Abstract
Background
Acellular dermal matrices (ADM) are widely used in direct-to-implant breast reconstruction and were introduced as part of the implant-based breast reconstruction within the previous decade. This study presents clinical outcomes of ADM-assisted direct-to-implant breast reconstruction and evaluates the most frequent and severe postoperative complications.
Methods
We performed a retrospective analysis of patients who underwent ADM-assisted submuscular direct-to-implant breast reconstruction from March 2013 to February 2017 at the University Hospital Copenhagen, Rigshospitalet. All postoperative complications were classified using the Clavien Dindo classification of surgical complications. We used univariate and multivariate analyses with Fisher’s exact test and multiple logistic regression to determine potential risk factors.
Results
A total of 102 breast reconstructions were carried out in the inclusion period. The incidence rate of severe skin flap necrosis and surgical site infection was 6% and 4%, respectively. The total rate of skin flap necrosis was 14.7%, surgical site infection 11.8%, rotation of anatomical implants 4.90%, seroma 3.92%, dynamic breast deformity 1.96% and hematoma 1.96%. No patients suffered from red breast syndrome or capsular contracture. Total explantation rate was 4.90%. The median follow-up period was 32 months.
Conclusion
This study demonstrates an acceptable rate of explantation in ADM-assisted direct-to-implant breast reconstruction. We found that skin flap necrosis and surgical site infection were the most frequently occurring complications with low rates of severe cases. However, there is a need for larger, controlled studies to further explore the impact of patient and surgery related risk factors.
Level of evidence
Level III, Risk/Prognostic.
Similar content being viewed by others
Introduction
Implant-based breast reconstruction is the most frequently used method for breast reconstruction following a mastectomy [1]. According to the literature, skin flap necrosis and surgical site infection are the most frequent complications affecting 18–20% and 7–12% of the patients, respectively [2,3,4]. Due to the acute nature of these complications, it is important to have detailed knowledge of their rate of occurrence. Moreover, seroma and red breast syndrome are speculated to have an increased incidence of occurrence in ADM-assisted reconstruction [5].
The use of acellular dermal matrix (ADM) in direct-to-implant breast reconstructions is widespread [6,7,8]. The use of ADM may improve the aesthetic outcome and minimize the risk of complications such as capsular contracture [9,10,11]. Previous studies present a wide interval of complication rates of 5–47% in relation to ADM-assisted breast reconstructions [3, 12,13,14,15,16,17]. Previous studies have not been able to identify a statistically significant patient or surgery-related risk factors [2, 13, 18, 19] except for a Danish single-center observational study from 2021 reporting a significant association between infection and postoperative chemotherapy and between skin flap necrosis and bilateral procedure [3]. Hence, multiple studies are needed so that they can be combined in future meta-analyses solely focusing on ADM-assisted direct-to-implant breast reconstruction.
In this study, we investigate the rate of postoperative complications with a long-term follow-up period of 2.3 years with emphasis on skin flap necrosis and surgical site infection in 59 consecutive women (102 breasts) undergoing submuscular implant-based breast reconstruction with ADM. Additionally, we investigate potential risk factors for skin flap necrosis and surgical site infection.
Patients and methods
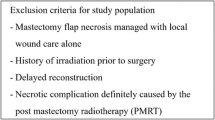
This retrospective study was performed according to the STROBE guidelines for observational studies. All women who underwent direct-to-implant breast reconstruction with ADM between March 2013 and February 2017 were included in the study. Data were assessed by a retrospective review of the patient’s medical records. Patient demographics and surgical characteristics were collected according to predefined variables.
Surgical indications involved oncological treatment of carcinoma, ductal carcinoma in situ, or risk-reducing treatment due to genetic or hereditary disposition to breast cancer. The selection of ADM-assisted breast reconstruction depended on various factors including patient comorbidity, oncologic safety, and skin flap potential [2, 20]. Patients were considered ineligible for the surgery if they were active smokers or had a BMI below 17, medical history with radiation therapy, or poor skin flap potential (exposed dermis). Patients with poor flap quality based on a perioperative clinical evaluation were converted to breast reconstruction with an expander and were excluded from the analysis. All patients were scheduled for follow-up visits two weeks and three months after surgery.
Surgical technique
All mastectomies were performed by a breast surgeon and the direct-to-implant breast reconstruction was performed by a plastic surgeon. Three different plastic surgeons performed the breast reconstructions. Initially, the plastic surgeon made a clinical evaluation of the flap quality. If the skin flap quality was considered adequate, a submuscular cavity was created under the pectoralis major muscle with the release of the inferior attachments and interposition of a sheet of acellular dermal matrix covering the lower half of the implant. The tissue matrix Strattice was used in all included patients. Two drains were placed: One axillary and one inframammary. All patients received 1.5 g of prophylactic intravenous cephalosporin perioperatively. This dosage was repeated on the first postoperative day and the patient received 1 gram of orally administered dicloxacillin four times a day until the drains were removed. Specialist follow-up was scheduled three and 12 months after surgery.
Endpoints
The primary endpoints were complications such as skin flap necrosis, surgical site infection, seroma, and red breast syndrome. Skin flap necrosis was defined as either necrotic tissue or epidermolysis around the incision. Surgical site infection was defined by suspicion of the surgeon and was based on the presence of cicatricial erythema, soreness, or local edema and treated with empirical antibiotics. Redbreast syndrome was defined as erythema localized to the area overlying the ADM and thus, differentiated from surgical site infection by a clinical evaluation of the extent and location of the erythema. Formation of seroma was either assessed by ultrasound or aspiration of fluid surrounding the ADM and the degree of capsular contracture was graded using the four-grade Baker classification scale. Additionally, we investigated the association between potential risk factors (surgical experience, specimen weight, incision type, and implant size) and postoperative complications.
All postoperative complications were classified using the Clavien Dindo classification of surgical complications. Each complication was categorized as either mild (CDC grade I-IIIa) or severe (CDC IIIb). Mild complications were defined as complications treated conservatively or with debridement in local anesthesia. Severe complications were defined as complications requiring surgical interventions under general anesthesia e.g. explantation or replacement of implant due to rotation [21].
Statistical analysis
Statistical analyses were performed using R for Statistical Computing (version 1.1.456) and a p-value < 0.05 was statistically significant. Patient demographic data was described with a median and interquartile range (IQR) for non-normally distributed continuous data and frequencies in percent for categorical data (Table 1). Univariate analyses were elaborated for each risk factor followed by a multivariate analysis for risk factors found empirically relevant (the surgeon’s surgical experience, specimen weight, type of incision, and implant size). Both analyses were presented with the percentage of complications and odds ratio (OR) including a 95% confidence interval and p-value (Tables 2 and 3). Statistical comparisons were performed using Fisher’s exact test for single categorical variables and multiple logistic regression for numeric variables or numerous categorical variables.
Results
A total of 59 women (102 breasts) were included in the study of which 43 women underwent bilateral reconstruction and 16 women underwent unilateral reconstruction. The median age was 41 years (IQR 34–50 years), and the median body mass index was 23 kg/m2 (IQR 21–26 kg/m2). Ten breasts (10%) received adjuvant chemotherapy, 33 breasts (32%) received neoadjuvant chemotherapy, and nine breasts (8.8%) had received chemotherapy in relation to treatment for a previous cancer. In total, 52 of the breasts underwent risk-reducing mastectomies, and the remaining 50 breasts were treated due to carcinoma, ductal carcinoma in situ (DCIS), or both. The median specimen weight was 306 g (IQR 226–393 g). A periareolar incision was used in 54 breasts and a nipple-sparing incision in 48 breasts. The median implant size was 385 cc (IQR 311–485 cc). The median follow-up period was 32 months (IQR 22–38 months). No recurrence of cancer was detected. For an overview of patient demographics and surgical characteristics see Table 1.
Clavien Dindo classification
Twenty-nine breasts (28%) developed one or more postoperative complications categorized as CDC grade I to IIIb. Ten of the complications occurred bilaterally whereas the remaining 19 complications occurred unilaterally. In 17 breasts (17%) the complications were categorized as mild (CDC grade I-IIIa) whereas 12 breasts (12%) were categorized as severe (CDC grade IIIb). No patients developed sepsis or other life-threatening complications (CDC grade IV-V). Mild complications occurred after a median time of 18 days (IQR 9–30 days) and severe complications occurred after a median time of 78 days (IQR 22–226 days). According to skin flap necrosis, mild complications occurred after a median time of 18 days (IQR 8–30 days) and severe complications occurred after a median time of 26 days (IQR 18–29 days). Mild and severe complications due to surgical site infection occurred after a median time of 13 days (IQR 9–26 days) and 19 days (IQR 13–33 days), respectively. Complications due to the formation of seroma were all categorized as mild (CDC grade IIIa) and occurred after a median time of 19 days (IQR 17–21 days). Table 4 demonstrates the CDC distribution of complication types.
All analyses were performed with ‘breast’ as the sampling unit. To adjust for the correlation between data in patients undergoing bilateral breast reconstruction we used a generalized estimating equation (GEE) model for uni- and multivariate logistic regression analyses [22, 23].
Clinical endpoints
Skin flap necrosis was observed in 15 breasts (15%) distributed in 13 patients and occurred after a median time of 22 days (IQR 12–30 days). Nine of the 15 breasts (8.8%) were classified as mild requiring no treatment, pharmacologic treatment, or minor revision surgery (CDC grad I-IIIa) and the remaining six breasts (6%) were classified as severe cases requiring surgery in general anesthesia (CDC grade IIIb). Two patients developed bilateral skin flap necrosis (four breasts) and 11 patients developed unilateral skin flap necrosis (11 breasts). The patients had a median age of 39 years (IQR 34–48 years) and a median body mass index of 23 kg/m2 (21–27 kg/m2). Two patients had a history of smoking (two breasts). Five patients (six breasts) received neoadjuvant chemotherapy before the surgery. The median specimen weight was 358 g (IQR 276–387 g) and the median size of the implant was 390 cc (IQR 375–405 cc).
Surgical site infection was observed in 12 breasts (12%) distributed in 10 patients after a median time of 16 days (IQR 9–26 days). Eight of the 12 breasts (7.8%) were classified as mild (CDC grade I-IIIa) whereas four breasts (3.9%) required major revision surgery (CDC grade IIIb). The infections occurred bilaterally in two patients (four breasts) and unilaterally in eight patients (eight breasts). The patients had a median age of 37 years (IQR 34–47 years) and a median body mass index of 23 kg/m2 (IQR 22–26 kg/m2). One patient had a history of smoking. Five breasts received neoadjuvant chemotherapy before the surgery. Three patients (three breasts) were treated exclusively due to surgical site infection of which one patient underwent a complicated treatment period with intravenous cefuroxim, irrigation of gentamicin directly in the cavity, and lastly, two weeks of tablet dicloxacillin and rifampicin due to staphylococcus aureus. The remaining two patients with isolated surgical site infections were treated successfully with dicloxacillin.
A total of five breasts (5%) had an implant explantation. One breast (1%) was explanted due to skin flap necrosis with no records of initial treatment. Nine breasts (8.8%) presented with a combination of surgical site infection and skin flap necrosis of which four breasts (3.9%) underwent implant explantation. Two of these breasts were initially treated with dicloxacillin and wound revision in local anesthesia but eventually underwent implant explantation after 109 days. The remaining two breasts were initially treated with ‘negative pressure wound therapy’ for 13 and 26 days before converting to explantation of the implant.
Two breasts (2.0%) presented with bilateral dynamic breast deformity and had two sessions of fat grafting to conceal the distortion. There were no cases presented with red breast syndrome or capsular contracture. Four breasts (3.9%) presented with seroma and were all treated successfully with compression bra, aspiration and drain either with or without adding antibiotics. Implant rotation occurred unilaterally in five breasts (4.9%). Three of these had the implants replaced, which was considered a severe complication (CDC grade IIIb). Hematoma occurred unilaterally in two breasts (2.0%) within 12 and 24 h, respectively. Both hematomas were evacuated under general anesthesia. The distribution of complication types is demonstrated in Table 5.
Multivariate analysis
There was no statistically significant association between the risk of flap necrosis or infection and the surgeons’ surgical experience (OR 0.994, 95% CI 0.976–1.01, P = 0.49). Neither did we find a statistically significant association between the risk of flap necrosis or infection and the weight of the resected tissue specimen (OR 1.00, 95% CI 0.998-1.00, P = 0.51), an implant size more than 600 cc (OR 0.173, 95% CI 0.01–2.11, P = 0.17) or the use of a non-nipple-sparing incision (OR 0.653, 95% CI 0.218–1.96, P = 0.45). See Table 3.
Discussion
Kalstrup et al., Salzberg et al., and our study comprise the largest populations investigating complications in patients undergoing submuscular direct-to-implant ADM-assisted breast reconstruction with a long-term follow-up [3, 24]. Previous larger studies have been focused on capsular contracture, the prepectoral approach, or include two-staged surgery [17, 25,26,27,28,29,30]. Skin flap necrosis and surgical site infection were the most frequently occurring complications. Skin flap necrosis had a median time of debut of 22 days (IQR 12–30 days) and a total incidence rate of 15% which is in line with previous studies [2, 3, 13, 31]. Surgical site infection had a median time of debut of 16 days (IQR 9–26 days) and occurred in 12% which is similar to previously published studies [2, 13, 31, 32]. However, this differs from Kalstrup et al. who reported a lower incidence of infection of 7%, and Potter et al. who reported a higher incidence of infection of 22–25% within three months of follow-up [3, 33]. Notably, the incidence rates of skin flap necrosis and surgical site infection requiring revision in general anesthesia including explantation (CDC grade IIIb) of our cohort were 6% and 4%, respectively. Moreover, two patients registered with skin flap necrosis were treated with prophylactic antibiotics whereas registration of surgical site infection was based on clinical suspicion without confirmed presence of bacterial cultures. These outcome reports might have led to an overestimation of both skin flap necrosis and surgical site infection.
The formation of a seroma is a known adverse event in prosthetic breast reconstruction and according to Kim et al. the incidence of seroma formation is significantly increased in the setting of ADM-assisted implant-based breast reconstruction [34]. Additionally, Nahabedian et al. and Kalstrup et al. present a mean incidence of seroma of 5% (range 0–24%) and 7% [3, 5], respectively, which is in line with our study cohort presenting an incidence of 4%.
Our study cohort showed no patients with capsular contracture. In 2016 Salzberg et al. assessed the incidence of capsular contracture in 1584 direct-to-implant ADM-assisted breast reconstructions with an average follow-up period of 4.7 years. They found an incidence of 0.8% of which all capsular contractures had their debut within two years. Based on this record and due to a median follow-up period of 32 months (2.3 years) in our cohort, we can conclude that our study findings support a low rate of capsular contracture in direct-to-implant ADM-assisted breast reconstructions [30, 35]. This finding is in line with Kelley et al. who report an incidence of capsular contracture of 0% when investigating 201 one- or two-staged breast reconstructions with ADM [17].
Recently, Murphy et al. presented a review and meta-analysis investigating the efficacy and safety of ADM in breast reconstruction by comparing human ADM, xenograft ADM, and synthetic mesh with no ADM [36]. Notably, the analysis included reconstructions using a tissue expander at the time of mastectomy. When comparing no ADM with the three types of ADM they found a statistically significant reduction of overall complications, infection, and seroma formation in the group of no ADM compared to human ADM. No significant difference was found when comparing no ADM with xenograft ADM.
We found that 17 out of 28 complications were mild according to the Clavien Dindo classification (CDC grade I-IIIa) and 12 complications were classified as severe (CDC grade IIIb) of which only nine breasts (8.8%) remained in the group of severe complications when excluding the elective procedures of implant replacement due to rotation. This differs from an incidence of severe complications of 29% in a cohort presented by Dikmans et al. in 2017 despite a restricted patient selection [16]. We discovered a large difference in time of debut amongst mild and severe complications indicating that late-onset complications require a lower threshold for initiating treatment. This is supported by Franchelli et al. who reported a significantly lower treatment success rate in late-onset infections (12% vs. 41%, P = 0.009) [37]. Opposite was reported by Sinha et al. who reported that the consequences of late surgical site infection are just as serious as early surgical site infection [38].
The Joint Guidelines from the Association of Breast Surgery and the British Association of Plastic, Reconstructive, and Aesthetic Surgeons from 2021 emphasized the importance of patient selection when using ADM in breast reconstruction. Based on a multicentre, prospective cohort study from 2019 the guidelines recommend clinical consideration for patients who were active smokers, had a BMI below 17, a medical history with radiation therapy, or a poor skin flap potential (exposed dermis) which is in line with the surgical exclusion criteria of our study cohort [8, 33]. In fact, no patients with a history of radiation is offered implant-based reconstruction in Denmark resulting in a naturally exclusion of these patients in our cohort. This provides us with an analysis of the outcomes related specifically to ADM-assisted direct-to-implant breast reconstruction allowing for a more accurate assessment of the technique’s efficacy and safety profile.
To evaluate the number of procedures compared to two-staged breast reconstruction, we accumulate the number of direct reconstructions with the number of IIIb-complications as well as secondary contralateral implantations. In the case of two-stage breast reconstruction, each of the 59 patients should have undergone surgery twice, resulting in a total of 118 surgeries conducted under general anesthesia. Notably, without the adjacent complications requiring surgery. Our study cohort had 59 direct-to-implant breast reconstructions plus 12 IIIb-complications plus one contralateral implantation resulting in a total of 72 surgeries under general anesthesia. Additionally, eight breasts underwent lipofilling and two breasts underwent excision of excess skin, both procedures being performed under local anesthesia. In summary, our study cohort presents with a substantially lower number of procedures compared to the alternative approach with two-stage breast reconstruction.
The endpoints of this study may contribute to a future meta-analysis with the necessary power to investigate potential risk factors for postoperative complications in direct-to-implant ADM-assisted breast reconstruction. Previous studies were inconsistent when reporting an association [2,3,4, 13, 18, 30, 39,40,41,42,43,44], however, throughout our analyses no risk factors were found to be significantly associated with the development of complications (Table 2). We performed a multivariate analysis of four empirically relevant risk factors despite the small size of events and thereby, a risk of overfitting. Throughout all analyses, we acknowledged the correlation in bilateral reconstructions, however, found no association between the development of complications and surgical experience, specimen weight, non-nipple-sparing incision, or implant size in line with several previous studies [3, 13, 18].
The skin flap quality plays a crucial role when it comes to the risk of developing complications [2, 20, 45]. Intraoperative indocyanine-green and laser-assisted fluorescence angiography (SPY-systems) can be used to guide the surgeon in need of further tissue resection, flap revision, or even conversion to tissue expander [45, 46]. We were not able to make an intraoperative quality assessment of the skin flap nor include the experience of the breast surgeons in our study cohort.
We investigate the terms of safety and the risk of complications compared to two-staged breast reconstruction with tissue expander and prepectoral direct-to-implant breast reconstruction. Our study cohort presented a complication rate of 28% (95% CI 19–36) which is comparable with previous studies [12,13,14,15]. Reconstruction with an expander has an expected complication rate of 27% according to a large prospective study [47]. However, this is not in line with Manrique et al. who reported a significantly lower complication rate of 12% [48]. Furthermore, our study cohort presented with an explantation rate of 5% similar to Lohmander et al. who reported an explantation rate of 5% for 64 breast reconstructions with ADM within a follow-up period of six months when excluding patients with a history of radiotherapy [4]. This meets the gold standard of < 5% for complications leading to explantation in ADM-assisted breast reconstruction presented by Martin et al. [15].
Representing a paradigm shift in post-mastectomy breast reconstruction, surgeons are reinvestigating the efficacy of prepectoral direct-to-implant reconstruction considering new surgical and technological advances [49, 50]. A systematic review of ADM-assisted prepectoral direct-to-implant breast reconstruction is presented by Antony et al. revealing a wide-ranging complications rate interval of 2–53% [50]. This emphasizes the necessity of providing powerful comparison analyses between submuscular and prepectoral breast implant placement.
A controlled cost-analysis of ADM in submuscular, implant-based breast reconstruction performed by Aliotta et al. represents a sample size of 50 direct-to-implant breast reconstructions and covers a follow-up period of 11 months. They reported no significant difference in several surgeries due to complications in direct-to-implant breast reconstruction with ADM compared with two-stage reconstruction with or without ADM [51]. In addition, the group of direct-to-implant breast reconstruction with ADM had significantly fewer total postoperative visits and significantly less total operative time compared with the two other groups. Conclusively, these findings confirm the benefits of decreased total surgery time for patients as well as surgeons and healthcare systems and are supported by several previous studies [52,53,54].
In terms of limitations and despite an acceptable sample size, the number of events is quite small which makes generalization difficult and increases the risk of overlooking possible associations between risk factors and complications. Furthermore, being a single-institution study contains both methodological advantages and disadvantages. Notably, the patient selection develops dynamically as well as a gradual improvement of the surgical experience which causes an increasing risk of selection bias.
Conclusions
In conclusion, our study cohort presents an acceptable rate of explantation in ADM-assisted direct-to-implant breast reconstruction with no significant association between risk factors and postoperative complications. Furthermore, our findings support a low rate of red breast syndrome, dynamic breast deformity, seroma, and capsular contracture. However, there is a need for larger, controlled studies and meta-analyses to further explore the impact of patient and surgery-related risk factors.
References
Quinn TT, Miller GS, Rostek M, Cabalag MS, Rozen WM, Hunter-Smith DJ (2016) Prosthetic breast reconstruction: indications and update. Gland Surg 5(2):174–186
Dikmans RE, El Morabit F, Ottenhof MJ, Tuinder SM, Twisk JW et al (2016) Single-stage breast reconstruction using strattice: a retrospective study. J Plast Reconstr Aesthetic Surgery: JPRAS 69(2):227–233
Kalstrup J, Balslev Willert C, Brinch-Møller Weitemeyer M, Hougaard Chakera A, Hölmich LR (2021) Immediate direct-to-implant breast reconstruction with acellular dermal matrix: evaluation of complications and safety. Breast 60:192–198
Lohmander F, Lagergren J, Roy PG, Johansson H, Brandberg Y et al (2019) Implant based breast Reconstruction with Acellular dermal matrix: Safety Data from an Open-label, Multicenter, Randomized, Controlled Trial in the setting of breast Cancer Treatment. Ann Surg 269(5):836–841
Nahabedian MY (2019) Prosthetic breast Reconstruction and red breast syndrome: demystification and a review of the literature. Plast Reconstr Surg Glob Open 7(5):e2108
Spear SL, Parikh PM, Reisin E, Menon NG (2008) Acellular dermis-assisted breast reconstruction. Aesthetic Plast Surg 32(3):418–425
JoAnna Nguyen T, Carey JN, Wong AK (2011) Use of human acellular dermal matrix in implant- based breast reconstruction: evaluating the evidence. J Plast Reconstr Aesthet Surg 64(12):1553–1561
Whisker L, Barber M, Egbeare D, Gandhi A, Gilmour A et al (2021) Biological and synthetic mesh assisted breast reconstruction procedures: joint guidelines from the Association of Breast Surgery and the British Association of Plastic, reconstructive and aesthetic surgeons. Eur J Surg Oncol 47(11):2807–2813
Basu CB, Leong M, Hicks MJ (2010) Acellular cadaveric dermis decreases the inflammatory response in capsule formation in reconstructive breast surgery. Plast Reconstr Surg 126(6):1842–1847
Leong M, Basu CB, Hicks MJ (2015) Further evidence that human acellular dermal matrix decreases inflammatory markers of capsule formation in implant-based breast reconstruction. Aesthet Surg J 35(1):40–47
Salzberg CA (2006) Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm). Ann Plast Surg 57(1):1–5
Loo YL, Haider S (2018) The Use of Porcine Acellular dermal matrix in Single-stage, Implant-based Immediate breast Reconstruction: a 2-center Retrospective Outcome Study. Plast Reconstr Surg Glob Open 6(8):e1895
Sheena Y, Ball J, Benyon SL, Forouhi P, Malata CM (2018) The comparison of Strattice and SurgiMend in Acellular dermal Matrix-Assisted, Implant-based Immediate breast Reconstruction. Plast Reconstr Surg 142(5):789e–90e
Hallberg H, Rafnsdottir S, Selvaggi G, Strandell A, Samuelsson O et al (2018) Benefits and risks with acellular dermal matrix (ADM) and mesh support in immediate breast reconstruction: a systematic review and meta-analysis. J Plast Surg Hand Surg 52(3):130–147
Martin L, O’Donoghue JM, Horgan K, Thrush S, Johnson R, Gandhi A (2013) Acellular dermal matrix (ADM) assisted breast reconstruction procedures: joint guidelines from the Association of Breast Surgery and the British Association of Plastic, reconstructive and aesthetic surgeons. Eur J Surg Oncol 39(5):425–429
Dikmans RE, Negenborn VL, Bouman MB, Winters HA, Twisk JW et al (2017) Two-stage implant-based breast reconstruction compared with immediate one-stage implant-based breast reconstruction augmented with an acellular dermal matrix: an open-label, phase 4, multicentre, randomised, controlled trial. Lancet Oncol 18(2):251–258
Kelley RS, Duraes EFR, Scomacao IR, Van Dijck P, Fahradyan V et al (2022) A retrospective review of submuscular implant-based breast reconstruction: the influence of dermal matrix (ADM) on complications and aesthetic outcomes. J Plast Reconstr Aesthet Surg 75(11):4117–4124
Song J, Zhang X, Liu Q, Peng J, Liang X et al (2014) Impact of neoadjuvant chemotherapy on immediate breast reconstruction: a meta-analysis. PLoS ONE 9(5):e98225
Ball JF, Sheena Y, Tarek Saleh DM, Forouhi P, Benyon SL et al (2017) A direct comparison of porcine (Strattice™) and bovine (Surgimend™) acellular dermal matrices in implant-based immediate breast reconstruction. J Plast Reconstr Aesthetic Surgery: JPRAS 70(8):1076–1082
Radu M, Bordea C, Noditi A, Blidaru A (2018) Assessment of Mastectomy skin flaps for Immediate Implant-based breast Reconstruction. J Med Life 11(2):137–145
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Teerenstra S, Lu B, Preisser JS, van Achterberg T, Borm GF (2010) Sample size considerations for GEE analyses of three-level cluster randomized trials. Biometrics 66(4):1230–1237
Hanley JA, Negassa A, Edwardes MDd, Forrester JE (2003) Statistical analysis of Correlated Data using generalized estimating equations: an orientation. Am J Epidemiol 157(4):364–375
Salzberg CA, Ashikari AY, Koch RM, Chabner-Thompson E (2011) An 8-year experience of direct-to-implant immediate breast reconstruction using human acellular dermal matrix (AlloDerm). Plast Reconstr Surg 127(2):514–524
Lee KT, Mun GH (2016) Updated evidence of Acellular dermal matrix use for Implant-based breast Reconstruction: a Meta-analysis. Ann Surg Oncol 23(2):600–610
Jones G, Antony AK (2019) Single stage, direct to implant pre-pectoral breast reconstruction. Gland Surg 8(1):53–60
McCullough MC, Vartanian E, Andersen J, Tan M (2021) A sustainable Approach to Prepectoral breast Reconstruction using Meshed Acellular dermal matrix. Plast Reconstr Surg Glob Open 9(1):e3392
Capuano I BR, Varvaras D, Mattei M (2020) Acellular dermal matrix in prosthetic breast reconstructive surgery with Prepectoral technique: a Literature Review. J Exp Pathol 2020(12):50–59
Wagner RD, Braun TL, Zhu H, Winocour S (2019) A systematic review of complications in prepectoral breast reconstruction. J Plast Reconstr Aesthet Surg 72(7):1051–1059
Salzberg CA, Ashikari AY, Berry C, Hunsicker LM (2016) Acellular dermal matrix-assisted direct-to-Implant breast Reconstruction and Capsular Contracture: a 13-Year experience. Plast Reconstr Surg 138(2):329–337
Salzberg CA, Dunavant C, Nocera N (2013) Immediate breast reconstruction using porcine acellular dermal matrix (Strattice): long-term outcomes and complications. J Plast Reconstr Aesthetic Surgery: JPRAS 66(3):323–328
Glasberg SB, Light D (2012) AlloDerm and Strattice in breast reconstruction: a comparison and techniques for optimizing outcomes. Plast Reconstr Surg 129(6):1223–1233
Potter S, Conroy EJ, Cutress RI, Williamson PR, Whisker L et al (2019) Short-term safety outcomes of mastectomy and immediate implant-based breast reconstruction with and without mesh (iBRA): a multicentre, prospective cohort study. Lancet Oncol 20(2):254–266
Jordan SW, Khavanin N, Kim JYS (2016) Seroma in prosthetic breast Reconstruction. Plast Reconstr Surg 137(4):1104–1116
Headon H, Kasem A, Manson A, Choy C, Carmichael AR, Mokbel K (2016) Clinical outcome and patient satisfaction with the use of bovine-derived acellular dermal matrix (SurgiMend™) in implant based immediate reconstruction following skin sparing mastectomy: a prospective observational study in a single centre. Surg Oncol 25(2):104–110
Murphy D, O’Donnell JP, Ryan ÉJ, Lane O, Neill B, Boland MR et al (2023) Immediate breast Cancer Reconstruction with or without dermal matrix or synthetic mesh support: a Review and Network Meta-Analysis. Plast Reconstr Surg 151(4):563e–74e
Franchelli S, Pesce M, Savaia S, Marchese A, Barbieri R et al (2015) Clinical and microbiological characterization of late breast Implant infections after reconstructive breast Cancer surgery. Surg Infect (Larchmt) 16(5):636–644
Sinha I, Pusic AL, Wilkins EG, Hamill JB, Chen X et al (2017) Late Surgical-Site infection in Immediate Implant-based breast Reconstruction. Plast Reconstr Surg 139(1):20–28
Colwell AS, Tessler O, Lin AM, Liao E, Winograd J et al (2014) Breast reconstruction following nipple-sparing mastectomy: predictors of complications, reconstruction outcomes, and 5-year trends. Plast Reconstr Surg 133(3):496–506
Keifer OP Jr., Page EK, Hart A, Rudderman R, Carlson GW, Losken A (2016) A complication analysis of 2 Acellular Dermal Matrices in Prosthetic-based breast Reconstruction. Plast Reconstr Surg Glob Open 4(7):e800
Ball JF, Sheena Y, Tarek Saleh DM, Forouhi P, Benyon SL et al (2017) A direct comparison of porcine (strattice) and bovine (Surgimend) acellular dermal matrices in implant-based immediate breast reconstruction. J Plast Reconstr Aesthetic Surgery: JPRAS 70(8):1076–1082
Lanier ST, Wang ED, Chen JJ, Arora BP, Katz SM et al (2010) The effect of acellular dermal matrix use on complication rates in tissue expander/implant breast reconstruction. Ann Plast Surg 64(5):674–678
Chun YS, Verma K, Rosen H, Lipsitz S, Morris D et al (2010) Implant-based breast reconstruction using acellular dermal matrix and the risk of postoperative complications. Plast Reconstr Surg 125(2):429–436
Hunsicker LM, Ashikari AY, Berry C, Koch RM, Salzberg CA (2017) Short-term complications Associated with Acellular dermal matrix-assisted direct-to-Implant breast Reconstruction. Ann Plast Surg 78(1):35–40
Gurtner GC, Jones GE, Neligan PC, Newman MI, Phillips BT et al (2013) Intraoperative laser angiography using the SPY system: review of the literature and recommendations for use. Ann Surg Innov Res 7(1):1
Liu EH, Zhu SL, Hu J, Wong N, Farrokhyar F, Thoma A (2019) Intraoperative SPY reduces post-mastectomy skin flap complications: a systematic review and Meta-analysis. Plast Reconstr Surg Glob Open 7(4):e2060
Bennett KG, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG (2018) Comparison of 2-Year complication Rates among Common techniques for postmastectomy breast Reconstruction. JAMA Surg 153(10):901–908
Manrique OJ, Charafeddine A, Abu-Ghname A, Banuelos J, Jacobson SR et al (2019) Two-staged Implant-based breast Reconstruction: a long-term outcome study in a Young Population. Med (Kaunas). ;55(8)
Kaplan J, Wagner RD, Braun TL, Chu C, Winocour SJ (2019) Prepectoral breast Reconstruction. Semin Plast Surg 33(4):236–239
Antony AK, Robinson EC (2019) An Algorithmic Approach to Prepectoral Direct-to-Implant breast Reconstruction: Version 2.0. Plast Reconstr Surg 143(5):1311–1319
Aliotta RE, Duraes EFR, Scomacao I, Morisada M, Orra S et al (2021) A controlled cost and outcomes analysis of acellular dermal matrix and implant-based reconstruction. J Plast Reconstr Aesthet Surg 74(6):1229–1238
Colwell AS, Christensen JM (2017) Nipple-sparing mastectomy and direct-to-Implant breast Reconstruction. Plast Reconstr Surg 140:44s–50s 5S Advances in Breast Reconstruction)
Choi M, Frey JD, Alperovich M, Levine JP, Karp NS (2016) Breast in a day: examining single-stage Immediate, Permanent Implant Reconstruction in Nipple-Sparing Mastectomy. Plast Reconstr Surg 138(2):184e–91e
Endara M, Chen D, Verma K, Nahabedian MY, Spear SL (2013) Breast reconstruction following nipple-sparing mastectomy: a systematic review of the literature with pooled analysis. Plast Reconstr Surg 132(5):1043–1054
.
Funding
Open access funding provided by National Hospital. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Conception and design: LH, JF, MNH,and PG. Administrative support: LH, JF, MNH, and PG. Provision of study materials or patients: All authors. Collection and assembly of data: LH. Data analysis and interpretation: LH. Manuscript writing: All authors. Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Not required. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The participant has consented to the submission of their data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hansen, L., Paulsen, J.F., Hemmingsen, M.N. et al. Acellular dermal matrix in direct-to-implant breast reconstruction: univariate and multivariate analysis on potential risk factors . Eur J Plast Surg 47, 35 (2024). https://doi.org/10.1007/s00238-024-02182-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00238-024-02182-5