Abstract
Background
In Italy, with a cohort of 6.3 million morbidly obese patients, panniculectomy is often necessary both in relation to bariatric surgery and as the sole treatment to reduce excess lower abdominal tissues. At first glance, the procedure could be misjudged as technically simple; however, when considering patients with Extreme obesity or worse (BMI > 40 kg/m2), the surgical risks increase significantly, patients are often inoperable, and few studies are available in the literature. Most surgeons actually avoid this job and related risks. Recent research has highlighted a potential role of the Bipolar Radiofrequency Scalpel (BRS) in various fields as a promising tool to reduce surgical complications. With this paper, the authors report their experience in the management of panniculectomy in Extreme (BMI > 40 kg/m2) and Super (BMI > 50 kg/m2) obese patients through the technique of BRS assisted panniculectomy.
Methods
A retrospective study was conducted on Extreme / Super obese patients who underwent BRS assisted panniculectomy between June 2013—June 2022. The panniculectomy involved lower abdomen excess skin and soft tissues removal, assisted by BRS, minimal undermining, and eventual abdominal hernia repair. Surgical procedures, and complications rate are discussed.
Results
Fourteen patients matched the selection criteria and were included in the study. Minor and major complications occurred in 28,6% and 14,3%, respectively. No flap necrosis, infections, cellulitis or decubitus ulcer occurred. Seroma 28,6% (4/14) and hematoma 7,1% (1/14) were the most relevant complications in the study population.
Conclusions
BRS assisted panniculectomy with minimal undermining is a valuable option for patients with extreme or super obesity. At the time of dissection, minimizing undermining and using BRS could make the operation safer and therefore extendable to a larger cohort of patients.
Level of evidence: Level IV, Therapeutic; Risk/Prognostic.
Similar content being viewed by others
Introduction
Obesity rate is increasing in Italy, with an estimated prevalence of 12% of obese people among the adult population [1], 6.3 million morbidly obese Italians [1], and over €13.34 billion in total estimated attributable costs in 2020 [2]. Given the burden of obesity, panniculectomy is often necessary either following bariatric procedures, or as sole treatment, to reduce the excessive and redundant abdominal skin and soft tissues.
Panniculectomy consists of surgical excision of defined adipocutaneous tissue volume from the lower abdomen [3]. At first glance, the procedure could be misjudged as a technically simple operation; however, the comorbidities of obese patients, the long duration of the procedures, and the extensive surgical dissections represent a major concern [4]. In addition, obesity causes vasculo-lymphatic hypertrophy of the abdominal region which persists even after post-bariatric massive weight loss. Indeed, patients are exposed to a high risk of intra and post-operative complications including bleeding, seroma, pain, wound dehiscence and infection [4].
As obesity worsens, the risks significantly increase [5]; moreover, the surgeries become considerably longer, and require special care including preoperative assessment, surgical technique, and follow-up. Accordingly, panniculectomies in patients with Extreme obesity or worse (BMI > 40 kg/m2) are poorly adopted, and, to the best of our knowledge, few studies are available in the present literature.
Recently, new technologies for surgical dissection have been developed to improve the surgical safety and reduce complications. In 1929, Bovie and Cushing first described energy dependent thermal coagulation tools. Since then, extended research has been carried out on energy—based technologies for surgical dissections. Among these, the Bipolar Radiofrequency Scalpel (BRS) is a new electrothermal bipolar vessel sealer available as an alternative to the traditional electrocautery in various surgical fields and several papers have reported a BRS related positive outcomes including bleeding reduction and shorter hemostasis time [6, 7].
With this paper, the Authors report their experience in the management of panniculectomy in patients with Extreme (BMI > 40 kg/m2) and Super (BMI > 50 kg/m2) obesity through the technique of BRS- assisted panniculectomy, with minimal undermining, and eventual abdominal hernia repair. Study procedure, surgical technique and outcomes are discussed.
Methods
Study design
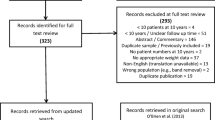
A retrospective chart review was conducted on patients with Extreme/Super obesity who underwent panniculectomy at the Plastic Surgery Unit of the University of Siena, between June 2013 and June 2022. Reasons for surgical intervention included abdominal dermal lipodystrophy with massive adipocutaneous excess, abdominal wall hernias, and abdominal elephantiasis. According to the American Society for Bariatric Surgery Obesity Classification [8], obesity was defined as Extreme if the BMI was greater than 40 kg/m2, Super if greater than 50 kg/m2. Surgical procedures consisted of targeted adipocutaneous tissue removal from lower abdomen through the technique of panniculectomy assisted by BRS, with minimal undermining, and eventual abdominal hernia repair.
Inclusion criteria consisted of patients with BMI > 40 kg/m2 that required panniculectomy either following a previous bariatric surgery, or as primary treatment/in preparation to bariatric surgery. All patients received at least 1 year of follow-up after surgery. Exclusion criteria were missing/incomplete patient demographics (age, weight, height, indication for surgery, surgical procedure, and weight of the resected pannus), as well as missing/incomplete follow up. Complications were defined as minor for any adverse event that did not require revision surgery and was followed by complete recovery. On the contrary, the major complications involved returning the patient to the operating room. All the enrolled patients provided their informed written consent. The study protocol followed the Principles of the Declaration of Helsinki.
The aim of the present article is to share the author’s personal experience with BRS assisted panniculectomy in dramatic cases of extreme obesity. The evaluation of the effectiveness of the BRS itself or the feasibility of other techniques for panniculectomy were not an outcome of the study; therefore, comparisons with alternative treatment strategies were not made.
Patient demographics, indications for surgery, surgical procedures, and post-operative complications rate were obtained from reevaluation of patients’ medical records and analyzed.
Preoperative evaluation
Multidisciplinary evaluation of Extreme/Super obese morbid patients undergoing panniculectomy is essential. All enrolled patients underwent abdominal CT to identify wall defects and/or hernias, venous color Doppler ultrasound for lower extremity thrombosis, and cardiology, pulmonary, and anesthesiology examinations for the assessment of overall surgical eligibility. Particular attention has been placed on pre-operative management of the metabolic syndrome through diet restriction, physical activity and appropriate pharmacological set. Nevertheless, the main concern was intra- and postoperative bleeding with anemia. Such problem is often burdened by the deficit in vitamin absorption of the post-bariatric patients. Consequently, a preoperative assessment of the hemoglobin level was performed, and patients were excluded for hemoglobin levels below 11 g/dL. In case of active cellulitis and/or severe intertrigo, patients underwent intravenous antibiotic treatment, and surgery was delayed until resolution of the acute infection.
Surgical technique
With the patient possibly standing upright, precise preoperative markings are made to obtain symmetrical, and camouflaged incisions. Patients with Extreme/Super obesity often present with a ptotic pubis, accordingly a low incision is chosen to obtain harmonious result. The lower limit of the resection is set at 6 cm from the base of the penis or the vulvar anterior commissure. Starting from this point, lateral markings are drawn up toward the anterior superior iliac spine. The lines are then extended laterally to include the excessive adipocutaneous apron. The upper limit is pre-signed, but the exact length will be determined during surgery (Fig. 1). Scars from prior surgery should be included in the resection if possible.
The surgical dissection begins with the suprapubic incision, Scarpa's fascia is identified, then it extends down to reach the suprafascial plane. The latter is followed cranially to isolate the panniculus. To preserve the lymphatic vessels, 5 mm thickness of subcutaneous tissue overlying the muscle fascia is spared. The dissection must necessarily address the presence of large caliber arterial, venous and lymphatic vessels of obese patients. In carrying out this procedure, the BRS (LigaSure Impact, Medtronic®) allows tissue dissection and concomitant vessels coagulation [6, 9], thus representing an optimal device for reducing intra- and postoperative bleeding and lymphatic leakage. If there are any vessels with a caliber greater than 3 mm, direct vessel ligation should be preferred with through absorbable stitches (polyglactin 3–0), especially in the periumbilical area where the perforating vessels of greater caliber are typically located. Eventually, hemostatic clips may also be used to achieve this purpose.
Once the panniculectomy is performed, the residual skin redundancy allows the surgeon to close primarily the defects with minimal or even non-existent undermining. Extensive dissections with larger dead spaces are not necessary, which on the contrary would dramatically increase postoperative complications such as hematomas and seromas. Therefore, undermining is minimized in an effort to maximize skin vascularity preservation and proper wound healing.
After complete dissection, the excess panniculus is removed and passed off of the table as a specimen for weight determination. In the event of abdominal hernia identification, hernioplasty procedure is performed. The umbilicus is transposed and sutured. In case of umbilical hernia or recurrent omphalitis, the umbilicus is removed and reconstructed with local flaps. To ensure a good approximation of the panniculectomy edges, a bevel incision is made to reduce any thickness difference, which is usually enhanced in patients with obesity (typically greater for the cranial than for the caudal edge). This technical detail, besides any aesthetic significance, promotes proper wound healing and dehiscence prevention. At the end of the procedure, two 19-French Blake drains are placed. The suture includes 3 complete layers (deep subcutis with Scarpa fascia approximation, superficial subcutis and intradermal suture). Finally, Dermabond® glue is applied on the wounds to further seal the sutures. A compression dressing is fixed, then the elastic band is placed and kept on for at least 1 month after surgery.
In consideration of the high risk of deep venous thrombosis and pulmonary embolism [10], all patients are preoperatively treated with subcutaneous injection of low-molecular-weight heparin 6000UI, then 4000UI per day until mobility is recovered, unless there are specific contraindications. The subcutaneous heparin injection site is usually the arm to avoid a higher concentration of drug in the abdomen. Antibiotics are administered intravenously during the surgery and continued orally until discharge. The drains are removed when drainage is less than 35 cc over a 24-h period. In the most challenging cases, the patient’s first postoperative day is programmed in the Sub-Intensive Care Unit (Table 1).
Results
Study population
From June 2013 to June 2022 14 patients, who underwent BRS assisted panniculectomy at the Plastic Surgery Unit of the University of Siena, matched the selection criteria and were enrolled in the study. The surgeries were performed by multiple surgical teams in which the senior author participated. Patients demographics are summarized in Table 2. The average age was 53,4 years old (range 39–72), 85,7% (12/14) were females, the average BMI was 46,22, (range 41,33–57,40), the average weight was 129,2 kg (range 100-180 kg), obesity was Extreme (BMI > 40) in 78,6% (11/14), Super (BMI > 50) in 21,4% (3/14). 28,6% (4/14) were smokers. Originally 6 (42,3%) underwent bariatric surgery. Of those participants 1 (16,7%) underwent gastric bypass, 2 (33,3%) one anastomosis gastric bypass (mini gastric bypass), and 3 (50%) sleeve gastrectomy. The average BMI at time of bariatric surgery was 63,2 (range 51–82,4,), the average time between bariatric surgery and panniculectomy was 4 years (range 2–10 years). The average weight loss prior to panniculectomy was 59,7 kg (21–80 kg).
The causes responsible for panniculectomy are summarized in Table 3. These included abdominal dermal lipodystrophy with massive adipocutaneous apron in 6 (42,9%), abdominal dermal lipodystrophy with massive adipocutaneous and abdominal wall hernias in 6 (42,9%), and abdominal elephantiasis in 2 (14,3%). The average weight of the excised panniculus specimen was 9,0 kg (range 6,3–19 kg). The average hemoglobin level prior and after surgery was 13,5 mg/dl (range 11,4–16,2 mg/dl) and 11,4 mg/dl (range 9,2–13,8 mg/dl) respectively (Table 4).
The average hospitalization time was 5 days (range 3–8). 13 out of 14 patients walked on the first postoperative day, 1 on the second. All patients received at least 1 year follow up after surgery, the average follow up was 46 months (range 13–115 months) (Figs. 2, 3, 4).
Thirty-nine-year-old Super obese patient (BMI 57,4) who underwent BRS assisted panniculectomy with removal of 19 kg pathological apron after 80 kg of weight loss following gastric bypass surgery performed 10 years earlier (maximum BMI reached 82.4). A, B, C: Preoperative evaluation. D, E, F: one-year follow up
Outcomes
Minor and major complication rate was 28,6% (4/14) and 14,3% (2/14) respectively (Table 5). No flap necrosis, infections, cellulitis or decubitus ulcer occurred. Hematoma occurred in 1 patient (7,1%) and required hemostasis revision in the operating room. Seroma was found in 4 (28,6%) patients and it was treated with repeated aspirations. Only one patient was brought back to the operating room for late seroma evacuation and drainage placement. Delayed umbilical healing was found in 2 patients (14,3%) but resolved within 2 months with no further complications. Two patients complained of moderate to severe pain after surgery, yet they recovered unremarkably.
Discussion
Obesity is growing worldwide at an alarming rate with US prevalence rates of 30–36% and 6.3% for obesity (BMI > 30 kg/m2) and Extreme obesity (BMI > 40 kg/m2) respectively [11]. The rates in Italy are lower, with 34.2% of overweight and mild obese people (BMI 25–30 kg/m2) and 12% of adult obese people (BMI > 30 kg/m2), which however represents 6,3 million adults Italians with obesity [1]. In parallel, the obesity related economic impact was estimated at €13.34 billion in Italy in 2020 [2], and over €147 billion in the US [12], representing up to 7% of all US health care spending.
As the obesity burden has increased in Italy and in US, surgery to treat obesity has become increasingly popular. Each year, more than 200,000 bariatric procedures are performed in the US [8]. Weight loss procedures are well documented to help alleviate comorbidities in obese patients such as diabetes, hyperlipidemia, hypertension, and obstructive sleep apnea [13]. In addition, bariatric and post-bariatric patients carry a higher prevalence of psychiatric comorbidities, including depression, anxiety, binge eating disorder, difficulty in self-regulation of emotional states and impulsive traits [14]. In such a scenario, panniculectomy is performed in body contouring procedures, to reduce the excessive and redundant abdominal skin and soft tissues, improve hygiene conditions and mobility, relieve back pain, and promote the overall quality of life, physically and psychologically.
Although the majority of patients undergoing bariatric surgery lose weight massively, there is a non-negligible percentage of patients who are still obese despite of their weight loss. Furthermore, some severely obese patients are so impaired, that they are not candidates for surgery, but still have a pathological apron [15, 16]. These patients constitute a small and selected cohort characterized by very high surgical risks but concomitant necessity of panniculectomy, to which this study is aimed.
Literature reveals a positive correlation between surgical complications and elevated BMI [5]. Data show a 15% to 80%. complication rate associated to panniculectomy on patients with obesity [3]. Zannis et al. [17] in a review on 563 panniculectomies, described a 3 to 15 times higher postoperative wound complication rate for BMI greater than 39 kg/m2. In addition, a positive correlation between resected panniculus size and postoperative wound complication rate was described by Neaman and Hansen by reviewing 26 abdominoplasties [18]. Finally, Gelidan et al. [19] recently conducted a retrospective study on 178 postbariatric patients who underwent abdominoplasty. The authors reported a hematoma rate of 2.8%. Interestingly, they found a statistically significant increase in the risk of hematoma for male smoking patients compared to female patients.
Noteworthy, due to the unstable clinical conditions and perioperative risks, most surgeons routinely deny this surgery, and this could explain both the small size of our cohort and the little literature available. However, given the worldwide progression of obesity, or rather of Globesity, these cohort will certainly become more and more numerous. It is therefore up to the scientific community to provide a concrete solution to a problem that is currently minimally addressed or neglected.
Recently, new technologies available in the operating room could represent a possible solution to increase the feasibility of surgical interventions in these challenging patients. In 1928, Bovie and Cushing first utilized energy dependent thermal coagulation instruments [20]. Since that time, technological advances have introduced the BRS as an alternative to traditional electrocautery. The BRS is a new electrothermal bipolar vessel sealer that allows concomitant tissues dissection and vessels coagulation, limiting overheating and tissue burn. It is a new energy-based scalpel characterized by reduced local impact and, today, it is widely adopted in various surgical fields and several studies on BRS have highlighted a reduced risk of bleeding and shorter hemostasis times [7, 21]. Its applications in plastic surgery include Güven et al. latissimus dorsi flap [22]. Konno and Kishi neurofibroma removal [23], and body contouring [6]. In our opinion, it could play a central role also in panniculectomy for patients with extreme and super obesity.
Although this indication (BRS + panniculectomy) is reasonable, to the best of our knowledge, there is limited information available in the present literature. Specifically, the use of BRS for panniculectomy in extreme and super obese patients is poorly described. Notably, the use of BRS is well known in the body contouring of ex- obese patients, suggesting that the association reported in this paper itself isn’t completely new [6]. Consistently, the lack of literature on BRS for panniculectomy in this specific category of patients (extreme/super obese) suggests that these patients are often neglected or excluded from the operating room. Pestana et al. [24] in 2014, described a series of 26 “supersize” panniculectomies. Despite their relatively numerous enrolled patients, the overall complication rate was 42.3%, thus demonstrating some criticalities.
In the present series, minor complications were found in 28,6% (4/14), but the major complications occurred in only 14,3% (2/14), thus showing encouraging data. Moreover, all patients recovered completely, suggesting appropriate treatment choice.
Overall, the management of these patients requires a multidisciplinary approach, with particular caution both in the preoperative phase and in the follow-up. However, the surgery itself must also be performed appropriately to reduce the burden of complications. Based on current reading and personal author’s experience, we believe that two technicalities helped achieving results. First, at the time of flap harvest, minimizing or avoiding undermining allowed to maximize skin vascularity and promote wound healing. Secondly, the BRS, by ensuring tissue resection and concomitant vascular and lymphatic vessels coagulation [9], promoted postoperative bleeding and lymphatic leakage reduction and hemostasis time shortening [7, 25,26,27,28].
Limitations of the study include the limited sample, variable follow-up duration, and lack of comparison with other surgical techniques. Specifically, the BRS was not compared with the traditional scalpel in terms of complications rate. Therefore, a truly blind randomized trial on a larger sample could be a plausible next step to confirm whether there really is an advantage in using the BRS compared to the traditional scalpel. Nevertheless, our study shows that these patients, with the necessary precautions, could access surgery. Overall, the hereby reported suggestions could represent decisive technicalities to reduce complications and extend surgical access to a greater number of patients.
Conclusions
The present study shows that BRS assisted panniculectomy, with minimal undermining, and eventual abdominal hernia repair is a valuable surgery for patients with Extreme/Super obesity. The procedure, when properly carried out, allows to increase mobility, decrease pain, increase hygiene and overall quality of life. At the time of dissection, minimizing undermining and using BRS appear to be key elements of the technique. Complications are frequent and sometimes unavoidable in these patients; however, proper execution makes this surgery not only a “dirty job” that nobody wants to do, but a viable therapeutic option even for patients with Extreme/Super obesity. We hope that our considerations can increase surgical access for this specific category of patients.
Data availability
Data are available on request due to privacy/ethical restrictions.
References
ISTAT (n.d.) Fattori di rischio per la salute: fumo, obesità, alcol e sedentarietà. 2021 June 22, 2023]; Available from: https://www.istat.it/it/archivio/270163
d’Errico M, Pavlova M, Spandonaro F (2022) The economic burden of obesity in Italy: a cost-of-illness study. Eur J Health Econ 23(2):177–192
Almutairi K, Gusenoff JA, Rubin JP (2016) Body contouring. Plast Reconstr Surg 137(3):586e–602e
Janis JE, Jefferson RC, Kraft CT (2020) Panniculectomy: practical pearls and pitfalls. Plast Reconstr Surg Glob Open 8(8):e3029
Livingston EH, Ko CY (2002) Assessing the relative contribution of individual risk factors on surgical outcome for gastric bypass surgery: a baseline probability analysis. J Surg Res 105(1):48–52
Pierazzi DM et al (2022) Ligasure impact and ligasure small jaw in body contouring after massive weight loss: a new perspective. J Invest Surg 35(3):659–666
Soon PS et al (2006) Use of the ligaSure vessel sealing system in laparoscopic adrenalectomy. ANZ J Surg 76(9):850–852
Mechanick JI et al (2008) American association of clinical endocrinologists, the obesity society, and american society for metabolic & bariatric surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Endocr Pract 14(Suppl 1):1–83
Heniford BT et al (2001) Initial results with an electrothermal bipolar vessel sealer. Surg Endosc 15(8):799–801
Samad F, Ruf W (2013) Inflammation, obesity, and thrombosis. Blood 122(20):3415–3422
Flegal KM et al (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 307(5):491–497
CDC (n.d.) Obesity Facts. Centers for Disease Control and Prevention. February 27, 2020 June 22, 2023]; Available from: https://www.cdc.gov/obesity/data/adult.html
Sugerman HJ et al (2003) Diabetes and hypertension in severe obesity and effects of gastric bypass-induced weight loss. Ann Surg 237(6):751–6 (discussion 757-8)
Sisto A, Barone M, Giuliani A, Quintiliani L, Bruni V, Tartaglini D, Persichetti P, Tambone V (2023) The body perception, resilience, and distress symptoms in candidates for bariatric surgery and post bariatric surgery. Eur J Plast Surg 46:417–425
Petty P et al (1992) Panniculus morbidus. Ann Plast Surg 28(5):442–452
Chernosky ME, Derbes VJ (1966) Elephantiasis nostras of the abdominal wall. Arch Dermatol 94(6):757–762
Zannis J et al (2012) Outcome study of the surgical management of panniculitis. Ann Plast Surg 68(2):194–197
Neaman KC, Hansen JE (2007) Analysis of complications from abdominoplasty: a review of 206 cases at a university hospital. Ann Plast Surg 58(3):292–298
Gelidan AG, H.M.H.A, Mortada H, Alkahtani FSA, Arab K, Kattan AE, Alfaqeeh FA (2023) The preoperative risk factors for hematoma development following postbariatric abdominoplasty: a retrospective analysis of 178 patients. Eur J Plast Surg. https://doi.org/10.1007/s00238-023-02046-4
Massarweh NN, Cosgriff N, Slakey DP (2006) Electrosurgery: history, principles, and current and future uses. J Am Coll Surg 202(3):520–530
Susini P, Pozzi M, el Araby Mohamed M, Cuomo R, Nisi G (2024) Abdominal elephantiasis—end stage disease or treatable disorder? case report, surgical technique and review of the literature. Indian J Surg. https://doi.org/10.1007/s12262-023-04009-2
Guven E et al (2010) Electrothermal bipolar vessel sealer in endoscope-assisted latissumus dorsi flap harvesting. J Laparoendosc Adv Surg Tech A 20(9):735–742
Konno E, Kishi K (2012) Use of the LigaSure vessel sealing system in neurofibroma excision to control postoperative bleeding. J Plast Reconstr Aesthet Surg 65(6):814–817
Pestana IA et al (2014) “Supersize” panniculectomy: indications, technique, and results. Ann Plast Surg 73(4):416–421
Ding Z, Wable M, Rane A (2005) Use of Ligasure bipolar diathermy system in vaginal hysterectomy. J Obstet Gynaecol 25(1):49–51
Franko J et al (2006) Safely increasing the efficiency of thyroidectomy using a new bipolar electrosealing device (LigaSure) versus conventional clamp-and-tie technique. Am Surg 72(2):132–136
Sadeghi P, Duarte-Bateman D, Ma W, Khalaf R, Fodor R, Pieretti G, Ciccarelli F, Harandi H, Cuomo R (2022) Post-Bariatric Plastic Surgery: Abdominoplasty, the State of the Art in Body Contouring. J Clin Med 11(15):4315. https://doi.org/10.3390/jcm11154315
Losco L et al (2022) Helix thigh lift. A novel approach to severe deformities in massive weight loss patients. J Invest Surg 35(3):620–626
Funding
Open access funding provided by Università degli Studi di Siena within the CRUI-CARE Agreement. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
“All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [Pietro Susini], [Davide Di Seclì] and [Giuseppe Di Luiso]. The first draft of the manuscript was written by [Pietro Susini] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.”
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. The University of Siena Research Ethics Committee has confirmed that no ethical approval is required.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Figures 2, 3, 4.
Conflict of interest
Pietro Susini, Mirco Pozzi, Gianluca Marcaccini, Davide di Seclì, Giuseppe Diluiso, Francesco Ruben Giardino, Roberto Cuomo, Luca Grimaldi, and Giuseppe Nisi report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Susini, P., Pozzi, M., Marcaccini, G. et al. Extreme—Super obesity and panniculectomy: bipolar radiofrequency scalpel assisted surgery as a valuable option for the most challenging cases. Eur J Plast Surg 47, 46 (2024). https://doi.org/10.1007/s00238-024-02195-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00238-024-02195-0