Abstract
Background
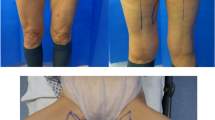
The diagonal upper gracilis myocutaneous (DUG) flap is an alternative for free autologous flap breast reconstruction. It has evolved from the transverse upper gracilis (TUG) flap by changing the orientation of the skin island, providing more bulk and easier donor site closure. This comes at the expense of a possibly more visible scar. This retrospective report aims to evaluate both clinical and patient-reported outcomes. We discuss the indications and technical details of this less common flap.
Methods
Fifteen consecutive DUG-flaps for breast reconstruction in 9 patients over a 2-year period were analysed. The skin paddle of the DUG-flaps was oriented in an oblique direction as opposed to traditional horizontal or vertical designs. Data were collected from the medical files. All patients completed the BREAST-Q questionnaire and a questionnaire about the donor site (upper thigh) and adjunctive procedures. Minimal follow-up was 20 months.
Results
In this series, there was no flap revision or flap failure. The sole complications were related to the donor site with delayed wound healing and seromas occurring in 4 patients. The mean BREAST-Q scores were 72 for quality of life and 85 for satisfaction, which is comparable to other types of free autologous flaps. Long-term discomfort during activities at the donor site scar was common. Scar visibility or the postoperative contour of the thighs was not a major concern. Adjunctive procedures further improved satisfaction with the final result.
Conclusions
The DUG flap is an improvement of the TUG flap, providing more tissue and easier donor site closure. This makes it a valuable option for breast reconstruction in women whose abdomen is not available as a donor site. In bilateral cases, it has the advantage over gluteal and lumbar flaps, that both breasts can be reconstructed in one procedure. Disadvantages include donor site problems and a high need for additional lipofilling procedures. Technical refinements of the procedure are being discussed.
Level of evidence: Level IV, Therapeutic study






Similar content being viewed by others
References
Craft RO, Colakoglu S, Curtis MS, Yueh JH, Lee BS, Tobias AM, Lee BT (2011) Patient satisfaction in unilateral and bilateral breast reconstruction. Plast Reconstr Surg 127(4):1417–24. https://doi.org/10.1097/PRS.0b013e318208d12a
Ochoa O, Garza R, Pisano S, Chrysopoulo M, Ledoux P, Arishita G, Ketchum N, Michalek JE, Nastala C (2019) Prospective longitudinal patient-reported satisfaction and health-related quality of life following DIEP flap breast reconstruction: relationship with body mass index. Plast Reconstr Surg 143(6):1589–1600. https://doi.org/10.1097/PRS.0000000000005616
Liu LQ, Branford OA, Mehigan S (2018) BREAST-Q, easurement of the patient perspective in oncoplastic breast surgery: a systematic review. Plast Reconstr Surg Glob Open 6(8):e1904. https://doi.org/10.1097/GOX.0000000000001904
Moller L, Berner JE, Dheansa B (2019) The reconstructive journey: description of the breast reconstruction pathway in a high-volume UK-based microsurgical centre. J Plast Reconstr Aesthet Surg 72(12):1930–5. https://doi.org/10.1016/j.bjps.2019.07.017
Macadam SA, Zhong T, Weichman K, Papsdorf M, Lennox PA, Hazen A, Matros E, Disa J, Mehrara B, Pusic A (2016) Quality of Life and patient-reported outcomes in breast cancer survivors: a multicenter comparison of four abdominally based autologous reconstruction methods. Plast Reconstr Surg 137(3):758–71. https://doi.org/10.1097/01.prs.0000479932.11170.8f
Colakoglu S, Khansa I, Curtis MS, Yueh JH, Ogunleye A, Haewyon C, Tobias AM, Lee BT (2011) Impact of complications on patient satisfaction in breast reconstruction. Plast Reconstr Surg 127(4):1428–36. https://doi.org/10.1097/PRS.0b013e318208d0d4
Yueh JH, Slavin SA, Adesiyun T, Nyame TT, Gautam S, Morris DJ, Tobias AM, Lee BT (2010) Patient satisfaction in postmastectomy breast reconstruction: a comparative evaluation of DIEP, TRAM, latissimus flap, and implant techniques. Plast Reconstr Surg 125(6):1585–95. https://doi.org/10.1097/PRS.0b013e3181cb6351
Pien I, Caccavale S, Cheung MC, Butala P, Hughes DB, Ligh C, Zenn MR, Hollenbeck ST (2016) Evolving trends in autologous breast reconstruction: is the deep inferior epigastric artery perforator flap taking over? Ann Plast Surg 76(5):489–93. https://doi.org/10.1097/SAP.0000000000000339
Erdmann-Sager J, Wilkins EG, Pusic AL, Qi J, Hamill JB, Kim HM, Guldbrandsen GE, Chun YS (2018) Complications and patient-reported outcomes after abdominally based breast reconstruction: results of the mastectomy reconstruction outcomes consortium study. Plast Reconstr Surg 141(2):271–81. https://doi.org/10.1097/PRS.0000000000004016
Dayan JH, Allen RJ (2019) Neurotized diagonal profunda artery perforator flaps for breast reconstruction. Plast Reconstr Surg Glob Open 7(10):e2463. https://doi.org/10.1097/GOX.0000000000002463
Lee CD, Butterworth J, Stephens R, Wright B, Surek C (2019) Reply: location of the internal mammary vessels for microvascular autologous breast reconstruction: the “1–2–3 rule.” Plast Reconstr Surg 143(5):1121e–2e. https://doi.org/10.1097/PRS.0000000000005540
Sojitra NM, Fabre G, Vandevoort M (2010) A valuable method for exposure of the recipient internal mammary vessels for microvascular breast reconstruction. Plast Reconstr Surg 125(2):77e–8e. https://doi.org/10.1097/PRS.0b013e3181c725d2
Saint-Cyr M, Wong C, Oni G, Maia M, Trussler A, Mojallal A, Rohrich RJ (2012) Modifications to extend the transverse upper gracilis flap in breast reconstruction: clinical series and results. Plast Reconstr Surg 129(1):24e–36e. https://doi.org/10.1097/PRS.0b013e31823620cb
Arnez ZM, Pogorelec D, Planinsek F, Ahcan U (2004) Breast reconstruction by the free transverse gracilis (TUG) flap. Br J Plast Surg 57(1):20–6. https://doi.org/10.1016/j.bjps.2003.10.007
Buntic RF, Horton KM, Brooks D, Althubaiti GA (2011) Transverse upper gracilis flap as an alternative to abdominal tissue breast reconstruction: technique and modifications. Plast Reconstr Surg 128(6):607e–13e 15. https://doi.org/10.1097/PRS.0b013e318230c2b6
Saour S, Libondi G, Ramakrishnan V (2017) Microsurgical refinements with the use of internal mammary (IM) perforators as recipient vessels in transverse upper gracilis (TUG) autologous breast reconstruction. Gland Surg 6(4):375–9 16. https://doi.org/10.21037/gs.2017.05.04
Hunter JE, Mackey SP, Boca R, Harris PA (2014) Microvascular modifications to optimize the transverse upper gracilis flap for breast reconstruction. Plast Reconstr Surg 133(6):1315–25. https://doi.org/10.1097/PRS.0000000000000173
McKane BW, Korn PT (2012) The fleur-de-lis upper gracilis flap for breast reconstruction: flap design and outcome. Ann Plast Surg 69(4):383–6. https://doi.org/10.1097/SAP.0b013e31824b25c1
Fattah A, Figus A, Mathur B, Ramakrishnan VV (2010) The transverse myocutaneous gracilis flap: technical refinements. J Plast Reconstr Aesthet Surg 63(2):305–13. https://doi.org/10.1016/j.bjps.2008.10.015
Dayan J (2015) Network PSE. Diagonal upper gracilis (DUG) flap. Arlington Heights, IL; Plastic Surgery Eduction Network, ASPS Online Learning Department
Samra F, Sobti N, Nelson JA, Allen RJ, Mehrara B, Dayan JH (2019) Frontiers in oncologic reconstruction. Plast Reconstr Surg Glob Open 7(6):e2181. https://doi.org/10.1097/GOX.0000000000002181
Dayan E, Smith ML, Sultan M, Samson W, Dayan JH (2013) The diagonal upper gracilis (DUG) flap: a safe and improved alternative to the TUG flap. Plast Reconstr Surg 132(4S–1):33–4. https://doi.org/10.1097/01.prs.0000435901.60333.62
Locke MB, Zhong T, Mureau MA, Hofer SO (2012) Tug ‘O’ war: challenges of transverse upper gracilis (TUG) myocutaneous free flap breast reconstruction. J Plast Reconstr Aesthet Surg 65(8):1041–50. https://doi.org/10.1016/j.bjps.2012.02.020
Park JE, Alkureishi LW, Song DH (2015) TUGs into VUGs and friendly BUGs: transforming the gracilis territory into the best secondary breast reconstructive option. Plast Reconstr Surg 136:447454. https://doi.org/10.1097/PRS.0000000000001557
Deutinger M, Kuzbari R, Paternostro-Sluga T, Quittan M, Zauner-Dungl A, Worseg A, Todoroff B, Holle J (1995) Donor-site morbidity of the gracilis flap. Plast Reconstr Surg 95(7):1240–4. https://doi.org/10.1097/00006534-199506000-00015
Carr M, Manktelow RT, Zuker RM (1995) Gracilis donor site morbidity. Microsurg 16(9):598–600. https://doi.org/10.1002/micr.1920160904
Craggs B, Vanmierlo B, Zeltzer A, Buyl R, Haentjens P, Hamdi M (2014) Donor-site morbidity following harvest of the transverse myocutaneous gracilis flap for breast reconstruction. Plast Reconstr Surg 134(5):682e–691e. https://doi.org/10.1097/PRS.0000000000000612
Jessica AS, Zhao J, Mackey S, Blackburn AV (2022) Transverse upper gracilis flap breast reconstruction: a 5-year consecutive case series of patient-reported outcomes. Plast Reconstr Surg 150(2):258–268. https://doi.org/10.1097/PRS.0000000000009362
Weitgasser L, Mahrhofer M, Schwaiger K, Bachleitner K, Russe E, Wechselberger G, Schoeller T (2021) lessons learned from 30 years of transverse myocutaneous gracilis flap breast reconstruction: historical appraisal and review of the present literature and 300 cases. J Clin Med 10(16):3629. https://doi.org/10.3390/jcm10163629
Siegwart LC, Fischer S, Diehm YF, Heil JM, Hirche C, Kneser U, Kotsougiani-Fischer D (2021) The transverse musculocutaneous gracilis flap for autologous breast reconstruction: focus on donor site morbidity. Breast Cancer 28(6):1273–1282. https://doi.org/10.1007/s12282-021-01264-7
Stocco C, Figus A, Razzano S (2018) Upgrading the BREAST-Q questionnaire with donor site evaluation after PAP flap breast reconstruction. J Plast Reconstr Aesthet Surg 71(6):928–929. https://doi.org/10.1016/j.bjps.2018.01.025
Funding
None of the authors received funding for their collaboration in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent to participate
Informed consent was obtained from all the individual participants included in the study.
Ethical approval
The AZ Monica ethics committee had no comments on the competence of the investigator and his staff, the suitability of the facilities and the protocol. The study was approved and can be conducted in our hospital. The ethics committee stresses that a favorable opinion does not signify that the committee assumes responsibility for the study.
Consent for publication
The authors affirm that participants provided informed consent for publication of the images in Figs. 1, 2, 3, 4, 5 and 6.
Conflict of interest
The authors Steven D. M. Colpaert, Astrid Heeren, Sarantos Papadopoulos, Nadeem Akhtar and Marc Van Cleemput declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 466389 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Colpaert, S.D.M., Heeren, A., Papadopoulos, S. et al. Diagonal upper gracilis (DUG) flap for autologous breast reconstruction: a case series. Eur J Plast Surg 46, 367–376 (2023). https://doi.org/10.1007/s00238-022-02013-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-022-02013-5