Abstract
Purpose
To investigate the predictive value of the “soap bubble” sign on molecular subtypes (Group A [PFA] and Group B [PFB]) of posterior fossa ependymomas (PF-EPNs).
Methods
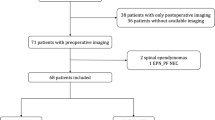
MRI scans of 227 PF-EPNs (internal retrospective discovery set) were evaluated by two independent neuroradiologists to assess the “soap bubble” sign, which was defined as clusters of cysts of various sizes that look like “soap bubbles” on T2-weighted images. Two independent cohorts (external validation set [n = 31] and prospective validation set [n = 27]) were collected to validate the “soap bubble” sign.
Results
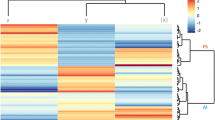
Across three datasets, the “soap bubble” sign was observed in 21 PFB cases (7.4% [21/285] of PF-EPNs and 12.9% [21/163] of PFB); none in PFA. Analysis of the internal retrospective discovery set demonstrated substantial interrater agreement (1st Rating: κ = 0.71 [0.53–0.90], 2nd Rating: κ = 0.83 [0.68–0.98]) and intrarater agreement (Rater 1: κ = 0.73 [0.55–0.91], Rater 2: κ = 0.74 [0.55–0.92]) for the “soap bubble” sign; all 13 cases positive for the “soap bubble” sign were PFB (p = 0.002; positive predictive value [PPV] = 100%, negative predictive value [NPV] = 44%, sensitivity = 10%, specificity = 100%). The findings from the external validation set and the prospective validation set were similar, all cases positive for the “soap bubble” sign were PFB (p < 0.001; PPV = 100%).
Conclusion
The “soap bubble” sign represents a highly specific imaging marker for the PFB molecular subtype of PF-EPNs.



Similar content being viewed by others
Data Availability
Data could be made available to qualified researchers upon reasonable request and agreement of a data-transfer agreement by the corresponding author.
References
Wu J, Armstrong TS, Gilbert MR (2016) Biology and management of ependymomas. Neuro Oncol 18:902–913
Albright AL (1993) Pediatric brain tumors. CA: Cancer J Clin 43:272–288
Larrew T, Saway BF, Lowe SR (2021) Molecular classification and therapeutic targets in ependymoma. Cancers (Basel) 13:6218
Pajtler KW, Witt H, Sill M (2015) Molecular classification of ependymal tumors across all cns compartments, histopathological grades, and age groups. Cancer Cell 27:728–743
Witt H, Mack SC, Ryzhova M (2011) Delineation of two clinically and molecularly distinct subgroups of posterior fossa ependymoma. Cancer Cell 20:143–157
Mack SC, Witt H, Piro RM (2014) Epigenomic alterations define lethal CIMP-positive ependymomas of infancy. Nature 506:445–450
Louis DN, Perry A, Wesseling P (2021) The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol 23:1231–1251
Panwalkar P, Clark J, Ramaswamy V (2017) Immunohistochemical analysis of H3K27me3 demonstrates global reduction in group-A childhood posterior fossa ependymoma and is a powerful predictor of outcome. Acta Neuropathol 134:705–714
Ellison DW, Aldape KD, Capper D (2020) cIMPACT-NOW update 7: advancing the molecular classification of ependymal tumors. Brain Pathol 30:863–866
Zhang M, Wang E, Yecies D (2022) Radiomic signatures of posterior fossa ependymoma: Molecular subgroups and risk profiles. Neuro Oncol 24:986–994
Pajtler KW, Mack SC, Ramaswamy V (2017) The current consensus on the clinical management of intracranial ependymoma and its distinct molecular variants. Acta Neuropathol 133:5–12
Ramaswamy V, Hielscher T, Mack SC (2016) Therapeutic impact of cytoreductive surgery and irradiation of posterior fossa ependymoma in the molecular era: a retrospective multicohort analysis. J Clin Oncol 34:2468–2477
Ruda R, Reifenberger G, Frappaz D (2018) EANO guidelines for the diagnosis and treatment of ependymal tumors. Neuro Oncol 20:445–456
de Sousa GR, Lira RCP, de Almeida MT (2021) A coordinated approach for the assessment of molecular subgroups in pediatric ependymomas using low-cost methods. J Mol Med (Berl) 99:1101–1113
Yonezawa U, Karlowee V, Amatya VJ (2020) Radiology profile as a potential instrument to differentiate between posterior fossa ependymoma (PF-EPN) group A and B. World Neurosurg 140:e320–e327
Ma Z, Yan H, Shi H (2016) The typical and atypical MR imaging findings of central neurocytomas: Report on eighteen cases and review of the literature. Clin Neurol Neurosurg 146:18–23
Li X, Guo L, Sheng S (2018) Diagnostic value of six MRI features for central neurocytoma. Eur Radiol 28:4306–4313
Pajtler KW, Wen J, Sill M (2018) Molecular heterogeneity and CXorf67 alterations in posterior fossa group A (PFA) ependymomas. Acta Neuropathol 136:211–226
Nambirajan A, Sharma A, Rajeshwari M (2021) EZH2 inhibitory protein (EZHIP/Cxorf67) expression correlates strongly with H3K27me3 loss in posterior fossa ependymomas and is mutually exclusive with H3K27M mutations. Brain Tumor Pathol 38:30–40
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Spoto GP, Press GA, Hesselink JR (1990) Intracranial ependymoma and subependymoma: MR manifestations. AJNR Am J Neuroradiol 11:83–91
Ramsahye H, He H, Feng X (2013) Central neurocytoma: radiological and clinico-pathological findings in 18 patients and one additional MRS case. J Neuroradiol 40:101–111
Koeller KK, Sandberg GD, Armed Forces Institute of Pathology (2002) From the archives of the AFIP. Cerebral intraventricular neoplasms: radiologic-pathologic correlation. Radiographics 22:1473–1505
Niiro T, Tokimura H, Hanaya R (2012) MRI findings in patients with central neurocytomas with special reference to differential diagnosis from other ventricular tumours near the foramen of Monro. J Clin Neurosci 19:681–686
Vieira MA, Costa CH, Ribeiro JC (2013) Soap bubble appearance in brain magnetic resonance imaging: cryptococcal meningoencephalitis. Rev Soc Bras Med Trop 46:658–659
Ueda H, Toribe Y, Kuwae Y (2003) An autopsy case of cryptococcal meningoencephalitis: correlation of MRI and pathologic findings. No To Hattatsu 35:499–504
Garcia-Lechuz JM, Sanchez-Conde M, Munoz L (2003) Clinical microbiological case: “soap bubbles” in the cerebellum of an HIV-infected patient. Clin Microbiol Infect 9(419–420):461–412
Taphoorn MJ, Tulleken CA, Jansen GH (1998) A “soap bubble” tumour in the brain: isolated cerebral immunocytoma. J Neurol Neurosurg Psychiatry 65:217
Anvarian Z, Mykytyn K, Mukhopadhyay S (2019) Cellular signalling by primary cilia in development, organ function and disease. Nat Rev Nephrol 15:199–219
Davenport JR, Watts AJ, Roper VC (2007) Disruption of intraflagellar transport in adult mice leads to obesity and slow-onset cystic kidney disease. Curr Biol 17:1586–1594
Nauli SM, Alenghat FJ, Luo Y (2003) Polycystins 1 and 2 mediate mechanosensation in the primary cilium of kidney cells. Nat Genet 33:129–137
Kottgen M, Buchholz B, Garcia-Gonzalez MA (2008) TRPP2 and TRPV4 form a polymodal sensory channel complex. J Cell Biol 182:437–447
Jonassen JA, San Agustin J, Follit JA (2008) Deletion of IFT20 in the mouse kidney causes misorientation of the mitotic spindle and cystic kidney disease. J Cell Biol 183:377–384
Ostrom QT, Cioffi G, Gittleman H (2019) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012–2016. Neuro Oncol 21:v1–v100
Saleh AH, Samuel N, Juraschka K (2022) The biology of ependymomas and emerging novel therapies. Nat Rev Cancer 22:208–222
Acknowledgements
We thank all the staff and patients in the participating centers for their contributions to this study.
Funding
This work was supported by the National Science Foundation of China (Nos. 81870958 and 81571631), the Beijing Municipal Natural Science Foundation for Distinguished Young Scholars (No. JQ20035), the Special Fund of the Pediatric Medical Coordinated Development Center of Beijing Hospitals Authority (No. XTYB201831).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jin, Y., Cheng, D., Duan, Y. et al. “Soap bubble” sign as an imaging marker for posterior fossa ependymoma Group B. Neuroradiology 65, 1707–1714 (2023). https://doi.org/10.1007/s00234-023-03231-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-023-03231-9