Abstract
Background
Major extremity trauma forms a considerable proportion of combat-related injuries. Coverage of lower limb soft tissue defects utilises the reconstructive ladder. The 72-h target to definitive reconstruction has been proposed in civilian trauma. The primary aim of this study was to determine whether the time to definitive reconstruction and the number of pre-flap debridements have an impact on flap success in lower limb combat injury reconstructions.
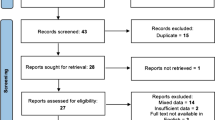
Methods
A literature search was conducted on Pubmed, Prospero, Dynamed, DARE, EMBASE, COCHRANE and BMJ databases. A random effects model was used due to significant heterogeneity between the papers and a meta-regression was implemented for the analysis of outcomes.
Results
A total of seven studies had fulfilled the inclusion criteria. The cumulative number of flaps performed was 378 (255 free flaps and 123 non-free flaps). The Latissimus Dorsi free flap was the most common flap performed (n = 153). The proportion of flap success across the studies was 88% (0.88, 95% CI: 0.77–0.94). There was no statistically significant impact of the number of pre-flap debridements on flap success rates (OR of: 1.23 [95% CI: 0.62 to 2.44], p > 0.05). Time to reconstruction had no statistically significant impact on flap success rates (OR of: 0.88 [95% CI: 0.77 to 1.00], p > 0.05).
Conclusions
The choice of flap used in lower limb combat-related injuries is dependent upon the type, extent and location of injury. Onus should be placed on ensuring the wound is adequately debrided prior to definitive coverage to provide a healthy wound bed for reconstruction.
Level of Evidence: Not gradable









Similar content being viewed by others
Abbreviations
- AHRQ:
-
The Agency for Healthcare Research and Quality
- ALT:
-
Anterolateral thigh
- CRI:
-
Combat-related injuries
- ETFL:
-
Extensor tensor fascia latae
- ICRC:
-
International Committee of the Red Cross
- LD:
-
Latissimus dorsi
- LL:
-
Lower limb
- RA:
-
Rectus abdominis
References
Theodorakopoulou E, Mason K, Pafitanis G, Ghanem A, Myers S, Iwuagwu F (2016) Free-tissue transfer for the reconstruction of war-related extremity injuries: a systematic review of current practice. Mil Med 181(1):27–34
Geiger S, McCormick F, Chou R, Wandel A (2008) War wounds: lessons learned from Operation Iraqi Freedom. Plast Reconstr Surg 122(1):146–153
Mathieu L, Plang S, de l’Escalopier N, Murison J, Gaillard C, Bertani A et al (2020) Soft tissue coverage using pedicled flap in combat zone: a case series. Military Medical Research. 7(1)
Kazmirchuk A, Yarmoliuk Y, Kazmirchuk A, Yarmoliuk Y, Lurin I, Gybalo R, Burianov O, Derkach S, Karpenko K (2022) Ukraine’s experience with management of combat casualties using NATO’s four-tier “changing as needed” healthcare system. World J Surg 46(12):2858–2862
Schweizer MA, Janak JC, Graham B, Mazuchowski EL, Gurney JM, Shackelford SA, Stockinger ZT, Monchal T (2019) Nonfatal motor vehicle related injuries among deployed US service members: characteristics, trends, and risks for limb amputations. J Trauma Acute Care Surg 87(4):907–914
Tintle SM, Forsberg JA, Keeling JJ, Shawen SB, Potter BK (2010) Lower extremity combat-related amputations. J Surg Orthop Adv 19(1):35–43
Tintle SM, Shawen SB, Forsberg JA, Gajewski DA, Keeling JJ, Andersen RC, Potter BK (2014) Reoperation after combat-related major lower extremity amputations. J Orthop Trauma 28(4):232–237
Stewart L, Shaikh F, Bradley W, Lu D, Blyth DM, Petfield JL, Whitman TJ, Krauss M, Greenberg L, Tribble DR (2019) Combat-related extremity wounds: injury factors predicting early onset infections. Mil Med 184(Suppl 1):83–91
Huh J, Stinner DJ, Burns TC, Hsu JR, Late Amputation Study Team (2011) Infectious complications and soft tissue injury contribute to late amputation after severe lower extremity trauma. J Trauma. 71(1 Suppl):47–51
Akula M, Gella S, Shaw CJ, McShane P, Mohsen AM (2011) A meta-analysis of amputation versus limb salvage in mangled lower limb injuries–the patient perspective. Injury 42(11):1194–1197
Giancnou C, Baldan M (2010) War surgery: working with limited resources in armed conflict and other situations of violence, vol 1. ICRC, Geneva
Sheean A, Tintle S, Rhee P (2015) Soft tissue and wound management of blast injuries. Curr Rev Musculoskelet Med 8(3):265–271
Sabino J, Franklin B, Patel K, Bonawitz S, Valerio I (2013) Revisiting the scapular flap. Plast Reconstr Surg 132(4):577e–585e
Eccles S, Handley B, Khan U, McFadyen I, Nanchahal J, Nayagam S (2020) Soft tissue reconstruction. Standards Manage Open Fract 63–74
Sabino J, Slater J, Valerio I (2016) Plastic surgery challenges in war wounded I: flap-based extremity reconstruction. Adv Wound Care 5(9):403–411
Richards A, Dafydd H, Wei F (2015) Key notes on plastic surgery. 2nd ed. John Wiley and Sons
Tajsic N, Husum H (2008) Reconstructive surgery including free flap transfers can be performed in low-resource settings: experiences from a wartime scenario. J Trauma: Injury, Infect Critical Care 65(6):1463–1467
Khundkar R (2019) Lower extremity flap coverage following trauma. J Clin Orthopaedics Trauma 10(5):839–844
Jordan D, Malahias M, Hindocha S, Juma A (2014) Flap decisions and options in soft tissue coverage of the lower limb. Open Orthopaedics J 8(1):423–432
Godina M (1986) Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg 78(3):285–292
Liu D, Sofiadellis F, Ashton M, MacGill K, Webb A (2012) Early soft tissue coverage and negative pressure wound therapy optimises patient outcomes in lower limb trauma. Injury 43(6):772–778
Qiu E, Kurlander D, Ghaznavi A (2018) Godina revisited: a systematic review of traumatic lower extremity wound reconstruction timing. J Plast Surg Hand Surg 52(5):259–264
Lee Z, Stranix J, Rifkin W, Daar D, Anzai L, Ceradini D et al (2019) Timing of microsurgical reconstruction in lower extremity trauma. Plast Reconstr Surg 144(3):759–767
Rivera J, Wenke J, Pugh M (2016) Open fracture care during war. J Bone Joint Surg Rev. 4(10)
Kumar A, Grewal N, Chung T, Bradley J (2009) Lessons from Operation Iraqi Freedom: successful subacute reconstruction of complex lower extremity battle injuries. Plast Reconstr Surg 123(1):218–229
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M et al (2022) Cochrane handbook for systematic reviews of interventions Version 6.3. The Cochrane Collaboration
Lo C, Mertz D, Loeb M (2014) Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 14(1)
Hughes R (2008) Patient safety and quality: an evidence-based handbook for nurses. Rockville, MD: Agency for Healthcare Res Qual
Duman H, Sengezer M, Celikoz B, Turegun M, Isik S (2001) Lower extremity salvage using a free flap associated with the ilizarov method in patients with massive combat injuries. Ann Plast Surg 46(2):108–112
Çeliköz B, Şengezer M, Işik S, Türegün M, Deveci M, Duman H et al (2005) Subacute reconstruction of lower leg and foot defects due to high velocity-high energy injuries caused by gunshots, missiles, and land mines. Microsurgery 25(1):3–15
Orr J, Kirk K, Antunez V, Ficke J (2010) Reverse sural artery flap for reconstruction of blast injuries of the foot and ankle. Foot Ankle Int 31(1):59–64
Tahirkheli M, Ellahi I, Dar M, Sharif A (2016) Distal based sural fascio-cutaneous flap: a practical limb saviour for wounds of war and peace. J College Phys Surg Pakistan. 26(5)
Ebrahimi A, Nejadsarvari N, Ebrahimi A, Rasouli H (2017) Early Reconstructions of complex lower extremity battlefield soft tissue wounds. Would J Plastic Surg. 6(3)
Karami R, Ghieh F, Chalhoub R, Saghieh S, Lakkis S, Ibrahim A (2019) Reconstruction of composite leg defects post-war injury. Int Orthop 43(12):2681–2690
Hacquebord J, Hanel D, Friedrich J (2017) The pedicled latissimus dorsi flap provides effective coverage for large and complex soft tissue injuries around the elbow. Hand 13(5):586–592
Reath D, Taylor J (1989) Free rectus abdominis muscle flap: advantages in lower extremity reconstruction. South Med J 82(9):1143–1146
Burns T, Stinner D, Possley D, Mack A, Eckel T, Potter B et al (2010) Does the zone of injury in combat-related type III open tibia fractures preclude the use of local soft tissue coverage? J Orthop Trauma 24(11):697–703
Tintle S, Gwinn D, Andersen R, Kumar A (2010) Soft tissue coverage of combat wounds. J Surg Orthop Adv 19(1):29–34
Georgiadis G, Behrens F, Joyce M, Earle A, Simmons A (1993) Open tibial fractures with severe soft-tissue loss Limb salvage compared with below-the-knee amputation. J Bone Joint Surg 75(10):1431–1441
Small J, Mollan R (1992) Management of the soft tissues in open tibial fractures. Br J Plast Surg 45(8):571–577
Sabino J, Polfer E, Tintle S, Jessie E, Fleming M, Martin B et al (2015) A decade of conflict: flap coverage options and outcomes in traumatic war-related extremity reconstruction. Plast Reconstr Surg 135(3):895–902
Valerio I, Sabino J, Mundinger G, Kumar A (2014) From battleside to stateside. Ann Plast Surg 72:S38–S45
Higgins T, Klatt J, Beals T (2010) Lower Extremity Assessment Project (LEAP) – the best available evidence on limb-threatening lower extremity trauma. Orthop Clin North Am 41(2):233–239
Klem C, Sniezek J, Moore B, Davis M, Coppit G, Schmalbach C (2013) Microvascular reconstructive surgery in Operations Iraqi and Enduring Freedom. J Trauma Acute Care Surg 75(2):S228–S232
Connolly M, Ibrahim Z, Johnson O (2016) Changing paradigms in lower extremity reconstruction in war-related injuries. Military Med Res. 3(1)
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Not required.
Conflict of interest
Umar Rehman, Elaine Cole, Elena Whiteman, Manaf Khatib, Naveen Cavale and Christos Giannou declare no competing interests.
Patient consent
Not applicable.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rehman, U., Cole, E., Whiteman, E. et al. Soft tissue reconstruction of combat-related injuries affecting the lower limb: is a time target realistic? A systematic review and meta-analysis. Eur J Plast Surg 46, 935–946 (2023). https://doi.org/10.1007/s00238-023-02095-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02095-9