Abstract
Background
Total laryngectomy (TL) as either a primary or salvage treatment strategy remains an effective oncologic operation in the management of laryngeal cancer. Dysphagia is the most common complication following TL and this has a significant impact on patients’ quality of life (QOL). Following removal of the larynx, a number of pharyngeal closure techniques exist. We aimed to evaluate the effect pharyngeal closure techniques have on dysphagia-specific QOL postoperatively.
Methods
We retrospectively reviewed patients who had undergone TL at our institution (2014–2019). Patients alive at the time of study were invited to complete the MD Anderson Dysphagia Inventory (MDADI). Outcomes were compared among Primary Closure (PC), Pedicled Pectoralis Major Myocutaneous Flap (PMMF) and Free Flap (FF) closure groups.
Results
There were 27 patients identified for inclusion. Eight patients (30%) underwent PC, 10 patients (37%) had PMMF-assisted closure and 9 patients (33%) underwent FF-assisted closure. Patients within the FF group scored consistently higher MDADI scores across all subscales (emotional, functional, physical, global) as well as composite MDADI score in comparison to the PC and PMMF groups. FF closure was associated with a reduced inpatient length of stay (LOS). Additionally, no significant differences in postoperative morbidity including rates of pharyngo-cutaneous fistula (PCF) were observed between groups.
Conclusions
We now advocate FF closure for our patients following salvage TL due to the improved dysphagia-specific QOL, reduced inpatient LOS and lack of additional surgical morbidity.
Level of evidence, Level III, therapeutic/prognostic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The National Cancer Institute Surveillance, Epidemiology and End-Results Program database estimates that approximately 12,370 new cases of laryngeal cancer were diagnosed within the USA in 2020 [1]. Historically, the primary treatment strategy for laryngeal cancer was surgical removal of the larynx which has a significant impact on patients’ ability to speak and to swallow. The management of laryngeal cancer has since undergone a paradigm shift over the last 30 years following publication of the VA Larynx and RTOG 91–11 trials with most patients now treated with chemoradiotherapy instead of surgery [2, 3]. Chemoradiotherapy aims to preserve patients’ speech and swallow function. However, some patients still require total laryngectomy (TL). TL remains an effective yet highly morbid operation for patients with advanced laryngeal cancer and those with either residual or recurrent disease following chemoradiotherapy. Complications of TL can include infection, haemorrhage, wound dehiscence, death and development of a pharyngo-cutaneous fistula (PCF). Rates of these complications particularly PCF rates are higher in those who undergo ‘salvage’ TL following radiotherapy with or without chemotherapy.
Multiple pharyngeal closure techniques exist following TL and these techniques can broadly be divided into Primary Closure (PC) and flap-assisted closure. Patients undergoing salvage TL more frequently undergo flap-assisted closure in comparison to those undergoing primary surgery in order to reduce the risk of a postoperative PCF [4]. The use of flap-assisted pharyngeal closure techniques following primary TL is less widespread as surgeons have less concern directly opposing healthy non-irradiated tissue [4]. Flap-assisted closure techniques can be achieved with a pedicled flap (usually a Pectoralis Major Myocutaneous Flap (PMMF)) or via Free Flap (FF) techniques (typically either an Antero-Lateral Thigh flap (ALT) or Radial Forearm Free Flap (RFFF)). Other pharyngeal closure techniques have been described within the literature such as the temporoparietal fascia free flap and the islanded facial artery musculo-mucosal flap but these are not in widespread use [5, 6].
TL also leads to a number of functional complications as removal of the larynx affects patients’ ability to speak and to swallow as well as their body image. These factors significantly impact on patients’ quality of life (QOL) following TL. Dysphagia is the most frequently cited complication following TL affecting 58–72% of patients [7, 8]. Over one-third of patients cite dysphagia as the most significant issue affecting their day to day life following TL [9]. Rates of dysphagia appear similar between patients who undergo primary TL and salvage TL [4, 10]. Causes of dysphagia following TL include a diverticulum, a pseudoepiglottis, cricopharyngeal dysfunction and strictures; factors that can be impacted by the pharyngeal closure technique [8]. Despite dysphagia having a significant impact on patients’ QOL following TL, the factors that impact patients’ ability to swallow following TL remain understudied. In particular, there is very little data to support what method of pharyngeal closure optimises patients’ swallow function following TL. Therefore, the purpose of this study was to assess whether the method of pharyngeal closure influences dysphagia-specific QOL in patients following TL using a validated dysphagia index for head and neck cancer patients.
Methods and materials
Study protocol
Following local institutional ethical approval, we performed a single-centre retrospective analysis of patients who have undergone TL with or without flap reconstruction between September 2014 and December 2019. Eligible patients were identified using operating theatre and multidisciplinary meeting records at our institution. Eligible patients were defined as those who had undergone a TL at our institution between September 2014 and December 2019 and patients greater than 18 years old. Both patients who had undergone primary TL and salvage TL were included in this analysis. Exclusion criteria were defined as patients that had simultaneous partial or total glossectomy at time of TL, patients undergoing pharyngo-laryngo-oesophagectomy or the presence of a medical or neurological condition that could affect speech or swallow function.
Patient data was collected from individual patient healthcare records by the authors. Specifically, this included age, sex, smoking history and alcohol history, history of prior head and neck surgery, chemo or radiotherapy, preoperative nutritional state (BMI and albumin), pathological tumour staging as per the AJCC staging and adverse pathological features such as perineural invasion, lymphovascular invasion, extra nodal extension or positive margins. Surgical notes revealed if primary tracheoesophageal puncture was performed and how the surgical defect was reconstructed. Within our institution, it is routine practice to perform flap-assisted closure in patients undergoing salvage TL. This is to reduce the risk of PCF in previously irradiated tissue. Following TL, patients at our institution are made nil by mouth for a minimum period of 7 days and are fed by alternate methods (typically a nasogastric tube placed at time of surgical procedure). After 7 days, all patients undergo videofluoroscopy and may resume oral feeding if a PCF is not present. Patients then undergo an extensive multidisciplinary rehabilitation program in order to maximise their functional outcomes prior to discharge. Postoperative outcomes were divided into surgical outcomes and functional outcomes. Surgical outcomes included length of stay, PCF, vascular complications, donor site morbidity and overall survival at 1 and 5 years. Functional outcomes collected included diet, speech, need for a feeding tube and need for oesophageal dilation.
Patients still alive at the time of the study and more than 12 months removed from date of surgery (to allow patients reach the point of maximal functional improvement) were then invited to complete the MD Anderson Dysphagia Inventory (MDADI) [11]. The MDADI is a 20-item questionnaire with each item scored on a 5-point Likert scale (strongly disagree, disagree, no opinion, agree, strongly agree). It has been validated to assess dysphagia-specific QOL in head and neck cancer patients and provides a score between 20 (severe dysphagia) and 100 (no dysphagia) on an emotional, functional and physical subscale as well as a global score. The emotional, functional and physical subscales are then combined to form a composite MDADI score [11].
Statistical analysis
Included patients were divided into 3 groups for statistical analysis depending on the pharyngeal closure technique used at TL. These groups were defined as PC, Primary Closure with PMMF overlay and FF (either using a RFFF or an ALT flap). All 27 patients were included when comparing group characteristics, surgical morbidity and functional outcomes. Chi-squared (categorical data) and the Kruskal–Wallis (numerical data) tests were used to assess data between all 3 groups. Fischer’s exact test compared donor site morbidity between the PMMF and FF groups. Five-year survival outcomes were calculated using a Kaplan–Meier analysis.
There were 20 patients alive to complete the MDADI at the time of study and of these patients 18 patients completed the MDADI. One patient declined to complete the MDADI while another patient was lost to follow up. As with the overall analysis, they were divided into PC, PMMF and FF groups. Mean scores were reported for each group in the emotional, functional and physical subscales as well as the mean global rating in each group. The emotional, functional and physical scales were combined to form a composite MDADI score. A Kruskal–Wallis test compared all 3 groups at each subscale. A head-to-head analysis of MDADI scores was subsequently performed between each of the groups (PC v PMMF, PC v FF, PMMF v FF). Again, they were compared using the Kruskal–Wallis test. For the purposes of this study, the alpha level for statistical significance was defined as 0.05. Statistical analysis was carried out using SPSS.
Results
Patient characteristics
A total of 27 patients were identified for inclusion in this study. Patient characteristics are displayed in Table 1. Eight patients (30%) underwent PC, 10 patients (37%) had PMMF-assisted closure and 9 patients (33%) underwent FF-assisted closure (5 ALT and 4 RFFF). Twenty-four patients (89%) were male and the mean age at time of surgery was 63 years old (range 41–79 years). No significant differences were observed between the 3 groups in terms of past medical history, comorbidities, nutritional status, tumour staging or additional treatments received. There was no significant difference in adverse pathological features within surgical specimens or mean follow-up duration between groups. Patients in the PC group were significantly more likely to have undergone primary TL (p < 0.001) and more likely to have received adjuvant therapy (p = 0.003) compared to the PMMF and FF groups.
Surgical morbidity
The median length of hospital stay (LOS) was 29 days (IQR 23–40). The LOS was noted to be lower in the FF group in comparison with the PMMF and PC groups (Table 2). Overall, 3 patients (11%) developed a PCF postoperatively with 1 patient in the PMMF group and 2 patients in the FF group. All patients who developed PCF postoperatively had undergone salvage TL following previous chemoradiotherapy. One patient developed a postoperative wound infection at the laryngeal surgical site which was managed with antibiotics. No significant differences were observed between groups in terms of need for surgical wound or flap revision. One patient in the PMMF group had wound breakdown at the donor site. No donor site morbidities were observed in the FF group. Overall survival was lowest in the PMMF group at 1 year and 5 years but this did not reach significance.
Functional outcomes
Patients in the PMMF and FF groups were more likely to have had a prolonged period of feeding tube dependence postoperatively but this did not reach statistical significance (12% (PC) v 40% (PMMF) v 33% (FF); p = 0.43). A higher proportion of patients in the PMMF (50%) group required oesophageal dilation during the study period. One patient within the PMMF group has undergone oesophageal dilation 8 times following TL. The majority of patients within the study achieved speech following TL (93%) while 38% of patients have no dietary restrictions following TL (Table 3).
Dysphagia-specific quality of life outcomes
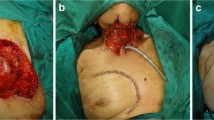
Dysphagia-specific QOL outcomes (Fig. 1) were measured for 18 patients who completed the MDADI. Of these 18 patients, 6 were part of the PC group, 5 the PMMF group and 7 from the FF group. Mean scores for each group were calculated within each MDADI subscale. The FF group scored consistently better across all 4 subscales (Table 4) and this achieved significance within the functional subscale (59.3 (PC) v 54.4 (PMMF) v 81.1 (FF); p = 0.04). The mean emotional subscale scores were 54.4 v 53.3 v 81.1 (p = 0.1) for the PC, PMMF and FF groups, respectively. On the physical subscale, the mean scores were 55.0 (PC) v 55.5 (PMMF) v 72.5 (FF) (p = 0.06) and with regard to the global rating, each group scored 50.0 (PC) v 48.0 (PMMF) v 80.0 (FF) (p = 0.06), respectively. Composite MDADI scores were 55.3 v 54.5 v 75.5 (p = 0.07) for the PC, PMMF and FF groups, respectively.
A head-to-head analysis was subsequently performed between groups (Table 5). The PC and PMMF groups scored similarly in all subscales with no significant differences between groups. When comparing the PC and FF groups, the FF group scored higher in all MDADI subscales. This reached statistical significance within the functional (58.3 v 81.1; p = 0.04), physical (55.0 v 72.5; p = 0.04) and global (50.0 v 80.0; p = 0.04) subscales. When comparing the PMMF and FF groups, the FF group again scored higher across all MDADI subscales. This reached statistical significance in the functional subscale (54.4 v 81.1; p = 0.04) and approached statistical significance in all other subscales. Within the FF group, specifically no significant differences were noted between the ALT and the RFFF groups.
Discussion
The most significant finding of this study is the demonstrated improvement in dysphagia-specific QOL associated with FF closure following TL using a validated dysphagia index. This reached significance in the MDADI functional subscale while approaching significance in all other subscales as well as the composite score. To the best of our knowledge, only one other study has compared dysphagia-related outcomes by pharyngeal closure technique using a validated dysphagia index [10]. Harris et al. used the EAT-10 questionnaire and in contrast to the present study, they found no significant difference in EAT-10 scores between PC, PMMF and FF pharyngeal closure [10]. Other previous studies have compared patients by self-reported dysphagia or alternative measures of dysphagia such as diet consistency, feeding tube dependence or need for oesophageal dilation. Nguyen et al. performed a retrospective analysis among 126 patients who have undergone salvage TL [12]. They found patients in the FF reconstruction group to be significantly less likely to require a modified diet compared with the PMMF group (15% v 39%; p < 0.05). The FF group was also less likely to need a chronic feeding tube and less likely to require oesophageal dilation but this did not reach statistical significance [12]. In a separate study, patients who underwent pharyngeal closure augmented by tissue containing muscle were noted to achieve worse swallowing outcomes compared with primary closure and tissue without muscle [13]. Our analysis using the MDADI was consistent with these findings. We showed that patients who had undergone FF-assisted pharyngeal closure scored consistently higher overall and among various subscales within the MDADI when compared with the PC and PMMF groups. Thus, our findings further support the use of FF pharyngeal closure over PC or PMMF following salvage TL in order to optimise patients’ swallow function and dysphagia-specific QOL.
Our study demonstrated a low overall rate of PCF development (11%) in comparison to rates between 15 and 65% reported within the literature [14,15,16]. It is widely accepted that both PMMF and FF pharyngeal closure methods are associated with reduced incidence of PCF following salvage TL [13, 17, 18]. However, it is unclear within the literature whether PMMF or FF reconstruction is superior for preventing PCF following salvage TL with studies demonstrating contrasting results [17, 18]. It is routine practice in our institution to perform flap-assisted closure in patients undergoing salvage TL to reduce the risk of a PCF in previously irradiated tissue. This was reflected in the study groups with the entire PC group undergoing primary TL (with presumed healthy, well-vascularised tissue) while the majority of patients in the PMMF (90%) and FF (78%) groups underwent salvage TL following previous radiotherapy (RT) or chemoradiotherapy (CRT). When comparing the flap-assisted closure techniques, PMMF reconstruction has a number of advantages. A PMMF is easy to harvest, it has a low failure rate, there is an abundance of tissue harvested and PMMF can be performed by a surgeon not trained in microvascular surgery [18]. However, PMMF has a number of drawbacks: it leaves a bulky lateral neck bulge, range of motion at the shoulder is reduced and it is not pliable to the surgical defect [19]. FF on the other hand is readily pliable to the surgical defect, less bulky and associated with reduced aesthetic and functional morbidity in comparison to PMMF. The need for a surgeon trained in microvascular surgery limits the widespread use of FF closure techniques. Some authors have also pointed to increased operative time and thus costs associated with FF closure methods when compared to PMMF closure following TL [12]. However, operating times within our institution are similar whether FF closure or PMMF closure is used as we perform a simultaneous FF harvest and tumour extraction during TL. In comparison during TL, a PMMF flap cannot be harvested until tumour extraction is complete due to a lack of space at the operating site. We have found the time taken for microvascular anastomosis for a FF similar to the time taken for PMMF harvest and placement. Within our institution prior to the results of this study, the decision to perform PMMF or FF closure was decided at our head and neck multidisciplinary meeting taking into account individual patient factors and in particular the expected surgical defect size following tumour extraction (FF closure often being reserved for larger surgical defects). However, the results of this study coupled with similar operating times have led to a shift in our institutional approach to reconstruction of these surgical defects. FF closure is now the standard practice in our institution following salvage TL and primary TL if augmented tissue closure is required.
The 81% 1-year survival among our group was similar to rates demonstrated in previous studies while the 76% 5-year survival was improved in comparison to previous studies [4, 20]. Overall rates of surgical complications such as wound infection and wound revision (4% and 15%, respectively) were in keeping with previous studies and in our study, no significant differences were detected between groups [21, 22]. Interestingly we observed that median inpatient LOS was reduced among the FF group. Not only does reduced LOS have economic benefits with reduced healthcare-associated costs but it also may reflect an improved postoperative recovery among this cohort.
The need for oesophageal dilation is indicative of poor swallowing outcomes following TL. Seven patients (26%) within this study required oesophageal dilation following TL which is similar to rates in other series (22.8–29.2%) [23, 24]. We observed that a higher proportion of patients within the PMMF group required oesophageal dilation, a finding also observed by Nguyen et al. [12]. PMMF closure is effective in reducing PCF rates following salvage TL as it supports less healthy previously irradiated tissue which is often tightly opposed. However, following TL, a PMMF is used as an overlay flap and therefore, it does not increase neopharyngeal diameter. This may explain why it has been noted to be associated with an increased need for oesophageal dilation following TL. Oesophageal dilation can be an effective procedure for patients with neopharyngeal strictures following TL and dilation significantly improves dysphagia following TL in this cohort [25]. However, oesophageal dilation exposes the patient to general anaesthesia and the risk of oesophageal perforation. The benefit associated with oesophageal dilation is often temporary. A significant proportion of patients require repeat oesophageal dilation with 43% of patients who undergo oesophageal dilation once requiring the procedure on more than 3 occasions [23]. This means these patients often undergo repeat exposure to the risks associated with general anaesthesia, the risk of oesophageal perforation and incurring significant healthcare-associated costs both to the patient and hospitals. This again supports the usage of FF pharyngeal closure of PMMF following TL.
The present study has a number of limitations. First is the small study population which may lead to type 2 statistical errors. The small sample size was limited by two factors. Patients were limited to those operated on after 2014 as FF reconstruction was not performed prior to this within our institution. There has also been a marked reduction in the number of TL performed in the “chemoradiotherapy era” since publication of the VA Larynx and RTOG 91-11 trials with laryngeal preservation strategies now preferred when possible [2, 3]. Another limitation of the present study is its retrospective design which may lead to selection bias. Patients in the PC group were more likely to have undergone primary TL (with assumed healthy not previously irradiated tissue) which makes comparisons with the PMMF and FF groups challenging. The groups however were otherwise similar in all aspects. All but one patient in the PC group had additional treatment following surgery (either radiotherapy or chemoradiotherapy). Despite these limitations, this study is one of the first to evaluate dysphagia-specific QOL in patients following TL comparing patients by pharyngeal closure technique. Patient characteristics and outcomes were similar to rates observed within the literature making comparisons with the present literature and follow-up studies possible.
Conclusions
Our study demonstrated that superior dysphagia-specific QOL was associated with FF pharyngeal closure when compared with PC and PMMF pharyngeal closure following TL using a validated dysphagia-specific QOL measure. Inpatient LOS was observed to be lower among the FF group while operating time is not increased when performing a FF compared with PMMF within our institution. Morbidity and other functional outcomes between the 3 groups did not differ significantly. These findings suggest that with the availability of a surgeon trained in microvascular surgery FF pharyngeal closure following salvage TL should be recommended over PMMF for its clear benefit on dysphagia-specific QOL, reduced inpatient LOS and the lack of increased operating time. As a result, FF pharyngeal closure is now the standard practice within our institution following salvage TL.
Change history
17 August 2022
Missing Open Access funding information has been added in the Funding Note.
References
Howlader NNA, Krapcho M (2020) SEER cancer statistics review, 1975–2017. National Cancer Institute, Bethesda. https://seer.cancer.gov/csr/1975_2017/. Accessed 13 Mar 2021
Department of Veterans Affairs Laryngeal Cancer Study G, Wolf GT, Fisher SG, Hong WK, Hillman R, Spaulding M, Laramore GE, Endicott JW, McClatchey K, Henderson WG (1991) Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N Engl J Med 324(24):1685–1690
Forastiere AA, Goepfert H, Maor M, Pajak TF, Weber R, Morrison W, Glisson B, Trotti A, Ridge JA, Chao C, Peters G, Lee DJ, Leaf A, Ensley J, Cooper J (2003) Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med 349(22):2091–2098
Sullivan CB, Ostedgaard KL, Al-Qurayshi Z, Pagedar NA, Sperry SM (2020) Primary laryngectomy versus salvage laryngectomy: a comparison of outcomes in the chemoradiation era. Laryngoscope 130(9):2179–2185
Akali NR, Jaya AC, Balasubramanian D, Iyer S, Thankappan K (2021) Islanded facial artery musculo-mucosal flap for partial pharyngeal defect reconstruction after total laryngectomy: case report. Head Neck 43(1):E1–E6
Molteni G, Gazzini L, Sacchetto A, Nocini R, Marchioni D (2021) Role of the temporoparietal fascia free flap in salvage total laryngectomy. Head Neck 43(5):1692–1694
Ward EC, Bishop B, Frisby J, Stevens M (2002) Swallowing outcomes following laryngectomy and pharyngolaryngectomy. Arch Otolaryngol Head Neck Surg 128(2):181–186
Maclean J, Cotton S, Perry A (2009) Post-laryngectomy: it’s hard to swallow: an Australian study of prevalence and self-reports of swallowing function after a total laryngectomy. Dysphagia 24(2):172–179
Robertson SM, Yeo JC, Dunnet C, Young D, Mackenzie K (2012) Voice, swallowing, and quality of life after total laryngectomy: results of the west of Scotland laryngectomy audit. Head Neck 34(1):59–65
Harris BN, Hoshal SG, Evangelista L, Kuhn M (2020) Reconstruction technique following total laryngectomy affects swallowing outcomes. Laryngoscope Investig Otolaryngol 5(4):703–707
Chen AY, Frankowski R, Bishop-Leone J, Hebert T, Leyk S, Lewin J, Goepfert H (2001) The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M. D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg 127(7):870–876
Nguyen S, Thuot F (2017) Functional outcomes of fasciocutaneous free flap and pectoralis major flap for salvage total laryngectomy. Head Neck 39(9):1797–1805
Microvascular Committee of the American Academy of Otolaryngology-Head and Neck Surgery (2019) Salvage laryngectomy and laryngopharyngectomy: multicenter review of outcomes associated with a reconstructive approach. Head Neck 41(1):16–29
Virtaniemi JA, Kumpulainen EJ, Hirvikoski PP, Johansson RT, Kosma VM (2001) The incidence and etiology of postlaryngectomy pharyngocutaneous fistulae. Head Neck 23(1):29–33
Paydarfar JA, Birkmeyer NJ (2006) Complications in head and neck surgery: a meta-analysis of postlaryngectomy pharyngocutaneous fistula. Arch Otolaryngol Head Neck Surg 132(1):67–72
Gendreau-Lefevre AK, Audet N, Maltais S, Thuot F (2015) Prophylactic pectoralis major muscle flap in prevention of pharyngocutaneous fistula in total laryngectomy after radiotherapy. Head Neck 37(9):1233–1238
Patel UA, Moore BA, Wax M, Rosenthal E, Sweeny L, Militsakh ON, Califano JA, Lin AC, Hasney CP, Butcher RB, Flohr J, Arnaoutakis D, Huddle M, Richmon JD (2013) Impact of pharyngeal closure technique on fistula after salvage laryngectomy. JAMA Otolaryngol Head Neck Surg 139(11):1156–1162
Chao JW, Spector JA, Taylor EM, Otterburn DM, Kutler DI, Caruana SM, Rohde CH (2015) Pectoralis major myocutaneous flap versus free fasciocutaneous flap for reconstruction of partial hypopharyngeal defects: what should we be doing? J Reconstr Microsurg 31(3):198–204
Moukarbel RV, Fung K, Franklin JH, Leung A, Rastogi R, Anderson CM, Yoo JH (2010) Neck and shoulder disability following reconstruction with the pectoralis major pedicled flap. Laryngoscope 120(6):1129–1134
Fowler BZ, Muller S, Chen AY, Johnstone PA (2006) Factors influencing long-term survival following salvage total laryngectomy after initial radiotherapy or conservative surgery. Head Neck 28(2):99–106
Fung K, Teknos TN, Vandenberg CD, Lyden TH, Bradford CR, Hogikyan ND, Kim J, Prince ME, Wolf GT, Chepeha DB (2007) Prevention of wound complications following salvage laryngectomy using free vascularized tissue. Head Neck 29(5):425–430
Boukovalas S, Goepfert RP, Smith JM et al (2020) Association between postoperative complications and long-term oncologic outcomes following total laryngectomy: 10-year experience at MD Anderson Cancer Center. Cancer 126(22):4905–4916
Petersen JF, Pezier TF, van Dieren JM et al (2019) Dilation after laryngectomy: incidence, risk factors and complications. Oral Oncol 91:107–112
Schuman AD, Birkeland AC, Farlow JL et al (2021) Predictors of stricture and swallowing function following salvage laryngectomy. Laryngoscope 131(6):1229–1234
Wu PI, Szczesniak MM, Maclean J, Graham PH, Quon H, Choo L, Cook IJ (2019) Endoscopic dilatation improves long-term dysphagia following head and neck cancer therapies: a randomized control trial. Dis Esophagus 32(6)
Funding
Open Access funding provided by the IReL Consortium.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All of the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Local institutional ethical approval was obtained from the Beaumont Hospital Research and Ethics committee (REC REF 20/31).
Conflict of interest
Eoin F. Cleere, Sherif Mamdouh, Emma Devoy-Flood, Marie-Therese O’Callaghan, Fiachra Martin, John B. O’Sullivan, Neville Shine and James P. O’Neill declare no competing interests.
Informed consent
Informed consent was obtained from study participants.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cleere, E.F., Mamdouh, S., Devoy-Flood, E. et al. Free Flap microvascular pharyngeal closure results in improved dysphagia-specific quality of life following total laryngectomy. Eur J Plast Surg 45, 399–407 (2022). https://doi.org/10.1007/s00238-021-01893-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-021-01893-3