Abstract
Purpose
To assess suspected acute stroke, the computed tomography (CT) protocol contains a non-contrast CT (NCCT), a CT angiography (CTA), and a CT perfusion (CTP). Due to assumably high radiation doses of the complete protocol, the aim of this study is to examine radiation exposure and to establish diagnostic reference levels (DRLs).
Methods
In this retrospective study, dose data of 921 patients with initial CT imaging for suspected acute stroke and dose monitoring with a DICOM header–based tracking and monitoring software were analyzed. Between June 2017 and January 2020, 1655 CT scans were included, which were performed on three different modern multi-slice CT scanners, including 921 NCCT, 465 CTA, and 269 CTP scans. Radiation exposure was reported for CT dose index (CTDIvol) and dose-length product (DLP). DRLs were set at the 75th percentile of dose distribution.
Results
DRLs were assessed for each step (CTDIvol/DLP): NCCT 33.9 mGy/527.8 mGy cm and CTA 13.7 mGy/478.3 mGy cm. Radiation exposure of CTP was invariable and depended on CT device and its protocol settings with CTDIvol 124.9–258.2 mGy and DLP 1852.6–3044.3 mGy cm.
Conclusion
Performing complementary CT techniques such as CTA and CTP for the assessment of acute stroke increases total radiation exposure. Hence, the revised DRLs for the complete protocol are required, where our local DRLs may help as benchmarks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is a frequent cause of disability and death in adults [1] and the etiology of stroke is either ischemic or hemorrhagic [2]. Ischemic stroke accounts for more than 85% of acute strokes and has a high global morbidity and mortality [3, 4]. Due to rapid irreversible damage of tissue, quick and accurate diagnosis is crucial to enable prompt therapy [5, 6].
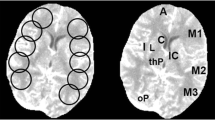
Non-contrast computed tomography (NCCT) of the head is widely recommended as initial imaging modality for suspected acute stroke because it is highly sensitive for depiction of intracranial hemorrhage [7, 8]. Moreover, NCCT can reveal early signs of infarction, although they occur only in a small proportion of patients [8, 9]. Computed tomography angiography (CTA) enables assessment of brain supplying extra- and intracranial vessels and provides additional information about occlusion site and origin of infarction [2, 10, 11]. Computed tomography perfusion (CTP) depicts cerebral hemodynamics and enables evaluation of vessel occlusion found during CTA [12, 13]. Since its establishment in the late 1990s, CTP expanded the value of CT techniques in acute stroke imaging because it detects irreversibly ischemic tissue and enables differentiation between irreversibly infarcted and ischemic but potentially salvageable tissue [2, 6, 14, 15].
A comprehensive CT protocol provides additional information and hereby improves the detection rate of ischemic stroke [2, 9, 16,17,18]. Alongside these benefits, CT is considered a high-dose imaging technique since its establishment and causes the major part of collective effective dose for all radiographic examinations and even increased within the last years [19,20,21,22].
Different national and multinational guidelines were published to limit radiation exposure and state diagnostic reference levels (DRLs) [23]. Hence, to monitor and optimize radiation exposure, standardized dose values need to be registered. The volume-weighted CT dose index (CTDIvol) quantifies the intensity of CT radiation that a patient is exposed to [24, 25]. The dose-length product (DLP) is the product of scan length and CTDIvol and quantifies the total amount of ionizing radiation [26, 27]. Modern CT scanners display and archive technical dose descriptors such as CTDIvol and DLP which are determined in polymethyl methacrylate (PMMA) phantoms of 16 or 32 cm in diameter [28, 29]. Consequently, as CTDIvol and DLP quantify the radiation dose output of a CT scanner, they are appropriate reference parameters. Although they do not directly represent the dose to an individual patient, CTDIvol and DLP might help to ensure lower radiation exposures [30]. To evaluate local radiation exposures, the 75th percentile of dose metric distributions is often used as DRL [31, 32]. Achievable dose (AD) is another useful benchmark and represents the 50th percentile of a distribution of ionizing radiation [32].
The aim of this study was to assess the distribution of radiation exposure of the CT protocol for the assessment of acute stroke and to establish local DRLs.
Material and methods
Patient cohort
Between June 2017 and January 2020, 2897 patients with acute stroke were treated at our center. Thereof, 921 patients who were identified using a DICOM header–based tracking and monitoring software (Radimetrics Enterprise Platform, Bayer Healthcare, Leverkusen, Germany) and who underwent initial CT examination for suspected acute stroke without prior imaging were included in this retrospective study. Dose data comprised 1655 CT scans using a local stroke protocol, consisting of 921 NCCT, 465 CTA, and 269 CTP examinations. Three subgroups could be determined: patients who underwent (I) NCCT solely, (II) NCCT and CTA, and (III) NCCT, CTA, and CTP. Ethical approval for this study was granted by the internal ethical committee of our institution and the requirement to obtain informed consent was waived (20-9175-BO).
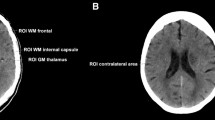
CT protocol and scanner
A standardized local “master” CT protocol for suspected stroke was used including initial NCCT, optional CTA from aortic arch to vertex, and optional CTP of the brain performed as implemented by the vendor. Clinical information and image-based findings were extracted from the report archived in the radiological information system (RIS). All scans were performed at one of three commercially available, modern multi-slice CT scanners: one single-source 128-slice SOMATOM Definition AS+, one dual-source 128-slice SOMATOM Definition Flash, and one dual-source 192-slice SOMATOM Force (all Siemens Healthcare, Forchheim, Germany). Technical settings according to device are shown in Table 1.
Dose assessment
For dose assessment, the commercially available automated dose-tracking software Radimetrics Enterprise Platform based on Monte Carlo simulation techniques was used. Examination data and dose measurements were extracted from this software, which collects radiation exposure metadata and patient demographic information from the Digital Imaging and Communications in Medicine (DICOM) header and from the radiation dose structured report stored in the picture archiving and communication system (PACS) [33]. If dose modulation was used, the CT device took the variation in dose into account when calculating radiation parameters. Topogram- and monitoring-based radiation exposure data were excluded. Dose assessments referred to the 16-cm diameter standard head phantom for NCCT and CTP and to the 32-cm diameter body phantom for CTA.
Statistics and data analysis
Descriptive statistics were performed using the GraphPad Prism 5.01 (GraphPad Software, San Diego, USA). DRLs were set at the 75th percentile and AD at the 50th percentile of dose distribution. To determine normal distribution, Kolmogorov-Smirnov and Shapiro-Wilk-test were applied. The examined variables did not follow normal distribution. The Kruskal-Wallis test with Dunn-Bonferroni post hoc test was applied to compare radiation doses in terms of CTDIvol and DLP at the three different CT scanners. A p-value lower than 0.05 was considered statistically significant.
Results
Patient cohort
In our retrospective study, 921 patients underwent the acute stroke CT protocol at three different multi-slice CT scanners between June 2017 and January 2020. The mean age was 66.7 years ± 16.7 (SD) with a range from 18 to 101 years. About 62% of all examinations were performed at SOMATOM Force, 24.7% at Definition Flash, and 13.3% at Definition AS+ (Tables 2 and 3).
Radiation exposures of each step of the CT protocol
Dose assessment comprised radiation exposure data of 1655 CT scans including 921 NCCT, 465 CTA, and 269 CTP examinations. The mean radiation exposure in terms of CTDIvol and DLP was distributed as follows median (interquartile range; mean ± SD): for NCCT, 31.4 mGy (28.9–33.9; 31.5 ± 3.8) and 480.9 mGy cm (436.5–527.8; 486.6 ± 72.5), and for CTA, 9.3 mGy (6.0–13.7; 10.0 ± 4.3) and 329.5 mGy cm (224.6–478.3; 359.4 ± 159.4). CTP radiation exposure is invariable and depends on CT device as well as its protocol settings: (CTDIvol, DLP) for SOMATOM Definition AS+, 219.8 mGy and 2503.9 mGy cm; for SOMATOM Definition Flash, 258.2 mGy and 3044.3 mGy cm; and for SOMATOM Force, 124.9 mGy and 1852.6 mGy cm. The detailed results differentiated by the device are shown for CTDIvol in Table 2 and for DLP in Table 3.
Local DRLs and ADs of the CT protocol
Local DRLs in terms of CTDIvol and DLP could be depicted as follows (versus national DRLs proposed by the Federal Office for Radiation Protection) (Bundesamt für Strahlenschutz, Germany [34]): for NCCT, 33.9 mGy (60 mGy) and 527.8 mGy cm (860 mGy cm), and for CTA, 13.7 mGy (20 mGy) and 478.3 mGy cm (600 mGy cm). ADs could be determined as follows: (CTDIvol, DLP) for NCCT, 31.4 mGy and 480.9 mGy cm and for CTA, 9.3 mGy and 329.5 mGy cm. As radiation indices of CTP were uniform and scanner-specific, we waived to determine DRL and AD.
Comparison between CT scanners
In terms of CTDIvol, NCCT showed very similar distribution of radiation exposure between the investigated CT scanners with the lowest CTDIvol at SOMATOM Definition Flash (median 27.0 mGy, IQR 25.8–28.9 mGy), highest at SOMATOM Force (median 32.4 mGy, IQR 30.2–34.6 mGy), and SOMATOM Definition AS+ in between (median 29.7 mGy, IQR 28.5–31.4 mGy) (Table 2). In comparison, the radiation exposures of CTA varied substantially: the highest dose was required by SOMATOM Definition Flash (median 14.5 mGy, IQR 13.2–15.6 mGy) and lowest by SOMATOM Definition AS+ (median 5.8 mGy, IQR 5.4–6.0 mGy). CTDIvol for CTA at SOMATOM Force was in between (median 8.6 mGy, IQR 6.2–9.8 mGy). Accordingly, median CTDIvol was about 2.5 times higher (2.4 for DLP) at SOMATOM Definition Flash and about 1.5 times higher (1.4 for DLP) at SOMATOM Force compared with SOMATOM Definition AS+. The Kruskal-Wallis test with Dunn-Bonferroni post hoc test revealed that CTDIvol and DLP for NCCT and CTA were significantly different between the three different CT scanners (p < 0.001). Concerning CTP, the lowest CTDIvol was achieved by SOMATOM Force (median 124.9 mGy) which was about 50% lower than SOMATOM Definition Flash (median 258.2 mGy). Radiation exposure at SOMATOM Definition AS+ was in between and slightly lower than SOMATOM Definition Flash (median 219.8 mGy). Differences between the three CT scanners were similar in terms of DLP compared with CTDIvol (Table 3).
Discussion
Our study reveals useful radiation exposure data and local DRLs for a multimodal stroke CT protocol and shows that modern multi-slice CT scanners enable imaging with lower radiation exposure than national DRLs. However, the multimodal CT protocol increases total radiation exposure significantly, which must be balanced with diagnostic benefits.
Radiation exposure
Monitoring radiation exposure of CT examinations helps to ensure radiation protection and provides essential information to optimize CT protocols [35]. Therefore, standardized collecting of radiation dose data is a common practice at our institute. Our results are in keeping with previous studies which reported that a multimodal CT protocol requires relative high radiation exposure [4]. Accordingly, CT procedures are considered to comprise stochastic radiation risks [36]. Nevertheless, CTDIvol and DLP are not intended to derive estimates of individual patient risk as they do not include radiosensitivity of organs [27, 37]. However, CTDIvol and DLP are useful values which measure the ionizing radiation emitted from the scanner and therefore act as quality control metrics, which represent exposure values rather than patient doses [35]. DRLs are helpful benchmark which indicate typical ionizing radiation exposure values in a country, region, or an institute [38]. Several studies have reported local, regional, or national DRLs which is a reasonable solution as equipment and protocols vary by institutes and, a fortiori, by nations [38].
Comparison with national and published local DRLs
German national DRL for NCCT is set at 60 mGy (CTDIvol) and 850 mGy cm (DLP) [34]. DRLs at our institution for NCCT and CTA were below national DRLs (Fig. 1). The highest CTA DLP was 1028 mGy cm with a CTDIvol of 26.4 mGy, concluding that the major part of radiation excess was due to expanded scan length. However, national DRLs exist for NCCT and CTA only and there are no DRLs for CTP for the assessment of stroke. Further, DRLs for NCCT are set by the European Commission: weighted CT dose index (CTDIw) 60 mGy and DLP 1050 mGy cm [23]. In comparison with previous studies from different European countries, our local values are remarkable below the published DRLs. Most DRLs for NCCT vary between 60 and 80 mGy (CTDIvol) [39,40,41]. Besides, we calculated ADs as another reference value to encourage further optimization of radiation protection [42]. The whole gamut of our radiation exposure is well below the reported data: exposures are below several recently reviewed studies reporting NCCT DRLs from different countries with a DLP ranging from 787 to 1305 mGy cm [35] and a median DLP of 733 mGy cm with a range from 81 to 2173 mGy cm [37]. Ionizing radiation exposure of CT can vary significantly by institution [43, 44]. In addition, our results correspond with previous studies that demonstrated variation of radiation exposure due to intrinsic differences of CT scanners [45, 46]. Mnyusiwalla et al. reported a mean radiation exposure six times higher for a multimodal CT protocol for acute stroke compared with NCCT solely [4]. Such high radiation doses must be balanced with the benefits of enhanced anatomic and prognostic data [4].
Distribution of radiation exposure for volume-weighted CT dose index (CTDIvol) (mGy) and dose-length product (DLP) (mGy cm) of non-contrast CT (NCCT) of the head and CT angiography (CTA) for the assessment of acute stroke. Radiation exposure of three different multi-slice CT scanners (SOMATOM Definition AS+, Definition Flash, and Force; Siemens Healthcare, Forchheim, Germany). Red broken line represents national dose reference level (DRL) for NCCT, CTDIvol 60 mGy and DLP 850 mGy cm, and for CTA, CTDIvol 20 mGy and DLP 600 mGy cm. Green broken line represents determined local DRL which is well below the national DRL. Whiskers represent min to max
Comparison between CT scanners
The lowest radiation exposure for NCCT in terms of CTDIvol was depicted at SOMATOM Definition Flash, even though it was the only scanner where NCCT was acquired in dual-source mode (Tables 1 and 2). This can be affiliated to the increased pitch and decreased rotation time, which both result in decreased radiation dose. Nonetheless, radiation exposure indices and DRLs showed similar distributions at all three investigated CT scanners. For CTA, substantially diverging radiation exposures were depicted at the three CT scanners. Application of dual-source mode at SOMATOM Definition Flash and different technical settings resulted in substantially higher radiation dose compared with SOMATOM Definition AS+ and Force (Table 2). Variation of pitch as an inversely proportional parameter and of rotation time as a directly proportional parameter to CTDIvol caused the radiation exposures to differ considerably. Our results demonstrate that radiation exposure from CTP is invariable and depends on CT device as well as its protocol settings. Nonetheless, several studies have reported modifications to reduce radiation exposure of CTP [17, 47]. Furthermore, Othman et al. demonstrated that low-dose CTP generates sufficient perfusion maps [48]. In conclusion, if institutes perform CTP examinations as recommended by the vendor, radiation exposure is virtually a CT scanner-specific parameter, and modifying protocols will not reduce the proportion of radiation by CTP unless scanner settings are modified. Our data show that radiation exposure of CTP can vary substantially. Tube current-time product, tube voltage, and rotation time were decreased at SOMATOM Force which resulted in the lowest CTDIvol compared with SOMATOM Definition AS+ and Definition Flash.
Radiation risks
While short-term effects of ionizing radiation from CT techniques for stroke are rare, long-term effects are not entirely known [4]. Imanishi et al. reported three cases of bandage-shaped scalp hair loss in patients undergoing serial CTP studies combined with digital subtraction angiography, although it should be mentioned that these patients received multiple examinations [49]. Regarding long-term effects, the estimate for risk of fatal cancer due to radiation exposure is 5% per Sievert [50] but excess cancer mortality also depends on patients’ age and attributable risk of cancer decreases with age [51]. However, full CT protocol was indicated due to strong clinical suspicion of acute stroke. Fortunately, the major proportion of our patients carried a lower risk of radiation exposure–related cancer mortality due to a mean age of 66.7 ± 16.7 years (SD). Nevertheless, we strongly advocate a judicious use of a multimodal CT protocol, in particular for young patients due to their heightened risk from ionizing radiation [4].
Acute stroke CT protocol
As widely recommended [7], we use NCCT as the initial imaging modality in acute stroke to exclude intracranial hemorrhage or stroke mimicking etiologies. As inconspicuous initial NCCT examinations cannot be equated with exclusion of ischemic stroke, further assessment is required in a major proportion of patients. Therefore, there is an increasing interest in advanced and complementary CT techniques for the evaluation of acute stroke [2, 6]. Possible detection of occluded extra- and intracranial arteries provides an argument for performing a subsequent CTA [2, 10, 11]. Furthermore, complementary CTA and CTP provide additional, often relevant, information [2, 52,53,54]. Moreover, in agreement with the findings in previous studies [2, 55], we confirm that a multimodal CT protocol can be performed as a single-time examination and takes less than 10 min more than NCCT only.
Advantages and limitations
About 62% of all CT scans were performed at SOMATOM Force which results in an underrepresentation of the other CT devices. Only patients who were identified by the DICOM header–based tracking and monitoring software were included in this study, which can result in a sampling bias. The strengths of our study include the large number of patients assessed by a uniform CT protocol and the detailed report of radiation exposure between different modern multi-slice CT scanners.
Conclusion
Performing complementary advanced CT techniques such as CTA and CTP for the assessment of acute stroke increases total radiation exposure substantially. Hence, revised and completed DRLs for the acute stroke CT protocol are required, where our locally examined DRLs may help as benchmarks as they were well below the major proportion of recently published DRLs. DRLs regarding a full CT imaging workup for acute stroke assessment enable optimization of local radiation protection and provide actual reference values for dose monitoring.
Abbreviations
- AD:
-
Achievable dose
- NCCT:
-
Non-contrast computed tomography
- CTA:
-
Computed tomography angiography
- CTDIvol :
-
Volume-weighted CT dose index
- CTDIw :
-
Weighted CT dose index
- CTP:
-
Computed tomography perfusion
- DLP:
-
Dose-length product
- DRL:
-
Diagnostic reference level
- IQR:
-
Interquartile range
- kV:
-
Kilovolt (tube voltage)
- mAs:
-
Milliampere second (tube current-time product)
- RIS:
-
Radiological information system
- SD:
-
Standard deviation
References
World Health Organization-International Society of Hypertension (1999) Guidelines for the management of hypertension. Guidelines Subcommittee. J Hypertens 17:151–183
de Lucas EM, Sánchez E, Gutiérrez A, Mandly AG, Ruiz E, Flórez AF, Izquierdo J, Arnáiz J, Piedra T, Valle N, Bañales I, Quintana F (2008) CT protocol for acute stroke: tips and tricks for general radiologists. Radiographics 28:1673–1687. https://doi.org/10.1148/rg.286085502
Bogousslavsky J, Kaste M, Skyhoj Olsen T et al (2000) Risk factors and stroke prevention. European Stroke Initiative (EUSI). Cerebrovasc Dis 10(Suppl 3):12–21. https://doi.org/10.1159/000047577
Mnyusiwalla A, Aviv RI, Symons SP (2009) Radiation dose from multidetector row CT imaging for acute stroke. Neuroradiology 51:635–640. https://doi.org/10.1007/s00234-009-0543-6
Hacke W, Kaste M, Skyhoj Olsen T, Orgogozo JM, Bogousslavsky J (2000) European Stroke Initiative (EUSI) recommendations for stroke management. The European Stroke Initiative Writing Committee. Eur J Neurol 7:607–623. https://doi.org/10.1046/j.1468-1331.2000.00137.x
Konstas AA, Goldmakher GV, Lee T-Y, Lev MH (2009) Theoretic basis and technical implementations of CT perfusion in acute ischemic stroke, part 1: theoretic basis. AJNR Am J Neuroradiol 30:662–668. https://doi.org/10.3174/ajnr.A1487
Adams HP, del Zoppo G, Alberts MJ et al (2007) Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation 115:e478–e534. https://doi.org/10.1161/CIRCULATIONAHA.107.181486
von Kummer R, Meyding-Lamadé U, Forsting M et al (1994) Sensitivity and prognostic value of early CT in occlusion of the middle cerebral artery trunk. AJNR Am J Neuroradiol 15:9–15 discussion 16-8
Kloska SP, Nabavi DG, Gaus C, Nam EM, Klotz E, Ringelstein EB, Heindel W (2004) Acute stroke assessment with CT: do we need multimodal evaluation? Radiology 233:79–86. https://doi.org/10.1148/radiol.2331030028
Horowitz SH, Zito JL, Donnarumma R, Patel M, Alvir J (1991) Computed tomographic-angiographic findings within the first five hours of cerebral infarction. Stroke 22:1245–1253. https://doi.org/10.1161/01.str.22.10.1245
Prokop M (2000) Multislice CT angiography. Eur J Radiol 36:86–96. https://doi.org/10.1016/S0720-048X(00)00271-0
Lev MH, Farkas J, Rodriguez VR, Schwamm LH, Hunter GJ, Putman CM, Rordorf GA, Buonanno FS, Budzik R, Koroshetz WJ, Gonzalez RG (2001) CT angiography in the rapid triage of patients with hyperacute stroke to intraarterial thrombolysis: accuracy in the detection of large vessel thrombus. J Comput Assist Tomogr 25:520–528. https://doi.org/10.1097/00004728-200107000-00003
Lev MH, Nichols SJ (2000) Computed tomographic angiography and computed tomographic perfusion imaging of hyperacute stroke. Top Magn Reson Imaging 11:273–287. https://doi.org/10.1097/00002142-200010000-00004
Klotz E, König M (1999) Perfusion measurements of the brain: using dynamic CT for the quantitative assessment of cerebral ischemia in acute stroke. Eur J Radiol 30:170–184. https://doi.org/10.1016/S0720-048X(99)00009-1
Konstas AA, Wintermark M, Lev MH (2011) CT perfusion imaging in acute stroke. Neuroimaging Clin N Am 21:215–238, ix. https://doi.org/10.1016/j.nic.2011.01.008
Ezzeddine MA, Lev MH, McDonald CT et al (2002) CT angiography with whole brain perfused blood volume imaging: added clinical value in the assessment of acute stroke. Stroke 33:959–966. https://doi.org/10.1161/hs0402.105388
Wintermark M, Flanders AE, Velthuis B, Meuli R, van Leeuwen M, Goldsher D, Pineda C, Serena J, Schaaf I, Waaijer A, Anderson J, Nesbit G, Gabriely I, Medina V, Quiles A, Pohlman S, Quist M, Schnyder P, Bogousslavsky J, Dillon WP, Pedraza S (2006) Perfusion-CT assessment of infarct core and penumbra: receiver operating characteristic curve analysis in 130 patients suspected of acute hemispheric stroke. Stroke 37:979–985. https://doi.org/10.1161/01.STR.0000209238.61459.39
Campbell BCV, Weir L, Desmond PM, Tu HTH, Hand PJ, Yan B, Donnan GA, Parsons MW, Davis SM (2013) CT perfusion improves diagnostic accuracy and confidence in acute ischaemic stroke. J Neurol Neurosurg Psychiatry 84:613–618. https://doi.org/10.1136/jnnp-2012-303752
Deak PD, Smal Y, Kalender WA (2010) Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 257:158–166. https://doi.org/10.1148/radiol.10100047
Shrimpton PC, Wall BF (1995) The increasing importance of X-ray computed tomography as a source of medical exposure. Radiat Prot Dosim 57:413–415. https://doi.org/10.1093/oxfordjournals.rpd.a082572
Shrimpton PC, Hillier MC, Lewis MA, Dunn M (2006) National survey of doses from CT in the UK: 2003. Br J Radiol 79:968–980. https://doi.org/10.1259/bjr/93277434
Hidajat N, Mäurer J, Schröder RJ, Nunnemann A, Wolf M, Pauli K, Felix R (1999) Relationships between physical dose quantities and patient dose in CT. Br J Radiol 72:556–561. https://doi.org/10.1259/bjr.72.858.10560337
European Commission (1999) European guidelines on quality criteria for computed tomography. EUR, vol 16262. Office for Official Publications of the European Communities, Luxembourg
Shrimpton PC, Hillier MC, Lewis MA et al (2005) Doses from computed tomography (CT) examinations in the UK-2003 review. NRPB Chilton, UK
Bauhs JA, Vrieze TJ, Primak AN, Bruesewitz MR, McCollough CH (2008) CT dosimetry: comparison of measurement techniques and devices. Radiographics 28:245–253. https://doi.org/10.1148/rg.281075024
Task Group on Control of Radiation Dose in Computed Tomography (2000) Managing patient dose in computed tomography. A report of the International Commission on Radiological Protection. Ann ICRP 30:7–45. https://doi.org/10.1016/s0146-6453(01)00049-5
McCollough CH, Leng S, Yu L et al (2011) CT dose index and patient dose: they are not the same thing. Radiology 259:311–316. https://doi.org/10.1148/radiol.11101800
McNitt-Gray MF (2002) AAPM/RSNA physics tutorial for residents: topics in CT. Radiation dose in CT. Radiographics 22:1541–1553. https://doi.org/10.1148/rg.226025128
McCollough CH, Bruesewitz MR, Kofler JM (2006) CT dose reduction and dose management tools: overview of available options. Radiographics 26:503–512. https://doi.org/10.1148/rg.262055138
Huda W, Ogden KM, Khorasani MR (2008) Converting dose-length product to effective dose at CT. Radiology 248:995–1003. https://doi.org/10.1148/radiol.2483071964
Institute of Physics and Engineering in Medicine (2004) Report 88: guidance on the establishment and use of diagnostic reference levels for medical X-ray examinations, York, England
National Council on Radiation Protection and Measurements (2012) Report No. 172. Reference levels and achievable doses in medical and dental imaging: recommendations for the United States
Cook TS, Zimmerman S, Maidment ADA, Kim W, Boonn WW (2010) Automated extraction of radiation dose information for CT examinations. J Am Coll Radiol 7:871–877. https://doi.org/10.1016/j.jacr.2010.06.026
Bundesamt für Strahlenschutz (2016) Bekanntmachung der aktualisierten diagnostischen Referenzwerte für diagnostische und interventionelle Röntgenanwendungen. Bundesanzeiger. AT 15.07.2016
MacGregor K, Li I, Dowdell T, Gray BG (2015) Identifying institutional diagnostic reference levels for CT with radiation dose index monitoring software. Radiology 276:507–517. https://doi.org/10.1148/radiol.2015141520
Little MP (2003) Risks associated with ionizing radiation. Br Med Bull 68:259–275. https://doi.org/10.1093/bmb/ldg031
Pantos I, Thalassinou S, Argentos S, Kelekis NL, Panayiotakis G, Efstathopoulos EP (2011) Adult patient radiation doses from non-cardiac CT examinations: a review of published results. Br J Radiol 84:293–303. https://doi.org/10.1259/bjr/69070614
Vassileva J, Rehani M (2015) Diagnostic reference levels. AJR Am J Roentgenol 204:W1–W3. https://doi.org/10.2214/AJR.14.12794
Danish Health Authority (2015) CT referencedoser. Indsamling og vurdering af patientdoser ved CT. https://www.sst.dk/-/media/Udgivelser/2015/CT-referencedoser/CT-referencedoser-2015%2D%2D-Indsamling-og-vurdering-af-patientdoser-ved-CT.ashx?la=da&hash=B83B89ABD4F9EFB7919C4E9C0AF7DD0640AA0286. Accessed 26 May 2020
Public Health England PHE-CRCE-013, Doses from computed tomography (CT) examinations in the UK - 2011 review. Chilton, UK
Treier R, Aroua A, Verdun FR, Samara E, Stuessi A, Trueb PR (2010) Patient doses in CT examinations in Switzerland: implementation of national diagnostic reference levels. Radiat Prot Dosim 142:244–254. https://doi.org/10.1093/rpd/ncq279
National Council on Radiation Protection and Measurements (2012) Reference levels and achievable doses in medical and dental imaging: recommendations for the United States. Bethesda, USA
Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de González A, Miglioretti DL (2009) Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med 169:2078–2086. https://doi.org/10.1001/archinternmed.2009.427
Héliou R, Normandeau L, Beaudoin G (2012) Towards dose reduction in CT: patient radiation dose assessment for CT examinations at university health center in Canada and comparison with national diagnostic reference levels. Radiat Prot Dosim 148:202–210. https://doi.org/10.1093/rpd/ncr024
Kalender WA (1998) Computed tomography: influence of exposure parameters and the establishment of reference dose values. Radiat Prot Dosim 80:163–166. https://doi.org/10.1093/oxfordjournals.rpd.a032496
Smith A, Shah GA, Kron T (1998) Variation of patient dose in head CT. Br J Radiol 71:1296–1301. https://doi.org/10.1259/bjr.71.852.10319004
Hirata M, Murase K, Sugawara Y, Nanjo T, Mochizuki T (2005) A method for reducing radiation dose in cerebral CT perfusion study with variable scan schedule. Radiat Med 23:162–169
Othman AE, Brockmann C, Yang Z, Kim C, Afat S, Pjontek R, Nikobashman O, Brockmann MA, Kim JH, Wiesmann M (2015) Effects of radiation dose reduction in volume perfusion CT imaging of acute ischemic stroke. Eur Radiol 25:3415–3422. https://doi.org/10.1007/s00330-015-3763-7
Imanishi Y, Fukui A, Niimi H, Itoh D, Nozaki K, Nakaji S, Ishizuka K, Tabata H, Furuya Y, Uzura M, Takahama H, Hashizume S, Arima S, Nakajima Y (2005) Radiation-induced temporary hair loss as a radiation damage only occurring in patients who had the combination of MDCT and DSA. Eur Radiol 15:41–46. https://doi.org/10.1007/s00330-004-2459-1
National Council on Radiation Protection and Measurements (1993) Limitation of exposure to ionizing radiation: recommendations of the National Council on Radiation Protection and Measurements. NCRP report, no. 116. The Council, Bethesda, MD
National Research Council (2006) Health risks from exposure to low levels of ionizing radiation. National Academies Press, Washington, D.C.
Lev MH, Segal AZ, Farkas J, Hossain ST, Putman C, Hunter GJ, Budzik R, Harris GJ, Buonanno FS, Ezzeddine MA, Chang Y, Koroshetz WJ, Gonzalez RG, Schwamm LH (2001) Utility of perfusion-weighted CT imaging in acute middle cerebral artery stroke treated with intra-arterial thrombolysis: prediction of final infarct volume and clinical outcome. Stroke 32:2021–2028. https://doi.org/10.1161/hs0901.095680
Schramm P, Schellinger PD, Fiebach JB, Heiland S, Jansen O, Knauth M, Hacke W, Sartor K (2002) Comparison of CT and CT angiography source images with diffusion-weighted imaging in patients with acute stroke within 6 hours after onset. Stroke 33:2426–2432. https://doi.org/10.1161/01.str.0000032244.03134.37
Rai AT, Carpenter JS, Peykanu JA, Popovich T, Hobbs GR, Riggs JE (2008) The role of CT perfusion imaging in acute stroke diagnosis: a large single-center experience. J Emerg Med 35:287–292. https://doi.org/10.1016/j.jemermed.2007.08.071
Parsons MW, Pepper EM, Chan V, Siddique S, Rajaratnam S, Bateman GA, Levi CR (2005) Perfusion computed tomography: prediction of final infarct extent and stroke outcome. Ann Neurol 58:672–679. https://doi.org/10.1002/ana.20638
Acknowledgements
Open Access funding provided by Projekt DEAL.
Funding
The authors state that this work has not received any funding. D. Bos was supported as a clinician scientist within the University Medicine Essen Academy (UMEA) program, funded by the German Research Foundation (DFG; grant FU356/12-1) and the Faculty of Medicine, University of Duisburg-Essen.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required. An Institutional Review Board approval was obtained (20-9175-BO).
Informed consent
A written informed consent was waived by the Institutional Review Board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zensen, S., Guberina, N., Opitz, M. et al. Radiation exposure of computed tomography imaging for the assessment of acute stroke. Neuroradiology 63, 511–518 (2021). https://doi.org/10.1007/s00234-020-02548-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02548-z