Abstract
Background
Penile skin inversion vaginoplasty (PIV) and sigmoid colon vaginoplasty (SCV) are both regarded as surgical options for gender reassignment surgery (GRS) to improve quality of life (QoL) in male-to-female (MTF) individuals. As no studies have compared the QoL between PIV and SCV techniques, this study aimed to evaluate the differences in QoL among MTF individuals who received PIV and SCV.
Methods
A cross-sectional study was conducted on patients who underwent GRS using PIV and SCV techniques at King Chulalongkorn Memorial Hospital (KCMH) from January 2002 to December 2022. The calibrated Thai version of Short-Form 36-Question Health Survey version 2 (SF-36v2) was used to assess QoL across eight health domains and to compare QoL between two surgical techniques.
Results
Of the 278 eligible MTF patients, who received GRS from 2002 to 2022, 57 completed the questionnaires; 37 and 20 MTF patients underwent PIV and SCV, respectively. Statistically significant difference was found in the Mental Component Summary (p-value = 0.02) of postoperative QoL between the two groups. SCV statistically outperformed PIV in seven out of eight domains.
Conclusion
In terms of QoL, MTF who underwent SCV showed better achievement than those who underwent PIV in most of the domains. Due to limitations of this study, further studies on a larger scale are needed to confirm the findings and compare other aspects of the surgical techniques.
Level of Evidence: Level III, Therapeutic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transsexualism [1], which overlaps with gender identity disorder (GID) [2], describes a condition when an individual has a strong desire to adjust their physical appearance to match their gender identification. The overall pooled prevalence of transsexualism of males, called male-to-female (MTF), was approximately 6.8 per 100,000 [3]. Moreover, recent studies have reported a trend of increasing prevalence of MTF to date [4,5,6,7,8,9]. Most MTF pursue treatments that aim to align their appearance to their desired gender and to improve their quality of life (QoL) [10]. To achieve the goals, MTF utilized a variety of therapeutic options including hormonal therapy [11,12,13] and surgical procedures such as breast augmentation, facial feminizing surgery, and gender reassignment surgery (GRS) [14].
The ultimate goal of GRS including penile skin inversion vaginoplasty (PIV) and sigmoid colon vaginoplasty (SCV) in MTF is to establish a female-like perineogenital complex in the aspects of function and appearance [15]. However, in assessing surgical outcomes, the success of the surgical techniques needed to be achieved along with patients’ well-being [16]. Various studies on GRS reported different outcomes in the aspect of QoL [17,18,19,20,21]. According to a survey on 47 Brazilian MTF who underwent PIV using the WHOQOL-100 questionnaire, there was a significant improvement in domains of psychological and social relationships but no significant change in domains of physical health and level of independence [17]. While a study on 31 MTF who underwent bowel vaginoplasty (BV) found that the total mean score using the Satisfaction with Life Scale (SWLS) was 27.7 ± 5.8, indicating high satisfaction [18].
PIV and SCV focused on fulfilling patients’ expectations in terms of function, aesthetic, and QoL. Since MTF are deemed to be in normal physical condition, the primary clinical purpose of the surgical procedures should be to improve QoL. Although several studies demonstrated the difference between PIV and BV in multiple aspects [22,23,24,25,26], there was no research comparing the QoL between techniques. Thus, this study focuses to compare the difference in QoL of MTF who underwent PIV and SCV.
Methods
Study design and sampling
This study was an open-label analytical cross-sectional study on patients who were diagnosed with gender identity disorder (GID) and underwent male-to-female (MTF) gender reassignment surgery (GRS) by penile skin inversion vaginoplasty (PIV) and sigmoid colon vaginoplasty (SCV) at King Chulalongkorn Memorial Hospital (KCMH), a tertiary referral university hospital in Thailand, from January 2002 to December 2022. Participants’ information was collected from the database of KCMH using ICD-10, which they were then recruited during the outpatient follow-up visits at the department. No sampling strategy was used in the study as we attempted to recruit all the eligible individuals.
The inclusion criteria were patients who (1) underwent PIV or SCV performed by the plastic and reconstructive surgery team of KCMH, (2) agreed to sign their informed consent, and (3) underwent the mentioned GRS surgeries for more than 3 months. The exclusion criteria are patients who (1) underwent PIV before SCV, (2) could not be contacted by their provided information, and (3) denied participating.
Procedure protocol
For GRS in KCMH, two main surgical operations were PIV and SCV. Three main surgeons performed both procedures and used the same approach. In brief, PIV technique uses penile skin and scrotal-perineal flap as a neovaginal lining. During SCV, the sigmoid colon was harvested laparoscopically by a general surgeon, and then the plastic surgery team dissected the perineum. Following that, the sigmoid colon was transplanted and sutured to the neovagina [27, 28].
Data collection
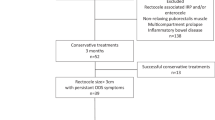
Patients were asked to complete the demographic data form and Short-Form 36-Question Health Survey version 2 (SF-36v2) by the researchers without a time limit and influence on the answers. The study flow diagram is shown in Fig. 1. The information was reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [29]. The reported checklist was provided in supplementary material 1.
The primary outcome of the study was health-related QoL using the SF-36v2. SF-36 questionnaire is a self- administered questionnaire consisting of 36 questions assessing QoL across eight domains including Physical Functioning, Physical Role, Bodily Pain, General Health, Vitality, Social Functioning, Emotional Role, and Mental Health [30]. These eight domains were categorized into the Physical Component Summary (PCS) and Mental Component Summary (MCS). The Physical Functioning, Physical Role, and Bodily Pain domains correlate highly with the PCS. The Emotional Role and Mental Health domains correlate highly with the MCS. Three of the domains (General Health, Vitality, and Social Functioning) correlate with both major component summaries. The Thai version of SF-36v2, which was calibrated by Lenette et al. to have no difference from the English version, was used in this study [31]. The response was calculated using norm-based scoring by using linear T-score transformations to make scores for component summary measures. Health domain scales have the same mean average of 50 and standard deviation of 10. A higher score in each domain indicates superior health [32].
Statistical analysis
The normal distribution of continuous variables was tested using visualization by histogram and the Shapiro–Wilk test. All continuous variables were represented as median (interquartile range) due to not normally distributed data. No descriptive variable was used in the study. The Mann–Whitney U-test was performed to compare the QoL between the PIV group and the SCV group. The probability of finding a statistically significant difference (power) in the non-significant QoL domains was estimated using alpha = 0.05 and the results from the study [33]. A p-value < 0.05 was considered statistically significant. Missing data and incomplete data were excluded from the statistical analysis. Stata version 17.0 (StataCorp, College Station, TX 77845 USA) was used for all data analysis.
Results
Baseline characteristics
From 2002 to 2022, a total of 278 eligible cases of MTF GRS were identified using ICD-10. Fifty-seven patients completed the questionnaires. Of these, 37 (64.9%) patients underwent PIV, and 20 (35.1%) patients received SCV. The median (IQR) age of the patients in the PIV and SCV groups was 30.0 (28.0–36.0) and 28.0 (24.0–37.0) years, respectively. The median (IQR) BMI of the patients in the PIV and SCV groups was 20.3 (18.6–21.4) and 19.9 (17.5–21.0) kg/m2, respectively. The median (IQR) age of self-recognition for patients in the PIV and SCV groups was 9.0 (5.0–16.0) and 9.0 (6.0–15.0) years, respectively. Other demographic characteristics including age of beginning living as a female, duration of living as a female before surgery, age of first hormone exposure, age of surgery, and postoperative satisfaction are demonstrated in Table 1. Between the two groups, demographic data revealed no statistically significant difference.
Quality of life (QoL)
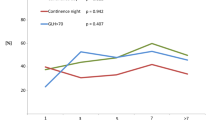
The PIV group demonstrated a median (IQR) QoL score of PCS of 51.9 (44.3–55.7), and the SCV group was at 54.0 (48.2–57.1). The median (IQR) of MCS scores in the PIV and SCV groups was 44.3 (37.0–52.3) and 51.2 (47.8–53.5), respectively. In terms of summary QoL, MCS demonstrated a statistically significant difference between the two groups (p = 0.02). In the subdomains, the SCV group showed significant differences in QoL than the PIV group in the seven out of eight domains except in the General Health domain (p = 0.08). Moreover, across all eight domains of QoL, the median values for each domain in the SCV group were higher than those in the PIV group. All results of the QoL in the study are shown in Table 2. The power estimations for PCS and the General Health domain were 0.22 and 0.51, respectively.
Discussion
This research was the first analytical cross-sectional study comparing the long-term postoperative quality of life (QoL) between penile skin inversion vaginoplasty (PIV) and sigmoid colon vaginoplasty (SCV). Statistically significant difference was found only in the Mental Component Summary (MCS) between the two groups. The lack of a significant difference in QoL between the two groups in the Physical Component Summary (PCS) could possibly be attributed to the similar treatment effects of both surgical techniques. However, it is more likely that the inadequate sample size for the study contributed to this outcome. Nevertheless, it is important to note that the values of PCS in both groups were close.
The use of well-constructed, reliable, and authorized questionnaires is important to help obtain data about the satisfaction and effectiveness of the surgery [34]. Globally used and validated instruments for evaluating health-related quality of life are SF-36 and WHOQOL-100 [35]. SF-36 questionnaire is a self-administered questionnaire consisting of only 36 questions [30], while WHOQOL-100 contains 100 questions [1]. Both questionnaires can be used to evaluate QoL, but SF-36 was used in this study, as the eight domains cover most measured health concepts and easy to collect information with high-quality data [30].
Most of the domains showed a statistically significant difference in SCV compared with PIV. The significantly higher score in seven out of eight domains in the SCV group may result from the SCV technique using the bowel as the vaginal canal lining which resembles the physiological female vagina in texture, appearance, and self-lubricating ability [36]. Therefore, it requires less postoperative self-neovaginal dilatation. A systematic review of surgical techniques demonstrated there were fewer neovaginal complications including neovaginal stricture and less wound dehiscence in the bowel vaginoplasty (BV) group compared with the PIV [22]. No statistically difference was found in General Health domain, reflecting respondents’ health status rating which might be due to the necessity of additional surgery to access the abdominal cavity for bowel segment harvesting, which could results in long-term intraabdominal complications such as constipation [23]. With a study power of 0.51 in the study, we cannot reject the possibility of an inadequate sample size to achieve a statistically significant difference.
From our study, the SCV group had higher median values in all the domains compared with the PIV group, implying SCV patients may have achieved better postoperative QoL. Following the surgery, functional and physical outcomes were strongly associated with patient satisfaction [37]. SCV is a reliable technique for achieving satisfactory vaginal depth that is both sexually functional and pleasing to the patient [38]. Additionally, MTF who received BV had high satisfaction with functional urogenital system and aesthetic aspects [18]. A meta-analysis on MTF also revealed that patients who underwent BV were more likely to achieve orgasm compared with PIV reflecting the ability to preserve genital sensation in BV [23]. Furthermore, high patients’ satisfactions were also associated with sexuality [39]. More than half of the PIV patients mentioned they were sexually inactive due to inadequate lubrication and discomfort during intercourse [40]. The naturally self-lubricating neovagina from SCV might improve sexual satisfaction and QoL.
There are no optimal techniques for GRS due to the unavailability of large comparative studies between available techniques. Nevertheless, the first line and most frequent technique used for vaginoplasty is PIV as it could fulfill patient satisfaction and is less invasive with no abdominal complications, and good functional and aesthetic outcomes [23, 24, 41]. On the contrary, PIV tended to result in stenosis, which is secondary to the wound healing process and skin graft contraction requiring adequate postoperative dilatation [42]. Additionally, the canal may get dry from the absence of natural lubrication [42]. These results could support our findings that the SCV group had better overall QoL than the PIV group. However, based on our center, SCV costs more than PIV according to the necessity of entering the abdominal cavity to harvest bowel segments. On the other hand, Brazilian trans women underwent GRS using the gold standard technique (PIV). QOL after GRS study in Brazilian society, most of the population were satisfied with GRS [43].
Other surgical options to increase QoL in MTF include facial feminization surgery (FFS) and breast augmentation surgery (BAS) [44]. Ainsworth et al. conducted a survey on MTF who underwent GRS and FFS and found that there was a significant improvement in QoL by SF-36v2 in physical, mental, and social aspects [45]. Moreover, a prospective cohort study revealed that FFS improved QoL with satisfying aesthetic outcomes and minimal complications [46]. Using the BREAST-Q questionnaire, Weigert et al. found an improvement in breast satisfaction, psychological well-being, and sexual well-being following BAS [47]. The most effective procedure to improve QoL is inconclusive because of no prior studies comparing QoL after GRS, FFS, and BAS. More studies are needed to provide sufficient evidence in terms of cost-effectiveness and QoL improvement between GRS, FFS, and BAS.
Limitations and suggestions
The limitations of this study include a small sample size that results in less generalizability and feasibility of conducting subgroup analysis of QoL by possible factors that may cause the differences between the two groups. Another limitation was that within-group comparison of QoL during pre- and postoperative was not conducted, which might lead to unidentified differences between pre- and postoperative periods. In addition, our study may contain certain biases due to the nature of the study design. Furthermore, the omission of patient selection details could affect the generalizability of the findings, and the study does not thoroughly investigate postoperative complications, crucial for assessing procedure safety and risk. Further studies on QoL, complications, and cost-effectiveness are suggested to recommend the type of GRS procedure for MTF and GRS in different individuals. In a longitudinal study, the researcher should assess the ability to orgasm, vaginal depth, lubrication, hair removal, postoperative dilation, sexual function, and complications, as this may impact patient perceptions of quality of life.
Conclusions
While requiring more operative steps and resources, male-to-female individuals who undergo sigmoid colon vaginoplasty may achieve a higher quality of life compared to those who undergo penile inversion vaginoplasty. Further studies on the efficacy and other aspects of sigmoid colon vaginoplasty and penile inversion vaginoplasty are needed to compare the two surgical techniques.
References
T W. Group (1998) The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med 46:1569–1585. https://doi.org/10.1016/s0277-9536(98)00009-4
D. American Psychiatric Association and A.P. Association 2013 Diagnostic and statistical manual of mental disorders: DSM-5 American psychiatric association Washington DC
Arcelus J, Bouman WP, Van Den Noortgate W, Claes L, Witcomb G, Fernandez-Aranda F (2015) Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry 30:807–815. https://doi.org/10.1016/j.eurpsy.2015.04.005
Hoenig J, Kenna JC (1974) The prevalence of transsexualism in England and Wales. Br J Psychiatry 124:181–190. https://doi.org/10.1192/bjp.124.2.181
Tsoi WF (1988) The prevalence of transsexualism in Singapore. Acta Psychiatr Scand 78:501–504. https://doi.org/10.1111/j.1600-0447.1988.tb06373.x
Weitze C, Osburg S (1996) Transsexualism in Germany: empirical data on epidemiology and application of the German Transsexuals’ Act during its first ten years. Arch Sex Behav 25:409–425. https://doi.org/10.1007/bf02437583
Vujovic S, Popovic S, Sbutega-Milosevic G, Djordjevic M, Gooren L (2009) Transsexualism in Serbia: a twenty-year follow-up study. J Sex Med 6:1018–1023. https://doi.org/10.1111/j.1743-6109.2008.00799.x
Judge C, O’Donovan C, Callaghan G, Gaoatswe G, O’Shea D (2014) Gender dysphoria - prevalence and co-morbidities in an irish adult population. Front Endocrinol 5:87. https://doi.org/10.3389/fendo.2014.00087
Becerra-Fernández A, Rodríguez-Molina JM, Asenjo-Araque N, Lucio-Pérez MJ, Cuchí-Alfaro M, García-Camba E, Pérez-López G, Menacho-Román M, Berrocal-Sertucha MC, Ly-Pen D, Aguilar-Vilas MV (2017) Prevalence, incidence, and sex ratio of transsexualism in the Autonomous Region of Madrid (Spain) according to healthcare demand. Arch Sex Behav 46:1307–1312. https://doi.org/10.1007/s10508-017-0955-z
Weinforth G, Fakin R, Giovanoli P, Nunez DG (2019) Quality of life following male-to-female sex reassignment surgery. Dtsch Arztebl Int 116:253–260. https://doi.org/10.3238/arztebl.2019.0253
T’Sjoen G, Arcelus J, De Vries ALC, Fisher AD, Nieder TO, Özer M, Motmans J (2020) European Society for Sexual Medicine Position Statement “Assessment and hormonal management in adolescent and adult trans people, with attention for sexual function and satisfaction.” J Sex Med 17:570–584. https://doi.org/10.1016/j.jsxm.2020.01.012
T’Sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V (2019) Endocrinology of transgender medicine. Endocr Rev 40:97–117. https://doi.org/10.1210/er.2018-00011
Tangpricha V, den Heijer M (2017) Oestrogen and anti-androgen therapy for transgender women. Lancet Diabetes Endocrinol 5:291–300. https://doi.org/10.1016/s2213-8587(16)30319-9
Wesp LM, Deutsch MB (2017) Hormonal and surgical treatment options for transgender women and transfeminine spectrum persons. Psychiatr Clin North Am 40:99–111. https://doi.org/10.1016/j.psc.2016.10.006
Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J (2015) Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med 12:1837–1845. https://doi.org/10.1111/jsm.12936
Sinno H, Dionisopoulos T, Slavin SA, Ibrahim AM, Chung KC, Lin SJ (2014) The utility of outcome studies in plastic surgery. Plast Reconstr Surg Glob Open 2:e189. https://doi.org/10.1097/gox.0000000000000104
Cardoso da Silva D, Schwarz K, Fontanari AM, Costa AB, Massuda R, Henriques AA, Salvador J, Silveira E, Elias Rosito T, Lobato MI (2016) WHOQOL-100 before and after sex reassignment surgery in Brazilian male-to-female transsexual individuals. J Sex Med 13:988–993. https://doi.org/10.1016/j.jsxm.2016.03.370
Bouman MB, van der Sluis WB, van Woudenberg Hamstra LE, Buncamper ME, Kreukels BPC, Meijerink W, Mullender MG (2016) Patient-reported esthetic and functional outcomes of primary total laparoscopic intestinal vaginoplasty in transgender women with penoscrotal hypoplasia. J Sex Med 13:1438–1444. https://doi.org/10.1016/j.jsxm.2016.06.009
Lindqvist EK, Sigurjonsson H, Möllermark C, Rinder J, Farnebo F, Lundgren TK (2017) Quality of life improves early after gender reassignment surgery in transgender women. Eur J Plast Surg 40:223–226. https://doi.org/10.1007/s00238-016-1252-0
Papadopulos NA, Lellé JD, Zavlin D, Herschbach P, Henrich G, Kovacs L, Ehrenberger B, Kluger AK, Machens HG, Schaff J (2017) Quality of life and patient satisfaction following male-to-female sex reassignment surgery. J Sex Med 14:721–730. https://doi.org/10.1016/j.jsxm.2017.01.022
Moog D, Latack KR, Adidharma W, Haley C, Satterwhite T, Morrison SD (2021) Getting to the bottom of patient experiences with genital gender affirmation surgery: a qualitative analysis of online reviews. Aesthetic Plast Surg 45:2990–2995. https://doi.org/10.1007/s00266-021-02150-5
Horbach SE, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG (2015) Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med 12:1499–1512. https://doi.org/10.1111/jsm.12868
Bustos SS, Bustos VP, Mascaro A, Ciudad P, Forte AJ, Del Corral G, Manrique OJ (2021) Complications and patient-reported outcomes in transfemale vaginoplasty: an updated systematic review and meta-analysis. Plast Reconstr Surg Glob Open 9:e3510. https://doi.org/10.1097/gox.0000000000003510
Dunford C, Bell K, Rashid T (2021) Genital reconstructive surgery in male to female transgender patients: a systematic review of primary surgical techniques, complication profiles, and functional outcomes from 1950 to present day. Eur Urol Focus 7:464–471. https://doi.org/10.1016/j.euf.2020.01.004
Bizic M, Kojovic V, Duisin D, Stanojevic D, Vujovic S, Milosevic A, Korac G, Djordjevic ML (2014) An overview of neovaginal reconstruction options in male to female transsexuals. Scientific World Journal 2014:638919. https://doi.org/10.1155/2014/638919
Chen ML, Reyblat P, Poh MM, Chi AC (2019) Overview of surgical techniques in gender-affirming genital surgery. Transl Androl Urol 8:191–208. https://doi.org/10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P (2015) Male-to-female vaginoplasty: Preecha’s surgical technique. J Plast Surg Hand Surg 49:153–159. https://doi.org/10.3109/2000656x.2014.967253
Neligan PPC (2017) Plastic surgery-volume 4: trunk and lower extremity. Elsevier-Health Sciences Division
Cuschieri S (2019) The STROBE guidelines. Saudi J Anaesth 13:S31. https://doi.org/10.4103/sja.SJA_543_18
Ware JE Jr (2000) SF-36 health survey update. Spine 25:3130–9. https://doi.org/10.1097/00007632-200012150-00008
Lim LL, Seubsman SA, Sleigh A (2008) Thai SF-36 health survey: tests of data quality, scaling assumptions, reliability and validity in healthy men and women. Health Qual Life Outcomes 6:52. https://doi.org/10.1186/1477-7525-6-52
Ware J, Kosinski MA, Dewey J (2000) How to score version 2 of the SF-36® health survey. Lincoln, QualityMetric Incorporated
Rosner B (2010) Fundamentals of biostatistics. Cengage Learning
Barone M, Cogliandro A, Di Stefano N, Tambone V, Persichetti P (2017) A systematic review of patient-reported outcome measures following transsexual surgery. Aesthetic Plast Surg 41:700–713. https://doi.org/10.1007/s00266-017-0812-4
Pequeno NPF, Cabral NLA, Marchioni DM, Lima S, Lyra CO (2020) Quality of life assessment instruments for adults: a systematic review of population-based studies. Health Qual Life Outcomes 18:208. https://doi.org/10.1186/s12955-020-01347-7
Claes KEY, Pattyn P, D’Arpa S, Robbens C, Monstrey SJ (2018) Male-to-female gender confirmation surgery: intestinal vaginoplasty. Clin Plast Surg 45:351–360. https://doi.org/10.1016/j.cps.2018.03.006
Lawrence AA (2003) Factors associated with satisfaction or regret following male-to-female sex reassignment surgery. Arch Sex Behav 32:299–315. https://doi.org/10.1023/a:1024086814364
Salgado CJ, Nugent A, Kuhn J, Janette M, Bahna H (2018) Primary sigmoid vaginoplasty in transwomen: technique and outcomes. Biomed Res Int 2018:4907208. https://doi.org/10.1155/2018/4907208
Zavlin D, Schaff J, Lellé JD, Jubbal KT, Herschbach P, Henrich G, Ehrenberger B, Kovacs L, Machens HG, Papadopulos NA (2018) Male-to-female sex reassignment surgery using the combined vaginoplasty technique: satisfaction of transgender patients with aesthetic, functional, and sexual outcomes. Aesthetic Plast Surg 42:178–187. https://doi.org/10.1007/s00266-017-1003-z
Buncamper ME, Honselaar JS, Bouman MB, Özer M, Kreukels BP, Mullender MG (2015) Aesthetic and functional outcomes of neovaginoplasty using penile skin in male-to-female transsexuals. J Sex Med 12:1626–1634. https://doi.org/10.1111/jsm.12914
Buncamper ME, van der Sluis WB, van der Pas RSD, Özer M, Smit JM, Witte BI, Bouman MB, Mullender MG (2016) Surgical outcome after penile inversion vaginoplasty: a retrospective study of 475 transgender women. Plast Reconstr Surg 138:999–1007. https://doi.org/10.1097/prs.0000000000002684
Shoureshi P, Dugi D 3rd (2019) Penile inversion vaginoplasty technique. Urol Clin North Am 46:511–525. https://doi.org/10.1016/j.ucl.2019.07.006
Jardim LMMP, Cerentini TM, Lobato MIR, Costa ÂB, Da Silva DC, Schwarz K, Fontanari AMV, Schneider MA, Rosito TE, La Rosa VL (2022) Sexual function, urinary function and quality of life in Brazilian transgender women following Gender-Affirming Surgery. A cross-sectional study. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph192315773
Morrison SD, Vyas KS, Motakef S, Gast KM, Chung MT, Rashidi V, Satterwhite T, Kuzon W, Cederna PS (2016) Facial feminization: systematic review of the literature. Plast Reconstr Surg 137:1759–1770. https://doi.org/10.1097/prs.0000000000002171
Wernick JA, Busa S, Matouk K, Nicholson J, Janssen A (2019) A systematic review of the psychological benefits of gender-affirming surgery. Urol Clin 46:475–486. https://doi.org/10.1016/j.ucl.2019.07.002
Morrison SD, Capitán-Cañadas F, Sánchez-García A, Ludwig DC, Massie JP, Nolan IT, Swanson M, Rodríguez-Conesa M, Friedrich JB, Cederna PS, Bellinga RJ, Simon D, Capitán L, Satterwhite T (2020) Prospective quality-of-life outcomes after facial feminization surgery: an international multicenter study. Plast Reconstr Surg 145:1499–1509. https://doi.org/10.1097/prs.0000000000006837
Javier C, Crimston CR, Barlow FK (2022) Surgical satisfaction and quality of life outcomes reported by transgender men and women at least one year post gender-affirming surgery: a systematic literature review. Int J Transgender Health 23:255–273. https://doi.org/10.1080/26895269.2022.2038334
Acknowledgements
The authors would like to thank the Faculty of Medicine at Chulalongkorn University for their support.
Funding
The authors declare that no funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Study conception and design was performed by Poonpissamai Suwajo. Material preparation and data collection were performed by Weerayut Weerapakorn, Chuthada Chintavalakorn, Piyawat Kantagowit, Threerapat Phitakwongroj, Worapon Ratanalert, Apichai Angspatt, Pornthep Phungrasmi, Seree Iamphongsai, Pasu Promniyom, Nittaya Phanuphak, Chatnapa Yodkitudomying, and Poonpissamai Suwajo. Analysis and first draft of the manuscript were performed by Weerayut Weerapakorn, Chuthada Chintavalakorn, and Piyawat Kantagowit. Study conception and design were performed by authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Chulalongkorn University (Date April 19, 2018/COA No. 351/2018 IRB No. 045/61).
Consent to participate
Informed consent was obtained from all individual participants who participated in the study.
Conflict of interest
Weerayut Weerapakorn, Chuthada Chintavalakorn, Piyawat Kantagowit, Threerapat Phitakwongroj, Worapon Ratanalert, Apichai Angspatt, Pornthep Phungrasmi, Seree Iamphongsai, Pasu Promniyom, Nittaya Phanuphak, Chatnapa Yodkitudomying, and Poonpissamai Suwajo declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 32.4 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weerapakorn, W., Chintavalakorn, C., Kantagowit, P. et al. A single-center cross-sectional study comparison between quality of life after penile inversion and sigmoid colon vaginoplasty in Thailand: a 20-year experience. Eur J Plast Surg 46, 1161–1167 (2023). https://doi.org/10.1007/s00238-023-02140-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02140-7