Abstract
Background
The transversus abdominus plane (TAP) block reduces postoperative donor site pain in patients undergoing autologous breast reconstruction with an abdominally based flap. This study aimed to determine the effect of TAP blocks on rates of conversion to chronic opioid use.
Methods
The Clinformatics Data Mart was queried from 2003 to 2019, extracting adult encounters for abdominally based free and pedicled flaps based on common procedural terminology (CPT) codes. Patients were excluded if they had filled a narcotic prescription 1 year to 30 days prior to surgery. The exposure variable—TAP block—was identified by CPT codes. Outcomes were evaluated using morphine milligram equivalents (MME) from prescriptions filled between 30 days prior to and 30 days after surgery. Chronic opioid use (COU) was defined as receiving 4 unique prescriptions or a 60-day supply between 30 and 180 days after surgery.
Results
Of the 4091 patients, (mean age 51.2 ± 9.0 years), 181 (4.4%) had a TAP block placed. Perioperative MMEs/day, postoperative COU, and length of stay did not differ in patients who received a TAP block (p = 0.142; p = 0.271). Significant predictors of risk of conversion to COU included younger age, pedicled abdominal flap, Elixhauser comorbidity index score > 3, filling a psychiatric medication prescription, and filling a benzodiazepine prescription.
Conclusions
In patients undergoing autologous breast reconstruction with abdominally based flap reconstruction, TAP blocks do not decrease perioperative MME/day, conversion to chronic opioid use, or length of stay. These data suggest that intraoperative TAP block placement may be a low-yield opioid-reduction strategy.
Level of evidence: Level III, risk/prognostic study
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The opioid epidemic has been a significant public health crisis in the USA for over three decades [1]. The COVID-19 pandemic has accelerated this trend; the US Center for Disease Control reported the highest number of deaths due to opioid overdose ever recorded in the 12-month period leading up to May 2020 [2]. The link between opioid-prescribing practices and overdose is well-established; opioid prescribing has quadrupled since 1999 and has increased concomitantly with the number of overdoses from prescription opioids [3, 4]. Physicians and policymakers thus continue to advocate for innovative strategies to reduce opioid prescriptions, such as implementing mandatory prescription drug monitoring programs in high-risk states [5, 6].
Surgical patients present a unique challenge because healthcare providers must balance minimizing opioid prescriptions with adequately managing their patients’ acute pain. Postoperative narcotic use is associated with ileus, respiratory depression, hypotension, lethargy, nausea, and risk of prolonged use [7]. At the same time, uncontrolled acute postsurgical pain has been shown to correlate to the development of chronic pain, and opioids are a highly effective postoperative analgesic [8].
One opioid-sparing modality specific to surgical patients is the use of the nerve blocks. Nerve blocks are thought to prevent the sensitization of pain pathways, thereby protecting against persistent neuropathic pain even after the effect of the block has subsided [9]. However, while there is some evidence that regional anesthesia decreases postoperative narcotic requirements, the impact on prolonged opioid use is mixed [10,11,12].
Over 12,000 abdominally based microsurgical breast reconstruction surgeries were performed in the USA in 2019, and there has been an increasing emphasis on minimizing opioid use in these patients [13, 14]. The transversus abdominus plane (TAP) block is one such strategy. TAP blocks involve injecting local anesthetic under ultrasound guidance between the internal oblique and transversus abdominus muscles in the plane of the intercostal nerves, thus targeting what tends to be the most painful surgical site for patients [15]. Reflecting the broader trend seen with regional anesthesia, studies on the efficacy of TAP blocks have been mixed. Some studies show that TAP blocks may decrease length of inpatient stay in microsurgical breast reconstruction patients, while others identify negligible effects on postoperative narcotic use [15,16,17]. Furthermore, these data are from single centers and are generally limited to the inpatient setting. The long-term impact of TAP blocks on prolonged opioid use after hospital discharge is unknown. Ascertaining the true value of the TAP block could help optimize enhanced recovery after surgery (ERAS) protocols and improve allocation of healthcare resources.
We used a national dataset to evaluate demographic characteristics and postoperative outcomes in opioid-naïve women undergoing breast reconstruction with an abdominally based free or pedicled flap with or without placement of a TAP block. We hypothesized that TAP blocks would be associated with (1) a reduction in postoperative narcotic use and (2) a decrease in the rate of conversion to prolonged opioid use.
Methods
Data source and study cohort
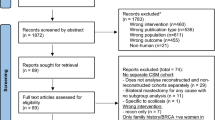
We conducted a retrospective analysis of the Clinformatics® Data Mart Database, a de-identified commercial claims data warehouse, to evaluate demographic characteristics and postoperative outcomes in women undergoing abdominally based free or pedicled flap breast reconstruction with or without placement of a TAP block between January 1, 2003, and September 30, 2019. The Optum Clinformatics® Data Mart Database is an adjudicated administrative health database containing commercial insurance claims data (inpatient/outpatient medical conditions, medications, and laboratory data) for US patients aged between 0 and 90 years in all fifty states, comprised of 7,114,773,019 claims involving 63,539,367 unique patients. The database includes information on retirees insured by Medicare who also receive supplemental employer insurance. This database has been validated against multiple claims datasets including the IBM Marketscan® Commercial Database. From this dataset, we isolated and analyzed opioid-naïve female patients aged 18 years and older with at least 1-year of continuous enrollment. Patients were considered opioid-naïve if they did not fill a narcotic prescription from 1 year to 31 days prior to surgery (Fig. 1). Patients who had records of additional procedures involving anesthesia within 180 days of their index surgery were excluded. Those who underwent autologous breast reconstruction with an abdominally based flap and intraoperative TAP block were identified using common procedural terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes (Appendix Table 5). The utilization of both of the CPT and HCPCS coding systems, managed by the American Medical Association (AMA) and the Centers for Medicare and Medicaid Services (CMS), respectively, ensured maximal inclusion of the desired patient population [18]. Morphine milligram equivalents (MME) were calculated for perioperative prescriptions which were filled between 30 days prior to and 30 days after surgery. The definition of the perioperative period for opioid prescriptions varies among studies; we chose 30 days prior to surgery and 30 days after surgery [19]. This time period captures any opioids that are prescribed at the preoperative evaluation that occurs at most institutions in the month prior to surgery, as well as during the postoperative period that aligns with the US Centers for Medicare and Medicaid outcome measure of the 30-day readmission rate. We defined prolonged opioid use (POU) as receiving at least four (4) unique prescriptions and/or at least a 60-day supply between 31 and 180 days after surgery. Together, these metrics provide a comprehensive assessment of prolonged opioid use in formerly opioid-naïve patients following the index reconstruction surgery.
Flow diagram of patients undergoing autologous breast reconstruction with an abdominally based free or pedicled flap, with or without a TAP block, screened for conversion to POU in the Clinformatics.® database. Patients were identified through CPT and HCPCS codes (Appendix Table 5)
Diagnoses and prescription claims
Insurance claims data were used to identify reconstruction laterality, pedicled or free flap, patient age, and length of stay. Comorbidities were assessed and reported with the Elixhauser index, using the International Classification of Disease, Ninth (ICD-9) and Tenth Edition (ICD-10) codes. ICD-9 codes were included unless patients had an existing ICD-10 diagnosis, in which case only ICD-10 diagnoses were evaluated. Pharmaceutical claims data were used to identify filled prescriptions of opioids, benzodiazepines, and non-opioid, non-benzodiazepine mood or psychiatric medications during the study period. Using the Centers for Medicare and Medicaid Services’ publicly available morphine equivalents per milligram conversion factors, we calculated daily oral morphine milligram equivalents (MME). Patients who filled any benzodiazepine prescription during the preoperative period (1 year to 31 days prior to surgery), during the perioperative period (30 days prior to 30 days after surgery), and during the postoperative period (31 days to 180 days after surgery) were identified. Patients were placed in two categories: those who filled any non-opioid, non-benzodiazepine mood or psychiatric medication during the study period (1 year prior to 180 days after surgery) and those who did not. Opioid and non-opioid prescriptions were identified by the American Hospital Formulary Service (AHFS) Classification codes or by generic names, respectively. A list of these codes generic drug names for which prescription claims were queried can be found in accompanying Appendix Table 6.
Outcomes
The following outcomes were analyzed in this study population: (1) average daily perioperative morphine milligram equivalents (MME) (filled between 30 days prior to and 30 days after the index surgery), (2) conversion to prolonged opioid use (POU) as measured by prolonged fills (4 + unique prescriptions or 60 + day supply of opioid medications in the postoperative period [31 days prior to 180 days prior to the index surgery]), and (3) length of inpatient stay (LOS) related to the index autologous breast reconstruction procedure,.
Covariables and statistical analysis for perioperative MME/day, POU outcomes, and LOS
We used multivariable linear regression to calculate the average difference in perioperative MME/day attributable to each independent variable. The following covariates of average daily perioperative MME were included: (1) flap type (free or pedicled flap), (2) procedure laterality (unilateral or bilateral), (3) TAP block at the time of breast reconstruction, (4) age (18 to 34 years, 35 to 44 years, 45 to 54 years, 55 to 64 years, and 65 years and older), (5) comorbidities, as measured and reported by the Elixhauser index using ICD-9 and ICD-10 codes, (6) presence or absence of a filled benzodiazepine prescription during the preoperative period (1 year to 31 days prior to surgery), (7) presence or absence of a filled benzodiazepine prescription during the perioperative period (30 days prior to 30 days after surgery), and (8) presence or absence of a filled non-opioid, non-benzodiazepine mood or psychiatric prescription during the study period (1 year prior to 180 days after surgery).
We used multivariable logistic regression to calculate adjusted odds ratios for conversion to POU for each independent variable included in the model. The following covariates of conversion to POU were included: (1) flap type (free or pedicled flap), (2) procedure laterality (unilateral or bilateral), (3) TAP block at the time of breast reconstruction, (4) age (18 to 34 years, 35 to 44 years, 45 to 54 years, 55 to 64 years, and 65 years and older), (5) comorbidities, as measured and reported by the Elixhauser index using ICD-9 and ICD-10 codes, (6) presence or absence of a filled benzodiazepine prescription during the preoperative period (1 year to 31 days prior to surgery), (7) presence or absence of a filled benzodiazepine prescription during the perioperative period (30 days prior to 30 days after surgery), (8) presence or absence of a filled benzodiazepine prescription during the postoperative period (31 days to 180 days after surgery), and (9) presence or absence of a filled non-opioid, non-benzodiazepine mood or psychiatric prescription during the study period (1 year prior to 180 days after surgery).
We used multivariable linear regression to calculate the average difference in length of stay attributable to each independent variable. The following covariates were included: (1) flap type (free or pedicled flap), (2) procedure laterality (unilateral or bilateral), (3) TAP block at the time of breast reconstruction, (4) age (18 to 34 years, 35 to 44 years, 45 to 54 years, 55 to 64 years, and 65 years and older), (5) comorbidities, as measured and reported by the Elixhauser index using ICD-9 and ICD-10 codes, (6) presence or absence of a filled benzodiazepine prescription during the preoperative period (1 year to 31 days prior to surgery), and (7) presence or absence of a filled non-opioid, non-benzodiazepine mood or psychiatric prescription during the study period (1 year prior to 180 days after surgery).
Schapiro-Wilk testing was used to determine whether continuous variables were normally distributed. Chi squared tests, Mann–Whitney-Wilcoxon tests, and multivariate regressions were used for statistical analysis. P values of < 0.05 were considered statistically significant. All analyses were completed using Stata, version 16.1 (StataCorp LLC).
Results
Patient characteristics
There were 4091 patients that met inclusion criteria and were included in this analysis (Table 1). Seventy-nine percent of patients underwent unilateral breast reconstruction. Only 4% of patients received an intraoperative TAP block. Free flap breast reconstruction was more common than pedicled flap reconstruction (68 vs. 32%). The majority of patients were aged 45 or older. The mean length of inpatient hospital stay was 3.37 days. The majority of patients had more than two comorbidities. Ninety percent of patients were prescribed opioids perioperatively. Regarding benzodiazepine prescriptions, 23% filled a prescription preoperatively, 25% filled a prescription perioperatively, and 36% filled a prescription postoperatively. Thirty-five percent of patients filled a non-benzodiazepine psychiatric medication either preoperatively, perioperatively, or postoperatively. There was an 11% overall conversion rate to prolonged opioid use.
Patient factors and predictors of increased perioperative MME/day
Table 2 describes the patient characteristics associated with variations in perioperative narcotic prescriptions. There was a statistically significant decrease in perioperative MME/day in patients older than 55 (p = 0.031). We also found that patients with greater than three comorbidities were prescribed increased MME/day (average increase 0.670, p < 0.001). Additional predictors of increased MME/day were pedicled flap reconstruction (average increase 1.002, p < 0.001) and filling a mood-related medication (average increase of 0.619, p = 0.001).
Patient factors and predictors of conversion to POU
Table 3 describes the patient characteristics associated with an increased risk of POU (4 + unique prescriptions or 60 + day supply of opioid medications in the postoperative period). We observed the following risk factors for conversion to POU: pedicled flap reconstruction (OR 1.559, p < 0.001), having greater than three comorbidities (OR 1.952, p < 0.001), filling a benzodiazepine prescription postoperatively (OR 1.897, p < 0.001), and filling a psychiatric medication prescription (OR 1.471, p = 0.007). We found that older age was a protective factor associated with a lower risk of conversion to POU. Unilateral vs. bilateral reconstruction, placement of a TAP block, and either preoperative or perioperative benzodiazepine use had no significant effect on conversion to POU.
Patient factors and predictors of LOS
Table 4 describes the patient factors associated with differences in LOS. We observed the following factors that significantly increased LOS: older age (p < 0.001), free flap breast reconstruction (p < 0.001), and taking a mood or psychiatric mediation (p = 0.031). Preoperative benzodiazepine use was mildly protective (average decrease of 0.266 days, p = 0.031). There was no statistically significant effect of unilateral vs. bilateral reconstruction or TAP block. The effect of the number of comorbidities was equivocal.
Discussion
The efficacy of TAP blocks to reduce opioid use after this procedure is controversial and is based largely on single-center, retrospective chart review data, so we sought to analyze longitudinal patient data from a national claims database. We found that TAP blocks did not have an appreciable effect on either postoperative narcotic prescriptions or conversion to prolonged opioid use. A systemic review by Abdou et al. of single-center studies on patients undergoing abdominally based microsurgical breast reconstruction indicated a statistically significant reduction in total opioid consumption with the use of a TAP block in the inpatient setting; however, other studies have indicated no significant reduction [17, 20]. Moreover, there is scarce data in the literature on the long-term impact of TAP blocks on opioid use. Our results are consistent with those from a study by Pan et al. which showed that the TAP block did not reduce prolonged postsurgical pain at 3 and 6 months after colorectal surgery [21]. Thus, any possible reduction in acute postoperative pain from a TAP block may not translate to a decreased risk of prolonged pain requiring narcotics. Furthermore, we found that TAP blocks did not significantly impact LOS, similar to the findings of Hunter et al.[17] Taken together, our analysis suggests that the costs and risks associated with TAP blocks, including intravascular injection, laceration of intra-abdominal organs, femoral nerve palsy, and infection, may outweigh the benefits [22]. It is important to note that our study only considers the impact of the TAP block on long-term opioid use, but does not capture the impact on short-term analgesia; one meta-analysis found that ultrasound-guided TAP block does decrease opioid consumption within six hours after abdominal laparotomy, abdominal laparoscopy, and cesarean delivery, without serious complications [23]. The scope of our study is limited to assessing the long-term effect of the TAP block on persistent postoperative opioid use. However, the TAP block may still have utility in reducing patient discomfort in the immediate postoperative period, particularly in breast reconstruction patients who have a self-reported poor pain tolerance or are chronic opioid users. Further prospective studies are needed to evaluate the utility of the TAP block in these subsets of patients.
We next analyzed other patient factors impacting perioperative MME/day, POU conversion rates, and LOS. Patients were stratified into five age groups, and we discovered that as expected, older patients stayed in the hospital longer after surgery. However, older age was also predictive of decreased perioperative MME/day and decreased POU conversion risk. Prior studies have shown that younger patients are more likely to develop persistent opioid use after total hip arthroplasty, open cardiac surgery, and urologic surgery [24,25,26]. There is evidence that younger patients are more likely to request and receive an opioid refill after surgery, while the elderly are more often undertreated for pain [26, 27]. We additionally observed that patients with greater than 3 comorbidities were more likely to receive increased MME/day as well as convert to POU compared to patients with no comorbidities or a single comorbidity, consistent with the findings of Marcusa et al.[14] These data may help aid physicians appropriately calibrate their opioid-prescribing practices based on patient demographic factors.
We found that free flaps were protective for perioperative MME/day as well as POU conversion as compared to pedicled flaps. In recent years, microsurgeons have developed techniques to increasingly spare rectus abdominus muscle during deep inferior epigastric perforator pedicle dissection in abdominal free flaps. In contrast, pedicled abdominal flaps usually require sacrifice of the muscle. Our results are consistent with previous findings that sparing rectus muscle decreases donor site morbidity and pain in breast reconstruction [28].
We parsed benzodiazepine use into three categories: preoperative, perioperative, and postoperative. We considered temporality of benzodiazepine use because we wanted to differentiate between prolonged preoperative benzodiazepine use as a possible risk factor for POU versus the possible ability for benzodiazepines to act as an analgesic in itself, thereby reducing prolonged opioid use. Interestingly, we found that postoperative benzodiazepine use increases risk of POU. A retrospective study by Sun et al. found that concomitant opioid and benzodiazepine use increased sharply from 2001 to 2013, and that benzodiazepine use potentiates the risk of death from opioid overdose [29]. Similarly, we found that use of a psychiatric or mood-related medication increases risk of POU, congruent with the link between mental health diagnoses and POU established in multiple studies [14, 30, 31]. Surgeons, primary care physicians, and mental health providers too often work in silos; our results suggest that coordination of postoperative care in high-risk patients could have a high-yield impact on mitigating conversion to POU.
Our study has a number of limitations. The first of these relates to the source of our data; the Optum claims database includes information on prescribed opioids but does not provide data on whether patients actually consumed the medication or whether their pain was adequately treated. The database deidentifies individual prescribers, so we were not able to parse out the effects of variations in prescribing practices. Additionally, due to bundling of procedures in flap CPT codes, we were unable to capture TAP blocks placed by the operating surgeon; only TAP blocks placed by a different provider, such as an anesthesiologist, were captured. Differences in TAP placement technique by individual providers could not be delineated. We were not able to distinguish different types of anesthetic instilled in the block (i.e., bupivacaine, lidocaine, or ropivacaine). We chose to focus on single-shot intraoperative TAP blocks rather than continuous infusion since the data set did not provide information on dosing and duration of continuous blocks. We also did not differentiate among types of flaps (i.e., MS-0, I, II, or III TRAM) or need for mesh reinforcement at the donor site.
In addition, our study did not distinguish between delayed and immediate flap reconstruction; therefore, it does not capture differences in opioid consumption stemming from mastectomy-related pain. Although patient socioeconomic level, race, and type of insurance coverage have been shown to impact opioid consumption after surgery, we chose not to consider these factors. The effects of chemotherapy and radiation on opioid consumption are beyond the scope of this study.
Conclusions
In patients undergoing autologous breast reconstruction with abdominally based flap reconstruction, TAP blocks did not decrease perioperative MME/day, conversion to prolonged opioid use, or length of stay. While some studies support the benefits of TAP blocks for inpatient management of pain, these data suggest that TAP block placement may be a low-yield strategy to reduce postoperative narcotic or prevent conversion to opioid-use disorder.
References
Lyden J, Binswanger IA (2019) The United States opioid epidemic. Semin Perinatol 43:123–131
Overdose Deaths Accelerating During COVID-19 | CDC Online Newsroom | CDC. https://www-cdc-gov.laneproxy.stanford.edu/media/releases/2020/p1218-overdose-deaths-covid-19.html
Bohnert ASB et al (2011) Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA - J Am Med Assoc 305:1315–1321
Increases in Drug and Opioid Overdose Deaths — United States (2000–2014). https://www-cdc-gov.laneproxy.stanford.edu/mmwr/preview/mmwrhtml/mm6450a3.htm
Strickler GK et al (2019) Effects of mandatory prescription drug monitoring program (PDMP) use laws on prescriber registration and use and on risky prescribing. Drug Alcohol Depend 199:1–9
Shev AB et al (2018) Prescription drug monitoring program: registration and use by prescribers and pharmacists before and after legal mandatory registration, California, 2010–2017. Am J Public Health 108:1669–1674
Alam A et al (2012) Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med 172:425–430
Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E (2017) Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg 125:1733–1740
Dahl JB, Møiniche S (2004) Pre-emptive analgesia. Br Med Bull 71:13–27
Chan EY, Fransen M, Parker DA, Assam PN, Chua N (2014) Femoral nerve blocks for acute postoperative pain after knee replacement surgery. Cochrane Database Syst Rev 2014
Andreae MH, Andreae DA (2013) Regional anaesthesia to prevent chronic pain after surgery: a Cochrane systematic review and meta-analysis. Br J Anaesth 111:711–720
Sun EC et al (2017) Lack of Association between the use of nerve blockade and the risk of postoperative chronic opioid use among patients undergoing total knee arthroplasty: evidence from the Marketscan Database. Anesth Analg 125:999–1007
Plastic Surgery Statistics Report (2019) https://pwww.plasticsurgery.org/2Fdocuments/2FNews/2FStatistics/2F2019/2Fplastic-surgery-statistics-full-report-2019.pdf
Marcusa DP et al (2017) Prescription opioid use among opioid-naive women undergoing immediate breast reconstruction. Plast Reconstr Surg 140:1081–1090
Jablonka EM et al (2017) Transversus abdominis plane blocks with single-dose liposomal bupivacaine in conjunction with a nonnarcotic pain regimen help reduce length of stay following abdominally based microsurgical breast reconstruction. Plastic Reconst Surg 140:240–251 (Lippincott Williams and Wilkins)
Zhong T et al (2014) Transversus abdominis plane block reduces morphine consumption in the early postoperative period following microsurgical abdominal tissue breast reconstruction: a double-blind, placebo-controlled, randomized trial. Plastic Reconst Surg 134:870–878 (Lippincott Williams and Wilkins)
Hunter C et al (2017) Transversus abdominis plane block and free flap abdominal tissue breast reconstruction. Ann Plast Surg 78:254–259
Cibas ES (2014) Chapter 18 - Laboratory management. In: Cibas ES, Ducatman BS (eds) Cytology, 3rd edn. W.B. Saunders, p 519–546. https://doi.org/10.1016/B978-1-4557-4462-6.00018-0 (https://www.sciencedirect.com/science/article/pii/B9781455744626000180)
Ho VT et al (2021) Increasing chronic opioid usage despite reduced prescriptions after vascular surgery. J Vasc Surg 74:e285–e286
Abdou SA, Daar DA, Wilson SC, Thanik V (2020) Transversus abdominis plane blocks in microsurgical breast reconstruction: a systematic review and meta-analysis. J Reconstr Microsurg 36:353–361
Pan ZY et al (2020) The effect of transversus abdominis plane block on the chronic pain after colorectal surgery: a retrospective cohort study. BMC Anesthesiol 20:116
Jankovic Z, Ahmad N, Ravishankar N, Archer F (2008) Transversus abdominis plane block: how safe is it? Anesth Analg 107:1758–1759
Baeriswyl M, Kirkham KR, Kern C, Albrecht E (2015) The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg 121:1640–1654
Inacio MCS, Hansen C, Pratt NL, Graves SE, Roughead EE (2016) Risk factors for persistent and new chronic opioid use in patients undergoing total hip arthroplasty: a retrospective cohort study. BMJ 29;6(4):e010664. https://doi.org/10.1136/bmjopen-2015-010664
Brown CR, Chen Z, Khurshan F, Groeneveld PW, Desai ND (2020) Development of persistent opioid use after cardiac surgery. JAMA Cardiol 5:889–896
Ziegelmann MJ et al (2019) Wide variation in opioid prescribing after urological surgery in tertiary care centers. Mayo Clin Proc 94:262–274
Cavalieri TA (2007) Managing pain in geriatric patients. J Osteopath Med 107:E10-E16. https://doi.org/10.7556/jaoa.2007.20014
Butler PD, Wu LC (2015) Abdominal perforator vs. muscle sparing flaps for breast reconstruction. Gland surg 4:212–21221
Sun EC et al (2017) Association between concurrent use of prescription opioids and benzodiazepines and overdose retrospective analysis. BMJ (Online) 356:760
Wilsey BL, Fishman SM, Tsodikov A, et al (2008) Psychological comorbidities predicting prescription opioid abuse among patients in chronic pain presenting to the emergency department. Pain Medicine 9: 1107–1117. https://doi.org/10.1111/j.1526-4637.2007.00401.x
Mellbye A, Svendsen K, Borchgrevink PC, Skurtveit S, Fredheim OMS (2012) Concomitant medication among persistent opioid users with chronic non-malignant pain. Acta Anaesthesiol Scand 56:1267–1276
Acknowledgements
Data for this project were accessed using the Stanford Center for Population Health Sciences Data Core. The PHS Data Core is supported by a National Institutes of Health National Center for Advancing Translational Science Clinical and Translational Science Award (UL1 TR001085) and from Internal Stanford funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This is an observational study using a large national deidentified database. The Stanford IRB Committee has confirmed that no ethical approval is required.
Consent to participate
No informed consent was required for this database study.
Conflict of interest
Rahim Nazerali is a consultant for MTF, Mentor, and Telabio. Arhana Chattopadhyay, Jennifer Krupa Shah, Pooja Yesantharao, Vy Thuy Ho, and Clifford Sheckter report no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chattopadhyay, A., Shah, J.K., Yesantharao, P. et al. Transversus abdominus plane blocks do not reduce rates of postoperative prolonged opioid use following abdominally based autologous breast reconstruction: a nationwide longitudinal analysis. Eur J Plast Surg 46, 203–213 (2023). https://doi.org/10.1007/s00238-022-01996-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-022-01996-5