Abstract
Background
The Poly Implant Prothèse (PIP) implants were withdrawn from the market in 2010 due to the use of low-grade silicone, causing a high risk for implant rupture. The aim of this study was to investigate the implant dynamics of PIP breast implants, as well as to determine the rate and predictors of implant gel bleeding, rupture, and capsular contracture in PIP implants.
Methods
Eighty women with a total of 152 PIP implants who underwent a reoperation in 2012 were enrolled in this study. Physical investigation included assessing the Baker score and demographics were retrospectively traced in medical records. The pre- and post-operative volumes of the implants were calculated and their state was determined intraoperatively by the surgeon.
Results
The implants were removed after a mean implant duration of 11 ± 2.1 years. Gel bleed and implant rupture occurred in respectively 42 and 25% of the implants. Intact implants had post-operative volume increase as well as decrease. There was a correlation between gel bleeding and more post-operative implant volume increase (P ≤ 0.05). Capsular contracture had a protective effect against post-operative implant volume increase (P ≤ 0.05), while a post-operative implant volume increase provided a protective influence in developing capsular contracture (P ≤ 0.05). Additionally, implant rupture led to a higher risk of capsular contracture (P ≤ 0.05).
Conclusions
We managed to illustrate that PIP implant shells were too permeable and that there is a correlation between gel bleeding and the increase of the post-operative implant volume. Implant rupture led to a higher risk for developing capsular contracture.
Level of evidence: Level III, risk / prognostic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2007, the quality of the silicone breast implants manufactured by Poly Implant Prothèse (PIP) was put into question, as physicians started reporting higher rupture rates among patients that were treated with PIP branded implants [1, 2]. It was not until 2010 that the French Medical Regulatory Authority (ANSM) declared that silicone breast implants manufactured by PIP were illegally authorized [3]. As a consequence, medical use of the PIP implants was prohibited in several European countries, including the Netherlands. Moreover, the Dutch Health Care Inspectorate (IGZ) recommended institutions to have these implants removed from the patients.
Several studies have reported on the chemical and physiochemical properties of PIP implants. The ANSM found that the implants contained low-grade silicone gel and shells, so patients who underwent breast surgery using PIP implants in the past were at a higher risk of an implant shell rupture [3]. Additional tests conducted in 2012 by a British NHS Expert Group determined high levels of low molecular weight cyclic siloxanes (D4–6) in PIP silicone gel, but found that these siloxanes did not have cytotoxic or genotoxic effects on the body [4]. Other studies demonstrated that the shell barrier which should have prevented the implant from bleeding was missing [5, 6]. However, the full effect of the chemical and physiochemical properties of implants on the implant dynamics (e.g., shell permeability, gel bleed, and gel rupture) is unknown.
Capsular contracture is the most common complication after breast implant implantation [7,8,9,10]. It occurs in 4–17% of esthetic or reconstructive patients that have undergone breast surgery [11]. Symptoms include hardening, pain, and deformation of the breast. As a tool to assess the grade of capsular contracture after palpating the breast, clinicians use the Baker score, illustrated in Table 1 [12]. It is unclear what exactly causes capsular contracture; some hypothesize that a biofilm created after a subclinical bacterial infection stimulates this contraction [13,14,15,16], while others think an immunologic response is the source [17, 18]. The leakage of silicone gel has also been associated with contraction of the capsule, whether through rupture or gel bleeding [19].
To date, few studies have studied the implant dynamics and its relationship with capsular contracture. Therefore, the primary purpose of this study was to assess the implant dynamics of PIP breast implants and the risk factors related to these implant dynamics. The second purpose of this study was to analyze the rate and predictors for developing capsular contracture in PIP implants.
Materials and methods
Subjects
In 2012, patients that underwent breast augmentation or reconstruction with PIP implants at the OLVG Hospital in Amsterdam, the Netherlands, were recalled to the clinic for a reoperation to remove or replace their implants. The measurements of 102 patients with 194 breast augmentations and reconstructions were reported. This study includes a consecutive cohort of patients that underwent a reoperation between March 2012 and September 2012 for removal or replacement of their breast implants.
Patients who received breast implants other than PIP were excluded (n = 35 breasts), as they were reoperated for other indications than high risk of rupture. For our analysis, we also excluded patients that primarily underwent breast reconstruction, as they constituted a minority within the sample (n = 7) and tended to have a higher chance of developing complications compared to breast augmentations [20]. The final cohort comprised of 80 patients with 152 breast reoperations.
All the women who were recalled were first seen in the outpatient clinic, where they underwent physical examination of the breast and axillae. Each breast was inspected and palpated and possible axillary lymphomas were noted. The four-grade Baker score was then determined for the first time. In some cases, the physician (re-) assessed the Baker score at the operation room. In the cases where the Baker score was determined at the two aforementioned moments, the most recent score was considered as the final Baker score. A clinical Baker score of 3 or 4 was further considered as capsular contracture in this study.
Patient medical records were manually reviewed for patient demographics, surgery-related information, and implant characteristics.
Implant characteristics
As soon as the implants were surgically removed, their integrity was recorded either as intact, gel bleeding, or ruptured. Implants were considered intact when no tears were found in the shell. Gel bleeding was reported when the shell was intact but a surrounding substance that stuck to the glove of the surgeon was apparent. Ruptured implants had holes or tears in the shell. All implants were immediately put on a digital weighing scale providing the post-operative mass (in grams (gr)). When the implants were ruptured, as much as possible of the implant substance was measured. This measuring procedure was attempted in a similar step-by-step manner by briefed theater nurses. When silicone lymphomas (siliconomas) were found during the operation, they were removed by the surgeon and sent for pathologic evaluation.
Implant volume versus mass
All the breast implants display their (pre-operative) volume information on the package, rather than the mass. As we did not know the pre-operative mass of the implants and could not contact the manufacturer of PIP in order to know the density of the silicone, we measured the density of an unused PIP implant with the help of the Dutch National Institute for Public Health and the Environment (RIVM). Using the water displacement method with measuring containers of adequate circumference, the density was found to be 0.975 g/ml, which we used to convert the post-operative mass to volume. This converted volume was used in the analyses.
Statistical analysis
The object of investigation was both the woman and the breast. Statistical analysis was done per breast. As most patients were operated on both breasts, the usual random effect that an unselected group of individual study objects should provide was not achieved as when using the breasts for analyses. We tested this with the use of Intra-class Coefficient Correlation tests. In order to correct this variance, multi-leveled tests were used for univariate as well as for multivariate analyses. For the nominal outcomes, a generalized linear mixed model test was used. For the dichotomous outcomes, we used the generalized estimating equations (GEE) test. Multivariable logistic regression analysis was done for all clinically relevant factors, as illustrated in the respective tables. We corrected for variables which could be possible confounders. These were the patient-related characteristics: age, body mass index, alcohol drinking, and years between operations. As, overall, this did not lead to relevant changes in the results, these outcomes are not portrayed in the tables.
Results were reported as odds ratios (OR) with 95% confidence intervals (CI) and P values. A two-tailed P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS® 22 (SPSS, Inc., Illinois, USA).
Results
The mean age of the 80 patients at the time of explantation was 53 ± 12 years. The mean body mass index was 24 ± 4.5 kg/m2 which falls under the category of normal weight. There were 41% smokers and 58% reported alcohol intake. Breast sides were almost equally divided, with 51% having had a breast implant on the left side of the body. The bra size could not be used for further analyses as there was not enough variable data for the tests. Breast implants were implanted for a mean of 11 ± 2.1 years. The majority of the patients did not have capsular contracture. Baker scores were 1 in 58%, 2 in 28%, 3 in 8.3%, and 4 in 5.3%. Table 2 summarizes these patient characteristics. There were two patients that developed siliconomas, which was too small a number to use in further analyses.
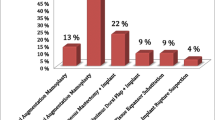
The PIP implants were all round and textured. Post-operative measurements showed a decrease in volume in 19% of the implants and an increase in 62%. In 19% of the implants, there was no change in the post-operative volume. There was a well-divided group regarding post-operative implant state, with 33% intact, 42% with gel bleeding, and 25% ruptured (Table 3). Of the 18 breasts that developed capsular contracture, 39% had intact implants, 22% gel bleed, and 39% ruptured.
Figure 1 in the supplementary file shows a graphical portrayal of the post-operative implant volume differences, separated per implant state group. Besides a few outliers, it is of interest to note an increase in implant volume in both intact and gel bleeding implants.
In the implant-related outcomes, it was not relevant or statistically possible to analyze the relationships between the ruptured implant variable and the post-operative implant volume, as the post-operative implant volume of ruptured implants logically only had a decrease in volume.
The associations resulting in a post-operative volume decrease or increase are portrayed in Table 4. Capsular contracture resulted in a lower risk of post-operative implant volume increase (OR = 0.15 CI = 0.036–0.59, P ≤ 0.05). There appears to be a significant association between bigger implant sizes and post-operative volume differences. As the OR is close to 1.0 for both post-operative implant volume decrease (OR = 1.02 CI = 1.01–1.03, P ≤ 0.05), as well as for post-operative implant volume increase (OR = 1.02 CI = 1.02–1.03, P ≤ 0.05), this association is not valid enough to have meaningful conclusions. When gel bleed was found as the post-operative implant state, there was a higher chance of developing an increased post-operative implant volume. In univariate analysis, the OR was 4.3 with CI = 1.5–13, (P ≤ 0.05), showing an apparent higher risk.
Table 5 shows the analysis for the outcome of the post-operative implant state. For implants with a post-operative increase in volume, there is a 3.4 higher risk for developing gel bleed, with OR of 3.4 (CI = 1.4–8.3, P ≤0.05).
The associations related to capsular contracture can be found in Table 6. Post-operative implant shell rupture led to a higher chance of capsular contracture with an OR of 1.8 (CI = 1.01–3.1, P = 0.044). An increased post-operative implant volume was related to a lower risk of developing capsular contracture with an OR of 0.23 (CI = 0.081–0.63, P ≤ 0.05).
Discussion
The primary aim of this study was to assess the implant dynamics of PIP breast implants and the risk factors related to these implant dynamics. The second purpose of this study was to analyze the rate and predictors for developing capsular contracture in PIP implants. This study shows that the PIP implant shell was highly permeable, leading to an increase or decrease in volume of the implant over the years. Capsular contracture and post-operative implant volume increase had a preventative effect on each other. Gel bleeding related to more implant volume increase and the other way around. Finally, the rupturing of implants led to higher capsular contracture rates.
Capsular contracture poses a protective risk (OR = 0.15, P ≤ 0.05) against a post-operative implant volume increase. A possible explanation is that the capsule surrounding the breast implant grows thicker and loses elasticity. Therefore, there is no space for the implant to expand.
Gel bleeding demonstrated a 4.3 (P ≤ 0.05) higher risk of increase in post-operative implant volume. Since the definition of gel bleeding is the diffusion of silicone out of the intact implant shell, it is striking that no relation was found between gel bleeding and post-operative implant volume decrease, as one would expect that the exuding of silicone could make the implant lighter. This finding backs the statement that the PIP implant shells were too permeable. Beretta et al. [21] studied the (physico)chemical properties of PIP silicone, comparing it with silicone from a McGhan implant model. They concluded that the silicone used by PIP was low-cohesive because of the method used to manufacture the chemicals, where polymers were not properly cross-linked. They proved that this silicone gel could adsorb substances like cholesterol from surrounding tissue, which could in turn lead to a lower viscosity and eventually higher risk of rupture. In a subsequent study, Beretta et al. [22] analyzed the biochemical structure of accumulated fluid around PIP implants. They showed that low and high molecular weight silicone can diffuse not only out of the implant shell but also out of the capsule formed around the implant and into the body. They also managed to illustrate that, besides cholesterol, other endogenous substances like uric acid, globulins, and albumin could enter the implant shell. They hypothesized that this diffusion occurs because of the osmotic power present and might be responsible for the increase in volume despite the gel bleed. Swarts et al. [5] also reported a higher risk of implant rupture due to lack of impermeability. PIP implant shells were proven to have been manufactured with inconstant degrees of thickness, sharp edges, and miniature holes in the hollow parts of textured shells. Additionally, the anti-bleeding barrier layer that is customarily fabricated in modern implants appeared to not have been included in the PIP implant model since 2007 [5].
The previous finding is strengthened, since a post-operative implant volume increase seems to lead to a 3.4 (P ≤ 0.05) higher risk of developing gel bleeding. If we hypothesize that the implant volume increased before the start of gel bleeding, one could argue that a larger content in the implant shell leads to a higher mechanical pressure and eventually leakage of silicone into the surrounding tissue. In the case that this process does not occur in that strict order, it is still very apparent that the PIP implant shell worked as an unsuitable protective layer that lets fluid through in both directions.
Regarding risks for developing capsular contracture, ruptured implants at explantation were associated with an OR of 1.8 (P ≤ 0.05). Studies by Feng et al. [23] and Holmich et al. [24] found similar risks. The large amount of silicone that is released after rupture could be a stimulus of the process of contracture. Alternatively, it could also be the effect of the mechanical changes of the ruptured implant that in turn cause friction with the surrounding tissue, leading to the formation of fibrous tissue. The opposite is also possible, namely, that capsular contracture leads to the rupturing of implants because of a higher mechanical pressure on them. Our cohort showed a rupture rate of 25%, which is comparable with the literature that reported a wide range of 3.9 to 31.6% [25,26,27,28,29,30,31,32]. Breasts that developed capsular contracture contained ruptured implants in 33% of the cases, which was not increased in comparison to intact (39%) and gel bleeding (22%) implants.
Additionally, post-operative implant volume increase seems to have a protective effect (OR = 0.23, P ≤ 0.05) against capsular contracture. Again, the capsular contracture surrounding the implant could prevent any possible expansion of the implant, because the contracted capsules tend to tighten around it. Since it is not possible to determine which phenomenon develops first, this outcome can, in the least, be interpreted as there being a clear association between the two variables.
The results of our study point towards the fact that PIP implant shells indeed lacked adequate impermeability and thus were prone to develop a change in post-operative implant volumes. This, in combination with low-quality silicone gel, provides a high risk for rupture and, thus, a higher probability for developing capsular contracture.
In evaluation of our study, we acknowledge that our study was conducted on a targeted group of patients following the PIP incident. What can be perceived as a limitation is the fact that these implants have been banned from use. However, due to the consequences of the PIP breast implant scandal and the high explantation rate, there have been many studies published on different aspects of this particular breast implant. This provides us with the opportunity to relate the different aspects to factors that influence shell rupture, gel bleeding, and capsular contracture, all of which are complications regularly occurring in patients with new models of breast implants. If we can compare these factors in the PIP implants, and compare the identified factors with breast implants that are currently being used, we will be able to better understand the causes for these complications. One major limitation that this scenario offers is the lack of a control group. Comparison of our data with other brands of implants could have provided a more clinically relevant outcome for our analyses. Furthermore, there appeared to be three different batches of silicone used in the implants throughout the years. The PIP silicone used to measure density was of the PIP2 batch, while the PIP implants of our cohort were predominantly from the PIP1 or NUSIL batch [33]. Although this density was the closest way of determining the post-operative volume, it might not be completely applicable to every PIP implant model used, as there is no traceable record of the component of different batches.
With a cohort of this size and the retrospective design of this study, a conclusion can be limited due to a high chance of bias, loss of data, or confounding factors. Missing data was considered random, since the investigators who collected the data were independent from the involved physicians in the patient care and only used data accessible in patient files. Also, this led to different sizes of variable groups, which made multivariable statistical analysis less reliable. A considerable advantage of our group was the follow-up time of 11 ± 2.1 years, which is a clinically satisfactory amount of time of implantation to observe the impact implants can have on the body and vice-versa. This study set-up was, to our knowledge, the first of its kind, measuring the post-operative implant volume difference in a cohort of this size and relating it to the post-operative implant state and development of capsular contracture.
In conclusion, we illustrated that the elastomer shells of PIP implants were functioning deficiently, since our cohort has shown that volume increase as well as decrease widely occurred. Consequently, there seems to be a correlation between gel bleeding implants and the increasing of the post-operative implant volume. In contrast, capsular contracture could have a protective effect against post-operative implant volume increase, and a post-operative implant volume increase could also provide a protective influence in developing capsular contracture. Additionally, implant ruptures led to a higher probability for capsular contracture. We unquestionably encourage more research on the dynamics of breast implants, particularly with implant models that are currently on the market. We also urge official health institutions to implement stricter guidelines following Hazard Analysis and Critical Control Points (HACCP) to ensure a higher quality of breast implants and thus better patient safety.
References
Berry RB (2007) Rupture of PIP breast implants. J Plast Reconstr Aesthet Surg 60(8):967–968
Lahiri A, Waters R (2006) Locoregional silicone spread after high cohesive gel silicone implant rupture. J Plast Reconstr Aesthet Surg 59(8):885–886
AFSSAPS (2010) Topical report PIP silicone gel pre-filled implants. http://www.ansm.sante.fr/var/ansm_site/storage/original/application/39acdab927235584ccfa340e4a9d3896.pdf. Accessed 20–10, 2016
Keogh SB (2012) Department of Health, NHS medical directorate. Poly Implant Prothese (PIP) breast implants: final report of the expert group 18-06-12.
Swarts E, Kop A, Nilasaroya A, Keogh C, Cooper T (2013) Rupture of poly implant prothèse silicone breast implants: an implant retrieval study. Plast Reconstr Surg 131(4):480e–489e
Keizers P, Vredenbregt M, Bakker F, Kaste D, Venhuis B (2015) Chemical fingerprinting of silicone-based breast implants. J Pharmaceut Biomed 102:340–345
Cunningham B (2007) The mentor core study on silicone MemoryGel breast implants. Plast Reconstr Surg 120(7):19S–29S
U.S. Food and Drug Administration (FDA) (2011) FDA update on the safety of silicone gel-filled breast implants. http://www.fda.gov/downloads/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/BreastImplants/UCM260090.pdf. Accessed 05–11, 2016
Kjøller K, Hölmich L, Jacobsen P et al (2002) Epidemiological investigation of local complications after cosmetic breast implant surgery in Denmark. Ann Plas Surg 48(3):229–237
Spear S, Baker J, Coffee H (1995) Classification of capsular contracture after prosthetic breast reconstruction. Plast Reconstr Surg 96(5):1124
Spear S, Mesbahi A (2007) Implant-based reconstruction. Clin Plast Surg 34(1):63–73
Holmes JD (1989) Capsular contracture after breast reconstruction with tissue expansion. Br J Plast Surg 42(5):591–594
Burkhardt (1988) Capsular contracture: hard breasts, soft data. Clin Plast Surg 15(4):521–532
Virden C, Dobke M, Stein P, Parsons L, Frank D (1992) Subclinical infection of the silicone breast implant surface as a possible cause of capsular contracture. Aesthetic Plast Surg 16(2):173–179
Schreml S, Heine N, Eisenmann-Klein M, Prantl L (2007) Bacterial colonization is of major relevance for high-grade capsular contracture after augmentation mammaplasty. Ann Plas Surg. 59(2):126–130
Potter E, Rohrich R, Bolden K (2013) The role of silicone granulomas in recurrent capsular contracture: a review of the literature and an approach to management. Plast Reconstr Surg 131(6):888e–895e
Wolfram D, Dolores W, Rainer C et al (2004) Cellular and molecular composition of fibrous capsules formed around silicone breast implants with special focus on local immune reactions. J Autoimmun 23(1):81–91
Prantl L, Schreml S, Fichtner-Feigl S, Poppl N, Eisenmann-Klein M, Schwarze H, Fuchtmeier B (2007) Clinical and morphological conditions in capsular contracture formed around silicone breast implants. Plast Reconstr Surg 120(1):275–284
Moyer H, Ghazi B, Losken A (2012) The effect of silicone gel bleed on capsular contracture: a generational study. Plast Reconstr Surg 130(4):793–800
Brown L, Pennello G (2002) Replacement surgery and silicone gel breast implant rupture: self-report by women after mammoplasty. J Women’s Heal Gender-based Medicine 11(3):255–264
Beretta G, Malacco M (2013) Chemical and physicochemical properties of the high cohesive silicone gel from Poly Implant Prothese (PIP) breast prostheses after explantation: a preliminary, comparative analytical investigation. J Pharm Biomed Anal 78:75–82
Beretta G, Richards A, Malacco M (2013) Chemical and biochemical composition of late periprosthetic fluids from women after explantation of ruptured Poly Implant Prothèse (PIP) breast prostheses. J Pharmaceut Biomed. 84:159–167
Feng L-J, Amini S (1999) Analysis of risk factors associated with rupture of silicone gel breast implants. Plast Reconstr Surg 104(4):955–963
Hölmich L, Kjøller K, Fryzek J et al (2003) Self-reported diseases and symptoms by rupture status among unselected Danish women with cosmetic silicone breast implants. Plast Reconstr Surg 111(2):723–732
Maijers M, Niessen F (2012) Prevalence of rupture in Poly Implant Prothèse silicone breast implants, recalled from the European market in 2010. Plast Reconstr Surg 129(6):1372–1378
Aktouf, Auquit-Auckbur, Coquerel-Beghin, Delpierre, Milliez P-Y (2012) Augmentation mammaire par prothèses en gel de silicone de la marque Poly Implant Prothèses (PIP) : étude rétrospective de 99 patientes. Analyse des ruptures et prise en charge. Ann Chir Plast Esthet 57(6):558–566
Crouzet, Gangloff, Chaput, Grolleau J-L, Garrido (2012) Bilan à 18 mois du retrait du marché des prothèses Poly Implant Prothèse. Expérience d’un centre anticancéreux. Ann De Chir Plastique Esthétique. 57(1):9–15
Berry MG, Stanek J (2013) PIP implant biodurability: a post-publicity update. J Plast Reconstr Aesthet Surg 66(9):1174–1181
Chummun S, McLean N (2013) Poly Implant Prothèse (PIP) breast implants: our experience. Surgeon 11(5):241–245
Quaba O, Quaba A (2013) PIP silicone breast implants: rupture rates based on the explantation of 676 implants in a single surgeon series. J Plast Reconstr Aesthet Surg 66(9):1182–1187
Tropet Y, Oulharj S, Pauchot J (2013) PIP breast implants: a series of 217 explants. Bull Acad Natl Med 197(1):123–130 discussion 130–1
Oulharj P (2014) Tropet. PIP breast implant removal: a study of 828 cases. J Plast Reconstr Aesthet Surg 67(3):302–307
Grall JY, Maraninchi D (2012) Etat des lieux de l’ensemble des controles effectuessur la societe Poly implants prothèse (PIP). AFSSAPS, Paris 70
Acknowledgements
We would like to thank Peter Keizers (PhD, National Institute for Public Health and the Environment, Bilthoven, The Netherlands) who offered expert advice on the chemical structure and development of the PIP implants. We would also like to show our gratitude to Martijn Heijmans (PhD, Department of Epidemiology and Biostatistics, VU University Medical Center, Amsterdam, The Netherlands) for his expert advice on statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yara Bachour, Zavira C.M. Heinze, Tobias Dormaar, Gijs van Selms, Marco J.P.F. Ritt, and Frank B. Niessen declare that they have no conflict of interest.
Ethical approval
The local medical ethical committee approved this study (reference number: 14u.113).
Informed consent
For this kind of article, patient consent is not required.
Electronic supplementary material
ESM 1
(DOCX 23 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bachour, Y., Heinze, Z.C.M., Dormaar, T.S. et al. Poly Implant Prothèse silicone breast implants: implant dynamics and capsular contracture. Eur J Plast Surg 41, 563–570 (2018). https://doi.org/10.1007/s00238-018-1427-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-018-1427-y