. Ann Plast Surg 78(2):223–229
Bandi S, KoteswaraRao RV, Reddy DM (2016) One plus one: Two free flaps from same donor thigh for simultaneous coverage of two different defects. Indian J Plast Surg 49(2):191–197
Lin YT, Lin CH, Wei FC (2006) More degrees of freedom by using chimeric concept in the applications of anterolateral thigh flap. J Plast Reconstr Aesthet Surg 59:622–627
Baumann DP, Butler CE (2013) Soft Tissue Coverage in Abdominal Wall Reconstruction. Surg Clin N Am 93:1199–1209
Tan PWW, Wong CH, Koong HN, Tan BK (2010) Chest wall reconstruction using a combined musculocutaneous anterolateral–anteromedial thigh flap. Indian J Plast Surg 43(1):88–91
Shetty N, Mashalkar NS, Ellur SR, Kagodu K (2016) Double free-flap for a bimalleolar dfect of lower leg and ankle. Indian J Plast Surg 49:95–98
Funding
Open access funding provided by Department of Atomic Energy. Nil.
Author information
Authors and Affiliations
Contributions
Dushjant Jaiswal, Raghav Shrotriya, Saumya Mathews, Mayur Mantri, Vineet Kumar and Ameya Bindu performed the surgeries. Dushyant Jaiswal and Vineet Kumar had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Dushyant Jaiswal, Raghav shrotriya and Vineet Kumar wrote the manuscript. Vinay kant Shankhdhar and Prabha Yadav reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
Not applicable.
Ethical approval
All procedures performed in studies involving human participants were by the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was notified to the hospital ethical committee and approval was not required being this a pure retrospective observational study.
Patient consent
Proper pre-procedure consents were taken for surgery, documentation and research purposes. Data storage was performed in consistence with good clinical practice guidelines.
Consent to participate
All the patients signed a written specific consent regarding the surgical procedure.
Consent to publish
All the patients signed a written consent about the use of data and images for scientific reasons.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jaiswal, D., Shrotriya, R., Kumar, V. et al. Managing complexity with chimerism: ALT-AMT flaps for complex head and neck reconstruction. Eur J Plast Surg 47, 61 (2024). https://doi.org/10.1007/s00238-024-02200-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00238-024-02200-6