Abstract
Purpose
Deep white matter lesions (DWMLs), T2 high-intensity areas in the subcortical white matter on magnetic resonance imaging (MRI), are a clinical phenotype of cerebral small vessel disease. Factors such as age and hypertension have been reported to significantly contribute to the presence and severity of DWMLs in cross-sectional studies. We herein report a 10-year longitudinal study on DWMLs in elderly Japanese subjects to reveal the clinical variables contributing to the progression of DWMLs.
Methods
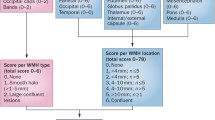
A total of 469 Japanese subjects were invited to participate in the study. Of the participants at baseline, 259 subjects completed the revisit MRI study 10 years later. In those 259 subjects, we evaluated the correlation between the progression of DWMLs and clinical variables, such as the gender, age, and overt vascular risk factors. To clarify the role of hypertension, 200 subjects with grade 1 DWMLs at baseline were categorized into three groups according to their status of hypertension and its treatment.
Results
Of the 200 subjects with grade 1 DWMLs, 47 subjects (23.5%) showed progression of DWMLs (progression group). In the progression group, the percentage of subjects with hypertension and the systolic blood pressure values were higher than in the non-progression group. In addition, subjects ≥ 60 years old at baseline tended to show deterioration of DWMLs in the group with hypertension without antihypertensive treatment.
Conclusion
The results of this 10-year longitudinal study imply a positive correlation between long-standing hypertension and the progression of DWMLs.



Similar content being viewed by others
References
LADIS Study Group (2011) 2001–2011: a decade of the LADIS (Leukoaraiosis And DISability) Study: what have we learned about white matter changes and small-vessel disease? Cerebrovasc Dis 32:577–588. https://doi.org/10.1159/000334498
Poggesi A, Gouw A, van der Flier W, Pracucci G, Chabriat H, Erkinjuntti T, Fazekas F, Ferro JM, Hennerici M, Langhorne P, O’Brien JT, Visser MC, Wahlund LO, Waldemar G, Wallin A, Scheltens P, Inzitari D, Pantoni L (2013) Cerebral white matter changes are associated with abnormalities on neurological examination in non-disabled elderly: the LADIS study. J Neurol 260:1014–1021. https://doi.org/10.1007/s00415-012-6748-3
Poggesi A, Gouw A, van der Flier W, Pracucci G, Chabriat H, Erkinjuntti T, Fazekas F, Ferro JM, Blahak C, Langhorne P, O’Brien J, Schmidt R, Visser MC, Wahlund LO, Waldemar G, Wallin A, Scheltens P, Inzitari D, Pantoni L (2014) Neurological abnormalities predict disability: the LADIS (Leukoaraiosis And DISability) study. J Neurol 261:1160–1169. https://doi.org/10.1007/s00415-014-7332-9
Wardlaw JM, Valdés Hernández MC, Muñoz-Maniega S (2015) What are white matter lesions made of? Relevance to vascular cognitive impairment. J Am Heart Assoc 4:001140. https://doi.org/10.1161/JAHA.114.001140
Masana Y, Motozaki T (2003) Emergence and progress of white matter lesion in brain check-up. Acta Neurol Scand 107:187–194. https://doi.org/10.1034/j.1600-0404.2003.02021.x
Hopkins RO, Beck CJ, Burnett DL, Weaver LK, Victoroff J, Bigler ED (2006) Prevalence of white matter lesions in a young healthy population. J Neuroimaging 16:243–251. https://doi.org/10.1111/j.1552-6569.2006.00047.x
Schmidt R, Fazekas F, Kapeller P, Schmidt H, Hartung HP (1999) MRI white matter hyperintensities: three-year follow-up of the Austrian Stroke Prevention Study. Neurology 53:132–139. https://doi.org/10.1212/wnl.53.1.132
de Leeuw FE, de Groot JC, Achten E, Oudkerk M, Ramos LM, Heijboer R, Hofman A, Jolles J, van Gijn J, Breteler MM (2001) Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study. The Rotterdam Scan Study. J Neurol Neurosurg Psychiatry 70:9–14. https://doi.org/10.1136/jnnp.70.1.9
Kim KW, MacFall JR, Payne ME (2008) Classification of white matter lesions on magnetic resonance imaging in elderly persons. Biol Psychiatry 15(64):273–280
van Dijk EJ, Prins ND, Vrooman HA, Hofman A, Koudstaal PJ, Breteler MMB (2008) Progression of cerebral small vessel disease in relation to risk factors and cognitive consequences: Rotterdam Scan study. Stroke 39:2712–2719. https://doi.org/10.1161/STROKEAHA.107.513176
Firbank MJ, Wiseman RM, Burton EJ, Saxby BK, O’Brien JT, Ford GA (2007) Brain atrophy and white matter hyperintensity change in older adults and relationship to blood pressure. Brain atrophy, WMH change and blood pressure. J Neurol 254:713–721. https://doi.org/10.1007/s00415-006-0238-4
Taylor WD, MacFall JR, Provenzale JM, Payne ME, McQuoid DR, Steffens DC, Krishnan KR (2003) Serial MR imaging of volumes of hyperintense white matter lesions in elderly patients: correlation with vascular risk factors. AJR Am J Roentgenol 181:571–576. https://doi.org/10.2214/ajr.181.2.1810571
Ohshima Y, Mizuno T, Yamada K, Matsumoto S, Nagakane Y, Kondo M, Kuriyama N, Miyazaki T, Takeda K, Nishimura T, Nakagawa M, Ozasa K, Watanabe Y (2013) Low vitamin and carotenoid levels are related to cerebral white matter lesions. J Nutr Health Aging 17:456–460. https://doi.org/10.1007/s12603-012-0419-z
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol 149:351–356. https://doi.org/10.2214/ajr.149.2.351
Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, Culebras A, DeGraba TJ, Gorelick PB, Guyton JR, Hart RG, Howard G, Kelly-Hayes M, Nixon JV, Sacco RL, American Heart Association; American Stroke Association Stroke Council (2006) Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 113:e873–e923. https://doi.org/10.1161/01.STR.0000223048.70103.F1
Tominaga M (2003) Diabetes millitus and HbA1c. Rinsho Byori 51:586–591
Oikawa S (2001) Progress in the treatment of hyperlipemia. The use of various guidelines. Nihon Naika Gakkai Zasshi 90:2003–2009
Nakajima H (2003) Management of hyperuricemia in occupational health: with reference to “guidelines for the management of hyperuricemia and gout”. Sangyo Eiseigaku Zasshi 45:12–19
Henskens LH, Kroon AA, van Oostenbrugge RJ, Gronenschild EH, Hofman PA, Lodder J, de Leeuw PW (2009) Associations of ambulatory blood pressure levels with white matter hyperintensity volumes in hypertensive patients. J Hypertens 27:1446–1452. https://doi.org/10.1097/HJH.0b013e32832b5204
Dufouil C, Chalmers J, Coskun O, Besançon V, Bousser MG, Guillon P, MacMahon S, Mazoyer B, Neal B, Woodward M, Tzourio-Mazoyer N, Tzourio C (2005) PROGRESS MRI Substudy Investigators. Effects of blood pressure lowering on cerebral white matter lesions in patients with stroke: the PROGRESS (Perindopril Protection Against Recurrent Stroke Study) Magnetic Resonance Imaging Substudy. Circulation 112:1644–1650. https://doi.org/10.1161/CIRCULATIONAHA.104.501163
Yamawaki M, Wada-Isoe K, Yamamoto M, Nakashita S, Uemura Y, Takahashi Y, Nakayama T, Nakashima K (2015) Association of cerebral white matter lesions with cognitive function and mood in Japanese elderly people: a population-based study. Brain Behav 5:e00315. https://doi.org/10.1002/brb3.315
Gebeily S, Fares Y, Kordahi M, Khodeir P, Labaki G, Fazekas F (2014) Cerebral white matter lesions (WMH): an analysis of cerebrovascular risk factors in Lebanon. Int J Neurosci 124:799–805. https://doi.org/10.3109/00207454.2014.884087
Veldink JH, Scheltens P, Jonker C, Launer LJ (1998) Progression of cerebral white matter lesions on MRI is related to diastolic blood pressure. Neurology 51:319–320. https://doi.org/10.1212/wnl.51.1.319
Weber R, Weimar C, Blatchford J, Hermansson K, Wanke I, Möller-Hartmann C, Gizewski ER, Forsting M, Demchuk AM, Sacco RL, Saver JL, Warach S, Diener HC, Diehl A, PRoFESS Imaging Substudy Group (2012) Telmisartan on top of antihypertensive treatment does not prevent progression of cerebral white matter lesions in the prevention regimen for effectively avoiding second strokes (PRoFESS) MRI substudy. Stroke 43:2336–2342. https://doi.org/10.1161/STROKEAHA.111.648576
Dong C, Della-Morte D, Rundek T, Wright CB, Elkind MS, Sacco RL (2016) Evidence to maintain the systolic blood pressure treatment threshold at 140 mm Hg for stroke prevention: The Northern Manhattan Study. Hypertension. 67:520–526. https://doi.org/10.1161/HYPERTENSIONAHA.115.06857
Asayama K, Satoh M, Murakami Y, Ohkubo T, Nagasawa SY, Tsuji I, Nakayama T, Okayama A, Miura K, Imai Y, Ueshima H, Okamura T, Evidence for Cardiovascular Prevention From Observational Cohorts in Japan (EPOCH-JAPAN) Research Group (2014) Cardiovascular risk with and without antihypertensive drug treatment in the Japanese general population: participant-level meta-analysis. Hypertension 63:1189–1197. https://doi.org/10.1161/HYPERTENSIONAHA.113.03206
Godin O, Tzourio C, Maillard P, Mazoyer B, Dufouil C (2011) Antihypertensive treatment and change in blood pressure are associated with the progression of white matter lesion volumes: the Three-City (3C)-Dijon Magnetic Resonance Imaging Study. Circulation 123:266–273. https://doi.org/10.1161/CIRCULATIONAHA.110.961052
Goldstein IB, Bartzokis G, Guthrie D, Shapiro D (2005) Ambulatory blood pressure and the brain: a 5-year follow-up. Neurology 64:1846–1852
Gottesman RF, Coresh J, Catellier DJ, Sharrett AR, Rose KM, Coker LH, Shibata DK, Knopman DS, Jack CR, Mosley TH Jr (2010) Blood pressure and white-matter disease progression in a biethnic cohort: Atherosclerosis Risk in Communities (ARIC) study. Stroke 41:3–8. https://doi.org/10.1161/STROKEAHA.109.566992
White WB, Wolfson L, Wakefield DB, Hall CB, Campbell P, Moscufo N, Schmidt J, Kaplan RF, Pearlson G, Guttmann CR (2011) Average daily blood pressure, not office blood pressure, is associated with progression of cerebrovascular disease and cognitive decline in older people. Circulation 124:2312–2319. https://doi.org/10.1161/CIRCULATIONAHA.111.037036
Gouw AA, van der Flier WM, van Straaten EC, Pantoni L, Bastos-Leite AJ, Inzitari D, Erkinjuntti T, Wahlund LO, Ryberg C, Schmidt R, Fazekas F, Scheltens P, Barkhof F, LADIS study group (2008) Reliability and sensitivity of visual scales versus volumetry for evaluating white matter hyperintensity progression. Cerebrovasc Dis 25:247–253. https://doi.org/10.1159/000113863
Fernando MS, O’Brien JT, Perry RH, English P, Forster G, McMeekin W, Slade JY, Golkhar A, Matthews FE, Barber R, Kalaria RN, Ince PG, Neuropathology Group of MRC CFAS (2004) Comparison of the pathology of cerebral white matter with post-mortem magnetic resonance imaging (MRI) in the elderly brain. Neuropathol Appl Neurobiol 30:385–395. https://doi.org/10.1111/j.1365-2990.2004.00550.x
Acknowledgments
The authors thank the members of the Kyoto Industrial Health Association and the Department of Epidemiology for Community Health and Medicine and Neurology, Kyoto Prefectural University of Medicine for their assistance.
Funding
This study was supported by a Grant-in-Aid for scientific research (B) from the Ministry of Education, Science, Sports, Culture and Technology of Japan (No. 14370143) and a Health and Labour Sciences Research Grant of Japan (H28-seishin-ippan-004)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 129 kb)
Rights and permissions
About this article
Cite this article
Tamura, A., Kuriyama, N., Akazawa, K. et al. A 10-year longitudinal study of deep white matter lesions on magnetic resonance imaging. Neuroradiology 63, 1599–1609 (2021). https://doi.org/10.1007/s00234-020-02626-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02626-2