Abstract
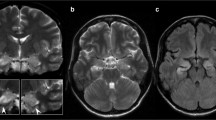
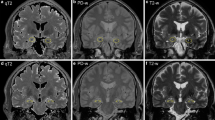
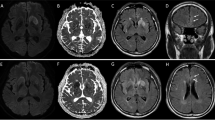
Introduction: The aim of the study was to analyze serial magnetic resonance imaging (MRI) scans in patients with various forms of limbic encephalitis (LE) in order to evaluate whether, and at what time point, MRI findings support the diagnosis of LE. Methods: Serial MRI scans (1 day to 15 years after the onset of symptoms) of 20 patients with LE were retrospectively evaluated. Of these 20 patients, 16 had definite LE (histopathological limbic inflammation, n=6; onconeural antibodies, n=5; voltage-gated potassium channel antibodies, n=3; malignant tumors, n=5), and 4 possible LE because they met the clinical criteria but had no typical antibodies or tumors. Results: Of 13 patients who were studied with MRI within 3 months after the onset of symptoms, 11 had swollen temporomesial structures (unilateral, n=7; bilateral, n=4). After up to 9 months, the swelling had resolved in nine of ten re-evaluated patients. Of seven patients who were initially studied with MRI more than 3 months after disease onset, three had swollen temporomesial structures, one had a hyperintense, normal-sized hippocampus, and three had hyperintense and atrophic temporomesial structures. Conclusion: LE starts as an acute disease with uni- or bilateral swollen temporomesial structures that are hyperintense on fluid attenuation inversion recovery and T2-weighted sequences. Swelling and hyperintensity may persist over months to years, but in most cases progressive temporomesial atrophy develops.




Similar content being viewed by others
References
Brierley JB, Corsellis JA, Hierons R, Nevin S (1960) Subacute encephalitis of later adult life, mainly affecting the limbic areas. Brain 83:357–368
Bernal F, Graus F, Pifarre A, Saiz A, Bernyahia B, Ribalta T (2002) Immunohistochemical analysis of anti-Hu-associated paraneoplastic encephalomyelitis. Acta Neuropathol 103:509–515
Gultekin SH, Rosenfeld MR, Voltz R, Eichen J, Posner JB, Dalmau J (2000) Paraneoplastic limbic encephalitis: neurological syndromes, immunological findings, and tumour association in 50 patients. Brain 123:1481–1494
Mihara M, Sugase S, Konaka K, et al (2005) The pulvinar sign in a case of paraneoplastic limbic encephalitis associated with non-Hodgkin’s lymphoma. J Neurol Neurosurg Psychiatry 76:882–884
Bien CG, Schulze-Bonhage A, Deckert-Schlüter M, et al (2000) Limbic encephalitis unrelated to neoplasm as a cause of temporal lobe epilepsy. Neurology 55:1823–1828
Pozo-Rosich P, Clover L, Saiz A, Vincent A, Graus F (2003) Voltage-gated potassium channel antibodies in limbic encephalitis. Ann Neurol 54:530–533
Vincent A, Buckley C, Schott JM, et al (2004) Potassium channel antibody-associated encephalopathy: a potentially immunotherapy-responsive form of limbic encephalitis. Brain 127:701–712
Thieben MJ, Lennon VA, Boeve BF, Aksamit AJ, Keegan M, Vernino S (2004) Potentially reversible autoimmune limbic encephalitis with neuronal potassium channel antibody. Neurology 62:1177–1182
Fauser S, Talazko J, Wagner K, et al (2005) FDG-PET and MRI in potassium channel antibody-associated non-paraneoplastic limbic encephalitis: correlation with clinical course and neuropsychology. Acta Neurol Scand 111:338–343
Söder BM, Urbach H, Elger CE, Bien CG, Beyenburg S (2005) VGKC-antibody-associated limbic encephalitis. Nervenarzt 76:760–762
Graus F, Delattre JY, Antoine C, et al (2004) Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry 75:1135–1140
Lacomis D, Hhoshbin S, Schich RM (1990) MR Imaging of paraneoplastic limbic encephalitis. J Comput Assist Tomogr 14:115–117
Dirr LY, Elster AD, Donofrio PD, Smith M (1990) Evolution of brain MRI abnormalities in limbic encephalitis. Neurology 40:1304–1306
Kodama T, Numaguchi Y, Gellad FE, Dwyer BA, Kristt DA (1991) Magnetic resonance imaging of limbic encephalitis. Neuroradiology 33:520–523
Flacke S, Wüllner U, Keller E, Hamzei F, Urbach H (2000) Reversible changes of echoplanar perfusion and diffusion weighted MRI during status epilepticus. Neuroradiology 42:92–95
Urbach H, Sassen R, Soeder BM, Flacke S, Becker A, Bien CG (2006) Serial MRI in patients with acquired hippocampal sclerosis. Clin Neuroradiol 16:47–52
Hirai T, Korogi Y, Yoshizumi Y, et al (2000) Limbic lobe of the human brain: evaluation with turbo fluid-attenuated inversion recovery MR imaging. Radiology 215:470–475
Arain A, Abou-Khalil B, Moses H (2001) Hashimoto’s encephalopathy: documentation of mesial temporal seizure origin by ictal EEG. Seizure 10:438–441
McCabe DJ, Burke T, Connolly S, Hutchinson M (2000) Amnestic syndrome with bilateral mesial temporal lobe involvement in Hashimoto’s encephalopathy. Neurology 54:737–739
Stübgen JP (1998) Nervous system lupus mimics limbic encephalitis. Lupus 7:557–560
Scheid R, Voltz R, Vetter T, Sabri O, von Cramon DY (2005) Neurosyphilis and paraneoplastic limbic encephalitis: important differential diagnoses. J Neurol 252:1129–1132
Henson RA, Hoffmann HL, Ulrich H (1965) Encephalomyelitis with carcinoma. Brain 88:449–464
Lang B, Dale RC, Vincent A (2003) New autoantibody mediated disorders of the central nervous system. Curr Opin Neurol 16:351–357
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Urbach, H., Soeder, B.M., Jeub, M. et al. Serial MRI of limbic encephalitis. Neuroradiology 48, 380–386 (2006). https://doi.org/10.1007/s00234-006-0069-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-006-0069-0