Abstract
Background
Cranial reconstruction is a challenging procedure. The procedure aims to restore the aesthetic and function of the normal skull bone. There have been several materials ascribed to the reconstruction of the cranial vault. Among these materials is polyetheretherketon (PEEK), which is a superior biomedical polymer.
Methods
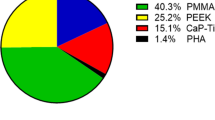
A retrospective review of all PEEK cranioplasties that were conducted in Khoula Hospital between 2017 and 2021 was performed. Fourteen patients were included in this study. Data collection included the demographics, the characteristics of the cranial defect, and the post-operative complications.
Results
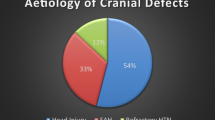
Majority of the cases had a cranial defect secondary to decompressive craniectomy 78.5% (n = 11). These defects had an average size of 12 × 10 cm. There were immediate postoperative complications reported. However, 4 cases had seroma collection upon follow-up that required aspiration. In terms of the aesthetic outcome, 2 cases had temporal hollowing.
Conclusion
PEEK serves as an outstanding material for cranial reconstruction. It is associated with a relatively low complication rate. However, the design of the implant should be modified to achieve a superior aesthetic outcome and reduce temporal depression.
Level of evidence: Level IV, Therapeutic.



Similar content being viewed by others
Data availability
The data that were generated at Khoula hospital for this study are available with the corresponding author, Khalifa Al Alawi, upon reasonable request.
References
Aydin S, Kucukyuruk B, Abuzayed B, Aydin S, Sanus GZ (2011) Cranioplasty: review of materials and techniques. J Neurosci Rural Pract 2(2):162. Available from: /pmc/articles/PMC3159354/. Accessed 15 Jan 2022
Arun Kumar KV, Singla NK, Gowda ME, Kumar D, Legha VS (2014) Current concepts in restoring acquired cranial defects. J Indian Prosthodont Soc 14(Suppl 1):14. Available from: /pmc/articles/PMC4501989/. Accessed 15 Jan 2022
Iaccarino C, Kolias AG, Roumy LG, Fountas K, Adeleye AO (2019) Cranioplasty following decompressive craniectomy. Front Neurol 10:1357. Available from: /pmc/articles/PMC7000464/. Accessed 15 Jan 2022
Shah AM, Jung H, Skirboll S (2014) Materials used in cranioplasty: a history and analysis. Neurosurg Focus 36(4):E19. Available from: https://thejns.org/focus/view/journals/neurosurg-focus/36/4/article-pE19.xml. Accessed 26 Sept 2022
Liu L, Lu ST, Liu AH, Hou WB, Cao WR, Zhou C et al (2020) Comparison of complications in cranioplasty with various materials: a systematic review and meta-analysis. [Internet]. [cited 2022 Sep 26];34(4):388–96. Available from: https://www.tandfonline.com/doi/abs/https://doi.org/10.1080/02688697.2020.1742291
Brichacek M, Antonyshyn O, Edwards G, Mainprize JG, da Costa L (2021) Decision-making in adult cranial vault reconstruction. Plast Reconstr Surg 148(1):109E–121E. Available from: https://pubmed.ncbi.nlm.nih.gov/34181619/. Accessed 27 Sep 2022
Sanan A, Haines SJ (1997) Repairing holes in the head: a history of cranioplasty. Neurosurgery 40(3):588–603. Available from: https://pubmed.ncbi.nlm.nih.gov/9055300/. Accessed 4 Oct 2022
Alkhaibary A, Alharbi A, Alnefaie N, Aloraidi A, Khairy S (2020) Cranioplasty: a comprehensive review of the history, materials, surgical aspects, and complications. World Neurosurg 1(139):445–452
Piitulainen JM, Kauko T, Aitasalo KMJ, Vuorinen V, Vallittu PK, Posti JP (2015) Outcomes of cranioplasty with synthetic materials and autologous bone grafts. World Neurosurg 83(5):708–714
Arun Kumar KV, Singla NK, Gowda ME, Kumar D, Legha VS (2014) Current concepts in restoring acquired cranial defects. The Journal of the Indian Prosthodontic Society 14(Suppl 1):14. Available from: /pmc/articles/PMC4501989/. Accessed 15 Jan 2022
Malcolm JG, Mahmooth Z, Rindler RS, Allen JW, Grossberg JA, Pradilla G et al (2018) Autologous cranioplasty is associated with increased reoperation rate: a systematic review and meta-analysis. World Neurosurg 1(116):60–68
Clinical outcome in cranioplasty: critical review in long-term follow-up. J Craniofac Surg. Available from: https://journals.lww.com/jcraniofacialsurgery/Abstract/2003/03000/Clinical_Outcome_in_Cranioplasty__Critical_Review.3.aspx. Accessed 29 Sept 2022
Park EK, Lim JY, Yun IS, Kim JS, Woo SH, Kim DS et al (2016) Cranioplasty enhanced by three-dimensional printing: custom-made three-dimensional-printed titanium implants for skull defects. J Craniofac Surg 27(4):943–949. Available from: https://journals.lww.com/jcraniofacialsurgery/Fulltext/2016/06000/Cranioplasty_Enhanced_by_Three_Dimensional.27.aspx. Accessed 29 Sept 2022
Zhu S, Chen Y, Lin F, Chen Z, Jiang X, Zhang J et al (2021) Complications following titanium cranioplasty compared with nontitanium implants cranioplasty: a systematic review and meta-analysis. J Clin Neurosci 1(84):66–74
Kurtz SM (2019) PEEK biomaterials handbook — Google Books. Available from: https://books.google.com.om/books?hl=en&lr=&id=SimLDwAAQBAJ&oi=fnd&pg=PP1&dq=peek+for+medical+implant+history+&ots=hutGYSjQOP&sig=a65jXdWxB63sYjaEPQWBJp3OwY4&redir_esc=y#v=onepage&q=peek%20for%20medical%20implant%20history&f=false. Accessed 30 Sept 2022
Punchak M, Chung LK, Lagman C, Bui TT, Lazareff J, Rezzadeh K et al (2017) Outcomes following polyetheretherketone (PEEK) cranioplasty: systematic review and meta-analysis. J Clin Neurosci 41:30–35. Available from: http://www.jocn-journal.com/article/S0967586816315375/fulltext. Accessed 30 Sept 2022
Brandicourt P, Delanoé F, Roux FE, Jalbert F, Brauge D, Lauwers F (2017) Reconstruction of cranial vault defect with polyetheretherketone implants. World Neurosurg 1(105):783–789
Thien A, King NKK, Ang BT, Wang E, Ng I (2015) Comparison of polyetheretherketone and titanium cranioplasty after decompressive craniectomy. World Neurosurg 83(2):176–180
Andrabi S, Sarmast A, Kirmani A, Bhat A (2017) Cranioplasty: indications, procedures, and outcome — an institutional experience. Surg Neurol Int 8(1). Available from: /pmc/articles/PMC5461575/. Accessed 30 Sept 2022
Mee H, Anwar F, Timofeev I, Owens N, Grieve K, Whiting G et al (2022) Cranioplasty: a multidisciplinary approach. Front Surg 17(9):531
Makiuchi Y, Ozaki M, Iwashina Y, Oshima N, Akagi K (2022) Tissue expander repositioning for wound dehiscence in scalp expanded prior to cranioplasty case report. Int J Surg Wound Care 3(2):50–54
Rubio EJ dos S, Bos EM, Dammers R, Koudstaal MJ, Dumans AG (2016) Two-stage cranioplasty: tissue expansion directly over the craniectomy defect prior to cranioplasty. Craniomaxillofac Trauma Reconstr 9(4):355. Available from: /pmc/articles/PMC5101123/. Accessed 19 Oct 2022
Carloni R, Hersant B, Bosc R, le Guerinel C, Meningaud JP (2015) Soft tissue expansion and cranioplasty: For which indications? J Cranio-Maxillofac Surg 43(8):1409–1415
Punchak M, Chung LK, Lagman C, Bui TT, Lazareff J, Rezzadeh K et al (2017) Outcomes following polyetheretherketone (PEEK) cranioplasty: systematic review and meta-analysis. J Clin Neurosci 41:30–35. Available from: https://pubmed.ncbi.nlm.nih.gov/28377284/. Accessed 19 Oct 2022
Amendola F, Vaienti L, Carbonaro R, Nataloni A, Barbanera A, Zingaretti N et al (2022) The antibiotic immersion of custom-made porous hydroxyapatite cranioplasty: a multicentric cohort study. J Craniofac Surg 33(5):1464–1468. Available from: https://journals.lww.com/jcraniofacialsurgery/Fulltext/2022/07000/The_Antibiotic_Immersion_of_Custom_Made_Porous.46.aspx. Accessed 26 Oct 2022
Frassanito P, Fraschetti F, Bianchi F, Giovannenze F, Caldarelli M, Scoppettuolo G (2019) Management and prevention of cranioplasty infections. Child’s Nervous System 35(9):1499–506. Available from: https://doi.org/10.1007/s00381-019-04251-8. Accessed 26 Oct 2022
Paredes I, Lagares A, San-Juan R, Castaño-León AM, Gómez PA, Jimenez-Roldán L et al (2020) Reduction in the infection rate of cranioplasty with a tailored antibiotic prophylaxis: a nonrandomized study. Acta Neurochir 162(11):2857–66. Available from: https://doi.org/10.1007/s00701-020-04508-1. Accessed 26 Oct 2022
Wolff A, Santiago GF, Belzberg M, Huggins C, Lim M, Weingart J et al (2018) Adult cranioplasty reconstruction with customized cranial implants: preferred technique, timing, and biomaterials. J Craniofac Surg 29(4):887–894. Available from: https://journals.lww.com/jcraniofacialsurgery/Fulltext/2018/06000/Adult_Cranioplasty_Reconstruction_With_Customized.19.aspx. Accessed 26 Oct 2022
Funding
The author(s) received no financial support for the research, author- ship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Khoula Hospital Ethical Board (REC 09/2022). This study was conducted in accordance with the Declaration of Helsinki.
Patient Consent
Patients have signed a written consent to share their data and use their photos in the manuscript.
Conflict of interest
Khalifa Al Alawi, Sultan Al Shaqsi, Moath Shummo, Mohudoom Meera Sahib, and Taimoor Al Balushi declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al Alawi , K., Al Shaqsi, S., Shummo, M. et al. Cranial reconstruction with polyetheretherketone patient-specific implant: a single-center experience. Eur J Plast Surg 46, 953–959 (2023). https://doi.org/10.1007/s00238-023-02083-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02083-z