Abstract
Background
Abdominoperineal resection in patients with anorectal malignancies may require flap reconstruction for large perineal defects as an adjunct to the oncologic surgery. Perineal reconstruction should be timely, safe, and yield good long-term functional results. There is no agreement on the ideal approach.
Methods
We performed a retrospective observational cohort study to compare clinical outcomes and post-operative complications between a musculocutaneous gluteal flap and a fasciocutaneous V–Y flap for perineal reconstruction. We included all patients who underwent abdominoperineal resection at Karolinska University Hospital between 2016 and 2019. Patient demographics and comorbidities, as well as treatment data, post-operative complications, and follow-up data, were collected from medical records.
Results
A total of 44 patients were included with a mean age of 65 years where 73% were men. Reconstruction was made with a musculocutaneous gluteal flap in 19 patients (43%) and with a fasciocutaneous V–Y flap in 25 patients (57%). Flap-related post-operative complications occurred in 39% of the patients and the incidence did not differ between the groups (p = 0.831). Neither operative time, time to ambulant mobility, time to drain removal, nor time to epidural removal differed between the groups (p > 0.05). Four patients in the gluteal flap group and one patient in the V–Y flap group presented with long-term complications.
Conclusions
Post-operative complications are common after perineal reconstruction following abdominoperineal resection regardless of reconstructive approach. Our study confirms that both a fasciocutaneous and a musculocutaneous flap are acceptable options for perineal reconstruction.
Level of evidence: Level III, risk/prognostic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abdominoperineal resection has been the gold standard surgery for many anorectal malignancies since its description in 1908 [1]. Perineal reconstruction with plastic surgery techniques is an important adjunct to oncologic surgery and allows for more aggressive tumor resection [2]. It is commonly agreed that successful perineal reconstruction is achieved through the elimination of perineal dead space, obliteration of the defect with healthy, well-vascularized tissue, and a tension-free closure. In patients undergoing abdominoperineal resection, perineal reconstruction with a myocutaneous flap yields better local outcomes compared to primary cutaneous closure [3,4,5]. There are several flap-based perineal reconstruction techniques, broadly divided into abdominal-based (such as rectus abdominis), thigh-based (such as gracilis or anterolateral thigh), and perineal-based (such as gluteal) approaches, none of which has been proven to have superior outcomes [6, 7].
In our institution, we have used a perineal-based approach, namely the myocutaneous gluteal flap, for reconstruction of medium-sized perineal defects for almost two decades, whereas for the reconstruction of large perineal defects, we use a vertical rectus abdominis muscle (VRAM) flap [2]. The VRAM flap is a well-established method for perineal reconstruction and allows plenty of bulk for the elimination of perineal dead space as well as tension-free closure; however, it carries a 15–17% risk of donor-site morbidity, and the pedicled design brings a 23–27% risk of perineal flap morbidity, and the risk of complete flap loss is small (2%) but present [8,9,10].
Our rationale behind using the myocutaneous gluteal flap reconstruction technique in medium-sized defects are its advantages of prone positioning of the patient, and lower donor-site morbidity compared to the VRAM flap, whereas the disadvantage is a higher risk of prolonged perineal healing and possibly a greater risk of long-term complications including perineal hernias due to poorer elimination of perineal dead space [11, 12]. The higher risk of perineal wound dehiscence may or may not be related to the increased frequency of neoadjuvant radiotherapy in this patient group. With the myocutaneous gluteal flap reconstruction technique, perineal post-operative morbidity affects 42% of patients [2, 11].
In the last few years, another perineal-based approach, the fasciocutaneous V–Y flap, has been described by several teams as a timely, safe, and efficient reconstructive approach for perineal defects [13,14,15,16]. Similar to the myocutaneous gluteal flap, the V–Y fasciocutaneous flap allows for prone positioning of the patient, and avoids morbidity of the abdominal wall, but has the additional advantage of being muscle-sparing. Patients undergoing gluteal flap–based reconstructive breast surgery have reported gait and ambulation problems both during the early and in the late post-operative period [17]. Post-operative mobilization is often limited by pain and tightness following the muscle flap reconstruction, further contributing to a long post-operative rehabilitation and potentially additional complications. In comparison to the myocutaneous gluteal flap, the V–Y flap could thus be hypothesized to offer a quicker dissection and flap mobilization, fewer post-operative complications, and an easier post-operative rehabilitation.
The potential disadvantage with the thinner fasciocutaneous V–Y flap, on the other hand, could be an increased risk of long-term perineal complications such as hernias. To our knowledge, no prospective or retrospective study has compared the myocutaneous flap with the fasciocutaneous option for perineal reconstruction after abdominoperineal oncologic resection.
In our unit, as of December 2018, patients who after abdominoperineal resection have pelvic floor defects too large for primary muscle closure, as jointly assessed by the colorectal and reconstructive plastic surgeons, are reconstructed with a V–Y fasciocutaneous flap [2]. We compare clinical outcomes and post-operative complications between the previously employed myocutaneous gluteal flap and the recently implemented fasciocutaneous V–Y flap for perineal reconstruction.
Materials and methods
We performed a retrospective observational cohort study of all patients who underwent abdominoperineal resection and perineal reconstruction with a unilateral perineal-based flap at Karolinska University Hospital between 1st January 2016 and 31st December 2019.
This study was performed in line with the principles of the Declaration of Helsinki. The Swedish Ethical Review Authority approved the study (reference number 2019–04636) and confirmed that no written consent was required for this observational study. The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1A–D and 2A–D.
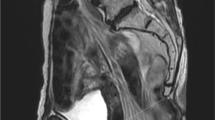
Patients were identified through a search in the electronic medical records for referrals between the colorectal unit and the reconstructive plastic surgery unit, since such a referral is the formal way of enlisting reconstructive competency in anticipation of an extended abdominoperineal resection. The choice of reconstructive method was at the discretion of the plastic surgeon and consisted of either a gluteal musculocutaneous flap (mainly 2016–2017) or a V–Y fasciocutaneous flap (mainly 2018–2019). For a typical size defect, please see Fig. 1A (Supplemental Online Material).
Patient demographics and comorbidities, indication for surgery, treatment data, and post-operative outcomes were all collected from electronic medical records. Patient data included sex, age, smoking habits, BMI, pre-operative serum albumin levels, and comorbidities such as diabetes, and ASA classification (American Society of Anesthesiologists Physical Status). Treatment data included tumor type, the use of neoadjuvant radiotherapy, and surgical approach. Data on reconstructive procedure duration, through the operating room electronic medical record, and tumor size, as stated by the pathology report, was also collected.
All post-operative complications were recorded. There were divided into any wound dehiscence, bleeding from the surgical site, local or systemic infection, partial or full flap necrosis, take-back to theater for flap-related reasons, re-admittance after discharge for flap-related complications, and perineal hernias. Complications were categorized as short-term (within 30 days of surgery) or long-term complications. Complications were further divided into systemic and local (flap or perineal) complications, the latter category including wound dehiscence, perineal surgical site infection, and flap necrosis. Systemic infections considered to have originated in perineal infections were classified as local, flap-related complications, whereas systemic infections without known source were classified as systemic complications. Post-operative rehabilitation factors recorded were time to ambulant mobility, defined as walking at least 10 m without human support as per the physiotherapists’ records, time to removal of perineal wound drains, time to removal of epidural pain catheter, and time to discharge from the university hospital to either the patient’s home, a rehabilitative unit, or a regional hospital. Patients were followed for as long as medical records were available, or until end-of-follow-up in September 2020.
Exclusion criteria were reconstruction with bilateral flaps instead of unilateral flaps, and concurrent vaginal reconstruction through an additional or extended flap. A STROBE checklist is supplied as supplementary material.
Surgical methods
All flaps were raised at the end of the abdominoperineal resection with the patient in a prone position. The gluteal musculocutaneous flap was marked on the skin as a cranially based rotational flap in a manner that has been described previously (Fig. 1, Supplemental Online Material) [2, 11]. The skin, the subcutaneous tissue, and the gluteus maximus fascia were incised all along the wound, after which one-third to half of the gluteus maximus muscle was divided from its medial border laterally. The medial border of the contralateral gluteus maximus muscle was identified. The musculocutaneous flap was raised until it reached the contralateral muscle without tension. The flap was sutured in four layers with interrupted sutures in the muscle, followed by interrupted or uninterrupted sutures in both the Scarpa’s fascia and the deep dermis, and finally interrupted non-absorbable sutures in the skin.
The fasciocutaneous flap was marked on the skin as a laterally based V–Y flap (Fig. 2, Supplemental Online Material). The skin, the subcutaneous tissue, and the gluteus maximus fascia were incised to provide mobility, followed by de-epithelization of 4–5 cm of the medial border. The de-epithelized tissue was sutured to the levator ani muscle if not resected in the abdominoperineal resection, otherwise and most often to the contralateral border of the gluteus maximus muscle. The flap was sutured in four layers with interrupted sutures between the de-epithelized tissue and the muscle, followed by interrupted or uninterrupted sutures in both the Scarpa’s fascia and the deep dermis, and finally interrupted non-absorbable sutures in the skin.
Post-operative regimen
The post-operative protocol was constructed in collaboration with colorectal surgeons and physiotherapists, and printed versions were available on the ward. The post-operative regimen for both surgical techniques included care in an air-fluidized therapy bed until discharge, avoidance of on-the-side positioning on the flap-side until the second post-operative day, two active wound drains, and removal of sutures at 21 days post-operatively. Drains were removed when producing less than 50 ml per drain per day, and at the earliest 24 h after removal of the abdominal or pelvic drains placed by the colorectal surgeons. Epidural catheters were used in all patients and were post-operatively gradually replaced with oral pain medication as needed. For both techniques, careful, step-wise mobilization of the patient was guided by physiotherapists, and sitting with 90° hip flexion was not allowed until 15 days post-operatively and then only for 30 min at a time. Step-wise mobilization was guided by patient pain and capacity, and ambulant mobility, initially with the help of human support or a walking frame, was encouraged to take place as early as possible. For patients operated with the gluteal musculocutaneous flap, hip flexion was kept below 45° until post-operative day 8, whereas for patients operated with the fasciocutaneous flap, hip flexion up to 60° was allowed from the first post-operative day, and the technique for physiotherapist-supported uprising from bed to standing position was adjusted accordingly.
Statistical analysis
Patient characteristics, management details, and outcomes were described using frequencies (in per cent), means, and ranges. Differences in post-operative outcomes were analyzed by type of reconstructive surgery. The Fisher exact test was used for categorical variables whilst the Mann–Whitney U test was employed for continuous variable analysis. Statistical analysis was carried out using Stata version 13.1. A p-value ≤ 0.05 was considered statistically significant.
Results
We identified 54 patients who had undergone abdominoperineal resection with perineal flap reconstruction during the study time. Ten patients were excluded on the basis of having had a bilateral flap reconstruction (five patients) or having had a concurrent vaginal reconstruction (five patients).
In total, 44 patients were included in our analysis (Table 1). A majority (32 patients, 72.7%) of the cohort were men. The mean age at surgery was 65.3 years (range 42–78 years). Two-third of patients (29 patients, 65.9%) had never been smokers, and diabetes was uncommon (8 patients, 18.2%). Mean BMI in the cohort was 26.0, and 20 patients (45.5%) had a low serum albumin, defined as below 33 g/L. A majority of patients (40 patients, 91%) were classified pre-operatively as ASA II or III. The indication for surgery was a locally advanced rectal malignancy resected with extralevator abdominoperineal excision (ELAPE) in 39 patients, a locally advanced anal cancer in three patients, and other (inflammatory bowel disease and suspected but not confirmed malignancy) in two patients. Seventeen patients (38.6%) were treated for a recurrent cancer, and thus underwent abdominoperineal resection for their second time. Most patients (90.9%) had previous radiotherapy.
The mean age was lower (63 years vs 67 years), and the mean BMI was higher (27 versus 25) in the cohort reconstructed with a musculocutaneous flap, but the differences were not statistically significant (p = 0.193, p = 0.169). The indication for surgery was rectal cancer in 78.9% of the cohort reconstructed with a musculocutaneous flap and 96.0% in the cohort reconstructed with a fasciocutaneous flap. All other patient characteristics were similar between the cohorts.
The mean duration of the perineal reconstruction was 116 min in the entire cohort (range 62–165 min, standard deviation (SD) 31). The mean duration of the fasciocutaneous V–Y flap reconstruction was slightly longer, 125 min, compared to the musculocutaneous flap reconstruction, 108 min, but the difference was not statistically significant (p = 0.105). Flap drains were kept for 8 days post-operatively on average (range 2–18 days, SD 3) and the epidural catheter for 7 days (range 4–13 days, SD 2). Patients were ambulant after 6 days on average (range 2–16 days, SD 3), and discharged from the hospital after a mean inpatient time of 13 days (range 5–37 days, SD 7). There was no difference between the two groups in time to drain removal, time to epidural removal, time to ambulant mobility, or inpatient time.
The incidence of any post-operative complication within 30 days was 70.5% in the entire cohort (Table 2). The incidence of flap-related complications was 38.6% in the cohort (Tables 2 and 3). Six patients (13.4%) required take-back to theater for flap-related reasons, four in the musculocutaneous flap group and two in the fasciocutaneous V–Y flap group. There was no difference in incidence of all complications (p = 0.797), in flap-related complications (p = 0.831), or in specific complications between the groups.
Ten patients in the cohort (22.7%) had complications that persisted after 30 days or occurred after 30 days, and half of these were flap-related (late wound dehiscence and/or perineal or flap infection). Late complications, occurring after more than 6 months, were identified in four patients in the musculocutaneous flap group (21.1%) and one patient in the fasciocutaneous flap group (4.0%), and consisted of persisting wound healing problems in three patients and perineal hernias in two patients, the latter both in the musculocutaneous flap group. Mean follow-up time was 9 months (range 1–32 months, SD 9), with a shorter follow-up time in the fasciocutaneous flap group compared to the musculocutaneous flap group (6 months and 12 months respectively, p = 0.092).
When looking only at the 39 ELAPE patients, we found a lower rate of flap-related complications in the group reconstructed with a fasciocutaneous flap (10 out of 24 patients, 41.7%) compared to the group reconstructed with a musculocutaneous flap (7 out of 15 patients, 46.7%), but this difference was not statistically significant (p = 0.509). The results of other analyses were the same (output not shown).
Discussion
In this retrospective cohort study of 44 patients, we reviewed the post-operative outcomes after two surgical methods of perineal reconstruction after abdominoperineal resection. We found no certain differences in post-operative rehabilitation or in complications in the two groups reconstructed with either a fasciocutaneous V–Y flap or a musculocutaneous gluteal flap.
The fasciocutaneous V–Y flap was introduced in our department in 2018, and we hypothesized it to be a quicker and safer perineal reconstruction method than the musculocutaneous gluteal flap. However, in this analysis, we were unable to detect a difference in operating time, rehabilitation time, or overall post-operative complications. We found an overall incidence of perineal post-operative complications of 39%, comparable to the previously described incidence of 42% for the musculocutaneous gluteal flap [2, 11]. Our results are similar to previously reported incidences of post-operative complications after the fasciocutaneous V–Y flap, ranging from 42 to 45% [13,14,15].
When looking only at ELAPE patients, we detected a lower rate of flap-related complications in the group reconstructed with a fasciocutaneous V–Y flap compared to the group reconstructed with a musculocutaneous flap. This difference was not statistically significant, which suggests the difference is due either to chance, or to a lack of power disguising a true difference in post-operative complication rates after perineal reconstruction in ELAPE patients, where the fasciocutaneous V–Y flap is more advantageous. This will need to be confirmed by analysis of more patients. The thinner, fasciocutaneous V–Y flap can be assumed to less effectively eliminate perineal dead space, and therefore increase the risk of for example seroma collections, but this was not reflected in our data.
Late complications, including persisting wound healing problems and perineal hernias, were identified in four patients in the musculocutaneous flap group and one patient in the fasciocutaneous flap group. However, the mean follow-up time was shorter in the fasciocutaneous flap group, since this is the newly introduced surgical approach, and thus we cannot conclude with certainty from this data that long-term complications are more common after reconstruction with the musculocutaneous gluteal flap compared to the fasciocutaneous V–Y flap. Since our center is a nationwide referral center for the treatment of advanced colorectal cancer, a majority of our patients are discharged to follow-up at their regional cancer centers, which is why our follow-up in this study is often very short. This means that, possibly, late complications may not be brought to our knowledge unless the patient has severe issues and is referred back to us, which makes our data on long-term complications unreliable. To our knowledge, only one previous study has examined the long-term complications after the fasciocutaneous V–Y flap, and detected two perineal hernias in their group of 38 ELAPE patients reconstructed with different approaches [15]. This underlines the need for more long-term follow-up and evaluation after perineal reconstruction.
This is to our knowledge the first study to compare, in the same unit, the musculocutaneous gluteal flap to the fasciocutaneous V–Y flap for perineal reconstruction after abdominoperineal reconstruction. One of the strengths of this study is the similarity between the two groups compared, with very similar patient characteristics, and treatment by the same colorectal and plastic surgery teams, respectively. Limitations include the retrospective study design, and the short follow-up times in relation to long-term complications. As a national cancer center, many of our patients are from outside the Stockholm region, making follow-up difficult. Long-term complications in both groups might have been managed in regional hospitals without being detected by us.
As our results clearly show, post-operative complications after abdominoperineal resection with perineal reconstruction affect many patients, and several factors other than the reconstructive surgery approach are likely to influence the post-operative complication rate. These include for example the extensiveness and duration of the abdominoperineal resection, the experience of the reconstructive plastic surgeon, and other variables which we were unable to control for in this analysis. It is possible that the surgical approach of perineal reconstruction matters little in relation to other variables in this high-morbidity procedure, in which case both examined reconstructive methods are equivalent. It is now more common than not that patients undergoing ELAPE have had prior radiotherapy, and it is worth noting that the local, perineal-based approach we use in both surgical techniques thus works well in this patient group.
In conclusion, our study shows that both a fasciocutaneous and a musculocutaneous flap are acceptable options for perineal reconstruction. Our data suggests that the fasciocutaneous V–Y flap might yield slightly fewer local complications in ELAPE patients, but this needs to be examined further, especially concerning the long-term outcomes.
Data availability
Data will not be shared since sharing would be in a breach of the obtained study permission from the Swedish Ethical Review Authority and of GDPR.
References
Miles WE (1971) A method of performing abdomino-perineal excision for carcinoma of the rectum and of the terminal portion of the pelvic colon (1908). CA Cancer J Clin 21(6):361–364
Holm T et al (2007) Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg 94(2):232–238
Howell AM et al (2013) How should perineal wounds be closed following abdominoperineal resection in patients post radiotherapy–primary closure or flap repair? Best evidence topic (BET). Int J Surg 11(7):514–517
Devulapalli C et al (2016) Primary versus flap closure of perineal defects following oncologic resection: a systematic review and meta-analysis. Plast Reconstr Surg 137(5):1602–1613
Foster JD et al (2018) Closure of the perineal defect after abdominoperineal excision for rectal adenocarcinoma - ACPGBI Position Statement. Colorectal Dis 20(Suppl 5):5–23
Copeland-Halperin LR et al (2020) Perineal reconstruction following abdominoperineal resection: comprehensive review of the literature. J Plast Reconstr Aesthet Surg 73(11):1924–1932
di Summa PG et al (2015) The combined pedicled anterolateral thigh and vastus lateralis flap as filler for complex perineal defects. Ann Plast Surg 75(1):66–73
Radwan RW et al (2021) Vertical rectus abdominis flap (VRAM) for perineal reconstruction following pelvic surgery: a systematic review. J Plast Reconstr Aesthet Surg 74(3):523–529
Schellerer VS et al (2021) Donor site morbidity of patients receiving vertical rectus abdominis myocutaneous flap for perineal, vaginal or inguinal reconstruction. World J Surg 45(1):132–140
Harries RL et al (2021) Outcomes following immediate vertical rectus abdominis myocutaneous (VRAM) flap-based perineal reconstruction following resectional surgery for pelvic malignancies. World J Surg 45(7):2290–2297
Anderin C et al (2012) Short-term outcome after gluteus maximus myocutaneous flap reconstruction of the pelvic floor following extra-levator abdominoperineal excision of the rectum. Colorectal Dis 14(9):1060–1064
Baloch N et al (2021) Perineal healing following salvage surgery for anal cancer. Colorectal Dis 23(5):1102–1108
Myers PL et al (2019) Gluteal flaps revisited: technical modifications for perineal wound reconstruction. Ann Plast Surg 82(6):667–670
Kokosis G et al (2019) Modified V-Y fasciocutaneous flap reconstruction after abdominoperineal resection in irradiated patients prevents wound dehiscence and associated complications: a retrospective analysis and benchtop confirmation. Ann Plast Surg 82(2):218–223
Barrie J, Haque A, Evans DA (2018) Perineal closure following extralevator abdominoperineal excision for cancer of the rectum. Colorectal Dis 20(11):981–985
Özkaya Ö et al (2018) Immediate perineal reconstruction after extralevatory abdominoperineal excision: buried desepidermised fasciocutaneous V-Y advancement flap. Ann Plast Surg 80(2):154–158
Hur K et al (2013) Patient-reported assessment of functional gait outcomes following superior gluteal artery perforator reconstruction. Plast Reconstr Surg Glob Open 1(5):e31
Funding
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and study design were performed by EKL and PS. Data collection was performed by EKL and JNG. Data analysis was performed by EKL. The first draft of the manuscript was written by JNG and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Joshua N Gertler, Pehr Sommar, and Ebba K Lindqvist declare no competing interests.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. The Swedish Ethical Review Authority approved the study (reference number 2019–04636).
Patient consent
The Swedish Ethical Review Authority approved the study (reference number 2019–04636) and confirmed that no written consent was required for this observational study. The research participants provided informed consent for publication of images.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gertler, J.N., Sommar, P. & Lindqvist, E.K. A V–Y fasciocutaneous flap for perineal reconstruction following abdominoperineal resection: quicker and better than a myocutaneous gluteal flap?. Eur J Plast Surg 46, 589–595 (2023). https://doi.org/10.1007/s00238-022-02035-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-022-02035-z