Abstract
Background
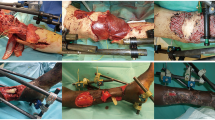
Major extremity trauma forms a considerable proportion of CRI. The aim of this study was to determine whether time to reconstruction and number of debridement’s had an impact on flap success in upper limb CRI.
Methods
A literature search was conducted on Pubmed, Dynamed, DARE, EMBASE, Cochrane, TRIP, Google scholar and BMJ databases. A random effects model was used due to significant heterogeneity between the papers and a meta-regression was implemented for the analysis of outcomes.
Results
Eight articles met the inclusion criteria, covering 65 patients and 74 flaps. Flap success rate was 93% (95% CI: 0.87 – 0.98) with an overall flap complication rate of 10.3% (95% CI 3.4% - 17.2%, p=0.02). Successful flaps had a mean of 8.3 (SD 4.76) pre-flap debridement’s versus 5.7 (SD 2.16) debridement’s in failed flaps.
Conclusions
Soft-tissue reconstruction in CRI often faces complexities due to associated injuries and the risk of infection. Whilst timely reconstruction is important, prioritizing meticulous and often multiple debridement’s over time targets may aid in flap success.
Level of evidence
Level III, Therapeutic.





Similar content being viewed by others
References
Theodorakopoulou E, Mason K, Pafitanis G, Ghanem A, Myers S, Iwuagwu F (2016) Free-tissue transfer for the reconstruction of war-related extremity injuries: a systematic review of current practice. Mil Med 181(1):27–34. https://doi.org/10.7205/MILMED-D-15-00059
Schweizer MA, Janak JC, Graham B, Mazuchowski EL, Gurney JM, Shackelford SA, Stockinger ZT, Monchal T (2019) Nonfatal motor vehicle related injuries among deployed US service members: characteristics, trends, and risks for limb amputations. J Trauma Acute Care Surg 87(4):907-914.7
Akula M, Gella S, Shaw CJ, McShane P, Mohsen AM (2011) A meta-analysis of amputation versus limb salvage in mangled lower limb injuries–the patient perspective. Injury 42(11):1194–1197
Tropf JG, Hoyt BW, Walsh SA, Gibson JA, Polfer EM, Souza JM, Potter BK (2023) Long-term health outcomes of limb salvage compared with amputation for combat-related trauma. Journal of Bone and Joint Surgery. 37733907. https://doi.org/10.2106/JBJS.22.01284
McCulloch I, Valerio I (2021) Lower extremity reconstruction for limb salvage and functional restoration – the combat experience. Clin Plast Surg 48(2):349–361. https://doi.org/10.1016/j.cps.2021.01.005
Wade SM, Harrington CJ, Hoyt BW, Melendez-Munoz AM, Potter BK, Souza JM (2023) Beyond limb salvage: limb restoration efforts following remote combat-related extremity injuries optimize outcomes and support sustained surgical readiness. Mil Med 188(3–4):e584. https://doi.org/10.1093/milmed/usab403
Bhandari PS, Maurya S, Mukherjee MK (2012) Reconstructive challenges in war wounds. Indian J Plast Surg 45:332–339. https://doi.org/10.4103/0970-0358.101316
Yaacoub S, Truppa C, Pedersen TI, Abdo H, Rossi R (2022) Antibiotic resistance among bacteria isolated from war-wounded patients at the Weapon Traumatology Training Center of the International Committee of the Red Cross from 2016 to 2019: a secondary analysis of WHONET surveillance data. BMC Infect Dis 22(1):257. https://doi.org/10.1186/s12879-022-07253-1
Grosset A, Pfister G, de l’ Escalopier N, Plang S, Russo AP, Murison JC, Mathieu L, Rigal S (2019) Risk factors and failures in the management of limb injuries in combat casualties. Int Orthop 43(12):2671–2680. https://doi.org/10.1007/s00264-019-04329-7
Avila-Herrera A, Thissen JB, Mulakken N, Schobel SA, Morrison MD, Zhou X, Grey SF, Lisboa FA, Unselt D, Mabery S, Upadhyay MM, Jaing CJ, Elster EA, Be NA (2022) Metagenomic features of bioburden serve as outcome indicators in combat extremity wounds. Sci Rep 12(1):13816. https://doi.org/10.1038/s41598-022-16170-x
Stewart L, Shaikh F, Bradley W, Lu D, Blyth DM, Petfield JL, Whitman TJ, Krauss M, Greenberg L, Tribble DR (2019) Combat-related extremity wounds: injury factors predicting early onset infections. Mil Med 184(Suppl 1):83–91
Naylor JF, April MD, Thronson EE, Hill GJ, Schauer SG (2020) U.S Military Medical Evacuation and Prehospital Care of Pediatric Trauma Casualties in Iraq and Afghanistan. Prehospital Emerg Care 24(2):265–272. https://doi.org/10.1080/10903127.2019.1626956
Shaw II TW, Chung KK, Wilson RL, April MD, Pamplin JC, Gillespie KR, Salinas J, Schauer SG (2022) An analysis of patient movements during sustained combat operations in the US Central Command: implications for remote support capabilities. Med J Per 73–77
Rozen N, Dudkiewicz I (2011) Wound ballistics and tissue damage in armed conflict injuries to the extremities. Springer. 21–33. https://doi.org/10.1007/978-3-642-16155-1_2.
Yongqiang Z, Dousheng H, Yanning L, Xin M, Kunping W (2020) Peacekeepers suffered combat-related injuries in Mali: a retrospective, descriptive study. BMJ Military Health 166(3):161–166. https://doi.org/10.1136/jramc-2018-001010
Dougherty AL, Mohrle CR, Galaneau MR, Woodruff SI, Duye JL, Quinn KH (2009) Battlefield extremity injuries in operation Iraqi freedom. Injury 40:772–777. https://doi.org/10.1016/j.injury.2009.02.014
Granick M, Boykin J, Gamelli R, Schultz G, Tenenhaus M (2006) Towards a common language: surgical wound bed preparation and debridement. Wound Repair Regeneration 14:1–10. https://doi.org/10.1111/j.1743-6109.2005.00096.x
Guthrie HC, Clasper JC (2011) Historical origins & current concepts of wound debridement. J R Army Med Corps 157:130–132. https://doi.org/10.1136/jramc-157-02-01
British Orthopaedic Association (BOA) (2017) BOAST – open fractures. https://www.boa.ac.uk/resource/boast-4-pdf.html. Accessed 2 Sept 2023
National Institute for Health and Care Research. PROSPERO. International prospective register for systematic reviews. Accessible at https://www.crd.york.ac.uk/prospero/. Accessed 28 Aug 2023
Godina M (1986) Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg 78(3):285–292. https://doi.org/10.1097/00006534-198609000-00001
Kumar AR, Grewal NS, Chung TL, Bradley JP (2009) Lessons from the modern battlefield: successful upper extremity injury reconstruction in the subacute period. J Trauma: Injury, Infect Crit Care 67:752–757. https://doi.org/10.1097/TA.0b013e3181808115
Lo C, Mertz D, Loeb M (2014) Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Medical Research Methodology. 14(1). https://doi.org/10.1186/1471-2288-14-45.
Naalla R, Chauhan S, Dave A, Singhal M (2018) Reconstruction of post-traumatic upper extremity soft tissue defects with pedicled flaps: an algorithmic approach to clinical decision making. Chin J Traumatol 21(6):338–351. https://doi.org/10.1016/j.cjtee.2018.04.005
Tintle SM, Wilson K, McKay PL, Andersen RC, Kumar AR (2010) Simultaneous pedicled flaps for coverage of complex blast injuries to the forearm and hand (with supplemental external fixation to the iliac crest for immobilization). Eur J Hand Surg 35:9–15. https://doi.org/10.1177/1753193409347428
Mathieu L, Gaillard C, Pellet N, Bertani A, Rigal S, Rongiéras F (2014) Soft tissue coverage of war extremity injuries: the use of pedicle flap transfers in a combat support hospital. Int Orthop 38:2175–2181. https://doi.org/10.1007/s00264-014-2398-7
Griffin M, Hindocha S, Malahias M, Saleh M, Juma A (2014) Flap decisions and options in soft tissue coverage of the upper limb. Open Orthop J 31:409–414. https://doi.org/10.2174/1874325001408010409
Payne CE, Hofer SO, Zhong T, Griffin AC, Ferguson PC, Wunder JS (2013) Functional outcome following upper limb soft tissue sarcoma resection with flap reconstruction. J Plast Reconstr Aesthet Surg 66(5):601–607. https://doi.org/10.1016/j.bjps.2013.01.034
Gabrysz-Forget F, Tabet P, Rahal A et al (2019) Free versus pedicled flaps for reconstruction of head and neck cancer defects: a systematic review. J Otolaryngol Head Neck Surg 48:13. https://doi.org/10.1186/s40463-019-0334-y
Tajsic B, Husum H (2008) Reconstructive surgery including free flap transfers can be performed in low-resource settings: experiences from a wartime scenario. J Trauma: Injury, Infect, Crit Care 65(6):1463–1467. https://doi.org/10.1097/TA.0b013e318173f803
Bhullar DS, Karuppiah SV, Aljawadi A, Gillham T, Fakih O, Khamdan K, Pillai A (2019) Local flaps vs. free flaps for complex lower limb fractures: effect of flap choice on patient-reported outcomes. J Orthop Surg Res 12(17):91–96. https://doi.org/10.1016/j.jor.2019.11.016
Berner JE, Ali SR, Will PA, Tejos R, Nanchahal J, Jain A (2023) Standardising the management of open extremity fractures: a scoping review of national guidelines. Eur J Orthop Surg Traumatol 33(5):1463–1471. https://doi.org/10.1007/s00590-022-03324-w
Hughes R (2008) Patient safety and quality: an evidence-based handbook for nurses. Rockville, MD: Agency for Healthcare Research and Quality.
Çeliköz B, Şengezer M, Işik S, Türegün M, Deveci M, Duman H et al (2005) Subacute reconstruction of lower leg and foot defects due to high velocity-high energy injuries caused by gunshots, missiles, and land mines. Microsurgery 25(1):3–15. https://doi.org/10.1002/micr.20049
Duman H, Sengezer M, Celikoz B, Turegun M, Isik S (2001) Lower extremity salvage using a free flap associated with the Ilizarov method in patients with massive combat injuries. Ann Plast Surg 46(2):108–112. https://doi.org/10.1097/00000637-200102000-00003
Orr J, Kirk K, Antunez V, Ficke J (2010) Reverse sural artery flap for reconstruction of blast injuries of the foot and ankle. Foot Ankle Int 31(1):59–64. https://doi.org/10.3113/FAI.2010.0059
Roberts DC, Jose RM, Duraku LS et al (2022) Management of conflict injuries to the upper limb. Part 2: reconstruction and managing complications. J Hand Surg 47(8):787–797
Smith J, Roberts B, Knight A, Gosselin R, Blanchet K (2015) A systematic literature review of the quality of evidence for injury and rehabilitation interventions in humanitarian crises. Int J Public Health 60(7):865–872. https://doi.org/10.1007/s00038-015-0723-6
Tahirkheli M, Ellahi I, Dar M, Sharif A (2016) Distal based sural fascio-cutaneous flap: a practical limb saviour for wounds of war and peace. Journal of College of Physicians and Surgeons Pakistan. 26(5).
Karami R, Ghieh F, Chalhoub R, Saghieh S, Lakkis S, Ibrahim A (2019) Reconstruction of composite leg defects post-war injury. Int Orthop 43(12):2681–2690. https://doi.org/10.1007/s00264-019-04423-w
Burns TC, Stinner DJ, Mack AW, Potter BK, Beer R, Eckel TT, Possley DR, Beltran MJ, Hayda RA, Andersen RC, Keeling JJ, Frisch HM, Murray CK, Wenke JC, Ficke JR, Hsu JR (2012) Skeletal Trauma Research Consortium. Microbiology and injury characteristics in severe open tibia fractures from combat. J Traum Acute Care Surg 72(4):1062–7
Warkentien T, Rodriguez C, Lloyd B, Wells J, Weintrob A, Dunne JR, Ganesan A, Li P, Bradley W, Gaskins LJ, Seillier-Moiseiwitsch F, Murray CK, Millar EV, Keenan B, Paolino K, Fleming M, Hospenthal DR, Wortmann GW, Landrum ML, Kortepeter MG, Tribble DR (2012) Infectious Disease Clinical Research Program Trauma Infectious Disease Outcomes Study Group. Invasive mold infections following combat-related injuries. Clin Infect Dis 55(11):1441–9. https://doi.org/10.1093/cid/cis749
Penn-Barwell JG, Fries CA, SargeantI D, Bennett PM, Porter K (2012) Aggressive soft tissue infections and amputation in military trauma patients. J Royal Navy Med Serv 98:14–18
Sabino J, Slater J, Valerio I (2016) Plastic surgery challenges in war wounded I: flap-based extremity reconstruction. Adv Wound Care 5(9):403–411. https://doi.org/10.1089/wound.2015.0656
Yaremchuk MJ, Brumback RJ, Manson PN, Burgess AR, Poka A, Weiland AJ (1987) Acute and definitive management of traumatic osteocutaneous defects of the lower extremity. Plast Reconstr Surg 80(1):1–14. https://doi.org/10.1097/00006534-198707000-00001
Sheean A, Tintle S, Rhee P (2015) Soft tissue and wound management of blast injuries. Curr Rev Musculoskelet Med 8(3):265–271. https://doi.org/10.1007/s12178-015-9275-x
Ebrahimi A, Nejadsarvari N, Ebrahimi A, Rasouli H (2017) Early reconstructions of complex lower extremity battlefield soft tissue wounds. World Journal of Plastic Surgery. 6(3).
Eccles S, Handley B, Khan U, McFadyen I, Nanchahal J, Nayagam S (2020) Soft tissue reconstruction. Standards for the Management of Open Fractures. 63–74.
Holmgaard R, Duffy J, Warburg FE, Jensen L, Bonde C (2016) Danish experience with free flaps in war wounds. Dan Med J 63:5180–5180
Valerio IL, Sabino J, Bevevino A, Tintle SM, Fleming M, Kumar A (2013) Sequential free tissue transfers for simultaneous upper and lower limb salvage. Microsurgery 33:447–453. https://doi.org/10.1002/micr.22145
Sabino J, Franklin B, Patel K, Bonawitz S, Valerio IL (2013) Revisiting the scapular flap. Plast Reconstruct Surg 132:577–585. https://doi.org/10.1097/PRS.0b013e31829f4a08
Hoyt BW, Wade SM, Harrington CJ, Potter BK, Tintle SM, Souza JM (2021) Institutional experience and orthoplastic collaboration associated with improved flap-based limb salvage outcomes. Clin Orthop Relat Res 479(11):2388–2396. https://doi.org/10.1097/CORR.0000000000001925
Deowall C, Perez-Nieves R, Mckinlay A, Kunasz Markian, Delaney RC, Lyons RH (2007) Operation Iraqi freedom. Ann Plast Surg 58(2):200–206. https://doi.org/10.1097/01.sap.0000237740.08862.85
Casey K, Sabino J, Weiss J, Kumar A, Valerio IL (2015) Limb salvage after vascular reconstruction followed by tissue transfer during the Global War on Terror. J Vasc Surg 61:734–740
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. EW and HE contributed equally to the paper and are joint first authors. EW contributed to the conception/design/literature search and final manuscript writing. HE contributed to the conception/design/literature search/statistical analysis and final manuscript writing. UR contributed to the conception/study design/literature search and final manuscript writing. MK contributed to the conception/study design and final manuscript writing. NC contributed to the conception/study design and final manuscript writing.
Corresponding author
Ethics declarations
Ethical approval
Not required.
Competing interests
Elena Whiteman, Hamza Ejaz, Umar Rehman, Manaf Khatib, and Naveen Cavale declare no conflict of interest.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Whiteman, E., Ejaz, H., Rehman, U. et al. Soft tissue reconstruction of combat-related injuries in the upper limb—should serial debridement’s be prioritised over time to reconstruction? A systematic review and meta-analysis. Eur J Plast Surg 46, 887–900 (2023). https://doi.org/10.1007/s00238-023-02136-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02136-3