Abstract
Purpose
To describe outcomes from the first-in-human study of dersimelagon, an investigational oral selective MC1R agonist, under development for the treatment of erythropoietic protoporphyria (EPP) and X-linked protoporphyria (XLP).
Methods
In this double-blind, placebo-controlled phase 1 study, the safety, tolerability, pharmacokinetics, and pharmacodynamics of single and multiple ascending oral doses of dersimelagon in healthy participants were evaluated.
Results
Dersimelagon was generally well tolerated in healthy participants, with the most common TEAEs being lentigo (52.8%) and skin hyperpigmentation (50.0%) after multiple doses. Systemic exposure to dersimelagon in plasma (based on AUC0-∞ and Cmax) increased in a slightly more than dose-proportional manner over the 1- to 600-mg single-dose range. Following multiple doses, dersimelagon was rapidly absorbed (median Tmax ranging from 4 to 5 h postdose on days 1 and 14). Mean t1/2 ranged from 10.56 to 18.97 h on day 14, and the steady state of plasma concentration was generally reached by 5 days of multiple dosing. There were no observable effects of age or race on the PK profile of dersimelagon or its metabolite dersimelagon glucuronide. No treatment-related effects on melanin density (MD) were observed following single doses of dersimelagon; however, after multiple doses, increases in MD were observed in participants receiving 150 and 300 mg dersimelagon.
Conclusion
Our study results indicate that dersimelagon is generally well tolerated and demonstrates a generally consistent PK profile across diverse subgroups. Treatment-related increases in MD warrant further investigation in a larger study population and in patients with EPP and XLP.
Trial registration
A Study to Investigate the Safety, Tolerability and Pharmacokinetics of MT-7117 in Healthy Subjects, NCT02834442, https://clinicaltrials.gov/ct2/show/NCT02834442, registration began July 2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The porphyrias are a heterogeneous group of rare inherited metabolic disorders caused by enzymatic deficiencies of the heme biosynthetic pathway [1,2,3]. Erythropoietic porphyrias, which include erythropoietic protoporphyria (EPP) and X-linked protoporphyria (XLP), result from mutations of the ferrochelatase (FECH) gene in EPP and mutations in the aminolevulinic acid synthase-2 (ALAS2) gene in XLP [1,2,3]. EPP is the most frequent type of porphyria in children and the third most common porphyria overall, with prevalence estimates ranging from 1 in 75,000 in the Netherlands to 1 in 200,000 in the United Kingdom (UK) [1]. Both EPP and XLP are characterized by accumulation of protoporphyrin in blood, erythrocytes, and tissues, leading to cutaneous photosensitivity manifesting as burning, swelling, itching, erythema, and severe pain in sun-exposed areas [1,2,3].
Current approaches to the management of EPP and XLP are primarily limited to preventive measures, including sun avoidance and use of protective clothing and sunscreens, posing a substantial burden to patients by requiring significant lifestyle adjustments [1,2,3]. In addition, treatment options have been limited to mainly symptomatic management, while curative approaches have consisted of hematopoietic stem cell transplant for patients with EPP who have severe progressive disease and are at high risk for complications and mortality. Currently, afamelanotide, a melanocortin 1 receptor (MC1R) agonist, is the only approved pharmacological intervention indicated for use in patients with EPP [1, 4]. Afamelanotide is a subcutaneous implant and must be administered by a healthcare professional, requiring patients to commute to healthcare facilities [4]. There remains a high unmet medical need for new safe and effective treatments, and the development of a well-tolerated oral treatment for EPP and XLP may address this unmet need.
Dersimelagon, a novel synthetic orally administered non-peptide small molecule that acts as a selective agonist for MC1R, is currently being investigated for the prevention of phototoxicity in patients with EPP and XLP and inhibition of the fibrotic process in patients with diffuse cutaneous systemic sclerosis (dcSSc). In preclinical studies, dersimelagon exhibited the highest affinity for human MC1R compared with other melanocortin receptors, with a half maximal effective concentration (EC50) in the nanomolar range [5]. Dersimelagon also has been shown to induce melanogenesis in both in vitro and in vivo studies, with increased melanin production occurring in a concentration‐dependent manner in a mouse B16F1 melanoma cell line [5]. Furthermore, oral administration of dersimelagon significantly induced coat color darkening in mice and significant skin pigmentation in a reversible manner in monkeys [5].
In a recently completed phase 2 randomized, multicenter, placebo-controlled clinical trial, ENDEAVOR (ClinicalTrials.gov ID: NCT03520036), the safety and efficacy of dersimelagon at doses of 100 mg and 300 mg were investigated [6]. The results of ENDEAVOR, which included 102 patients with EPP or XLP, indicated that dersimelagon was efficacious at increasing symptom-free light exposure and had an acceptable safety and tolerability profile after 16 weeks of treatment [6]. Here, we report the results of a first-in-human phase 1 double-blind, placebo-controlled study (ClinicalTrials.gov ID: NCT02834442) that evaluated the safety, tolerability, pharmacokinetics (PK), and pharmacodynamics (PD) of single and multiple ascending oral doses of dersimelagon in healthy participants, including effects of sex, age, and race on the PK profile of dersimelagon. To complement these results, and because the information on distribution volume, clearance, and absolute bioavailability in animals is helpful in understanding the PK characteristics of dersimelagon, we also report findings from the preceding nonclinical animal studies to demonstrate the similarity between the preclinical PK profile in animals and the clinical PK profile of dersimelagon in humans. Moreover, allometric projections from animal PK data are described.
Methods
Study design
This trial was a phase 1 randomized, double-blind, placebo-controlled study conducted at a single center in the UK. Prior to study initiation, the protocol and all other appropriate documents were reviewed and approved by an Independent Ethics Committee and local regulatory authorities. The study was conducted in accordance with the ethical principles stated in the Declaration of Helsinki, the International Conference on Harmonisation for Good Clinical Practice guidance, and all local and regional applicable laws and regulations. Prior to the performance of any study-related assessments and procedures, all participants signed a written informed consent form with details of the trial treatment, procedures, and potential risks.
Study participants
The study consisted of eight parts, of which only five are presented in this report (A, D, E, F, and H) and summarized in eTable 1. Eligible participants were healthy individuals aged 18 to 55 years (inclusive at screening, except for Part H) with a body weight ≥ 50 kg for females and ≥ 60 kg for males and a body mass index (BMI) ranging from 18 to 30 kg/m2 at the time of screening and day 1. Part A included White males, whereas Part D included White females who were not pregnant or lactating. Part F included Black males, and Part H included White males aged ≥ 65 years. Participants who had previously received dersimelagon, who had used afamelanotide or melanotan within 6 months prior to the study, or with a history of melanoma and/or dysplastic naevus were not included in the study. Randomization was performed according to a computer-generated randomization list using SAS® version 9.3 (Cary, North Carolina, US) prior to the first administration of study drug.
Study treatments
Dersimelagon was supplied as a 50-mg tablet or as a powder (1 to 600 mg, for oral suspension) of active substance, and placebo was supplied as either a tablet or powder to match dersimelagon dosage strength.
Single doses
Part A of the study was a single ascending dose (SAD) study conducted in seven dosed cohorts. Each cohort was composed of eight participants, and in each cohort, participants were randomized to receive dersimelagon suspension (n = 6) or placebo suspension (n = 2). In total, 56 participants were included and received dersimelagon at doses of 1 mg, 3 mg, 10 mg, 30 mg, 100 mg, 300 mg, and 600 mg. In parts D, F, and H of the study, participants received a single oral dose of either 100 mg of dersimelagon (n = 6) or placebo (n = 2) as a tablet formulation. To evaluate the effect of sex difference Part D included eight female participants, and Part F evaluated the effect of race, and included eight Black participants. Part H evaluated the effect of age in eight participants aged ≥ 65 years.
Multiple ascending doses
The multiple ascending dose (MAD) study (Part E) was conducted in four cohorts in which participants received multiple dose administration of dersimelagon as a tablet or suspension formulation for 14 days in one treatment period. Each cohort was composed of 12 participants who were randomized to dersimelagon (n = 9) or placebo (n = 3). The dose levels of dersimelagon used were 30 mg (Cohort 1, suspension), 150 mg (Cohort 2, tablet), 300 mg (Cohort 3, tablet), and 450 mg (Cohort 4, tablet). A Fitzpatrick scale test was performed at screening to categorize patient skin types into type I (always burns, never tans), type II (usually burns, tans with difficulty), type III (sometimes mild burn, gradually tans), type IV (rarely burns, tans with ease), type V (very rarely burns, tans very easily), or type VI (never burns, always tans) [7]. Participants with Fitzpatrick skin types II to IV were included in the 30-, 150-, and 300-mg cohorts. The protocol was amended following emerging pigmentation data, and only participants with Fitzpatrick skin type V were included in the 450-mg cohort.
Safety assessments
Safety and tolerability were assessed by evaluating vital signs (supine blood pressure, pulse rate, respiratory rate, and body temperature), 12-lead electrocardiogram (ECG) parameters, clinical laboratory assessments, and adverse events (AEs). AEs were considered treatment emergent if they occurred after the first administration of dersimelagon or if a predose event increased in severity following dosing. The frequency and incidence of treatment-emergent AEs (TEAEs) were summarized by system organ class and preferred term for each treatment group. AEs were coded using the Medical Dictionary for Regulatory Activities (MedDRA) version 19.0. Safety laboratory test results, vital signs, and ECG parameters were summarized by treatment group and planned sampling point. All participants in the study (N = 144) were included in the safety analysis population.
Pharmacokinetic assessments
Blood samples for single-dose PK evaluations (Parts A, D, F, and H) were collected at predose and at 0.25, 0.5, 1, 2, 3, 4, 5, 6, 8, 10, 12, 24, and 48 h postdose and at day 5 follow-up (96 h). Blood samples for MAD evaluations (Part E) were collected on day 1 (predose and at 0.25, 0.5, 1, 2, 3, 4, 5, 6, 8, 10, and 12 h postdose), day 2 to day 13 (predose), day 14 (predose and at 0.25, 0.5, 1, 2, 3, 4, 5, 6, 8, 10, and 12 h postdose), day 15 (24 h post last dose), day 16 (48 h post last dose), and day 17 (72 h post last dose). To determine the concentrations of dersimelagon and dersimelagon glucuronide (a primary in vitro human metabolite), plasma samples were analyzed using a validated liquid chromatography coupled with tandem mass spectrometry (LC/MS/MS) method with solid phase extraction with a lower limit of quantification (LLOQ) of 0.1 ng/mL. The plasma PK parameters, including maximum observed plasma concentration (Cmax), time to maximum plasma concentration (Tmax), plasma terminal elimination half-life (t½), area under the plasma concentration–time curve from time zero to the last measurable concentration (AUC0-last), to infinity (AUC0-∞), and over the 24-h dosing interval, at steady state (AUC0-τ) were calculated with reference to day 1 dosing and/or the last day of dosing where applicable for dersimelagon and its metabolite dersimelagon glucuronide. The PK parameters were derived by noncompartmental analysis using Phoenix WinNonlin® software version 6.3 (Certara, LP, Princeton, New Jersey, US). For the calculation of PK parameters, data below the LLOQ were imputed a value of zero. Participants who received at least one dose of dersimelagon and who had at least one postdose value of plasma concentration (N = 110) were included in the PK analysis population.
Pharmacodynamic assessments
The effect of dersimelagon treatment on pigmentation was assessed in all participants in Part A by measuring melanin density on three skin segments (lower back, forehead, and cheek) by spectrophotometry (Konica Minolta Spectrophotometry) prior to dersimelagon administration and at days 3, 5, and 15 following a single oral dose of dersimelagon. In Part E, melanin density was measured prior to dersimelagon administration and at days 3, 5, 7, 10, 15, 22, 29, and 57 by spectrophotometry on the lower back, forehead, cheek, neck, inner upper arm, and outer forearm. The melanin density was calculated according to the following formula:
where R400 is the reflection at 400 nm and R420 is the reflection at 420 nm [8, 9]. Participants who received at least one dose of dersimelagon or placebo and who had at least one postdose value of melanin density (Part A: N = 56; Part E: N = 48) were included in the PD analysis population.
Statistical methods
The statistical analysis was performed using SAS® version 9.4 (SAS Institute Inc.; Cary, North Carolina, US). All variables were summarized by dose level for the SAD and MAD parts and by sex, age, and race category as appropriate. Unless otherwise stated, continuous data were summarized descriptively including N (number of participants), n (number of observations), mean, standard deviation, minimum, median, and maximum. Categorical data were summarized using frequency tables (frequency and percent). A linear model was used to analyze log-transformed AUC (AUC0-∞) and Cmax, with race (White vs Black), sex (male vs female), or age (≤ 55 years vs ≥ 65 years) as fixed effects. The difference in least squares (LS) means and corresponding 90% CIs were back-transformed to obtain the estimates and CIs of the geometric mean ratios comparing Black with White, female with male, and participants aged ≥ 65 years with those who were aged ≤ 55 years. In Part A (SAD) and Part E (MAD), PK parameters of interest were used to evaluate dose proportionality. A linear model was used to fit the power model after log transformation of the parameter of interest. The model included the log-transformed dose as a fixed effect. The point estimate and its 95% CI were derived for slope β to evaluate dose proportionality. The results were considered dose proportional if the CI included 1.
Nonclinical animal studies
All animal studies were performed according to the rules for the proper conduct of animal experiments and approved by the Institutional Animal Care and Use Committee of the test facility. Additional details regarding the nonclinical study protocols can be found in the Supplementary methods.
PK study in rats
A study was conducted to characterize the PK of dersimelagon in male Sprague–Dawley rats (n = 4) after a single oral administration (0.3, 1, and 3 mg/kg) and intravenous administration (2 mg/kg).
PK study in monkeys
A study was conducted to evaluate the PK of dersimelagon up to 48 h when administered orally (3 mg/kg) and intravenously (1 mg/kg) to male cynomolgus monkeys (n = 4).
In vitro plasma protein binding of dersimelagon
In vitro binding of radiolabeled [14C] dersimelagon free base to plasma proteins of rats, cynomolgus monkeys, and humans was examined by the equilibrium dialysis method. The [14C] dersimelagon free base (0.1, 1, and 9 µg/mL)-spiked plasma was incubated in a rapid equilibrium dialysis device for 8 h at 37 °C in a CO2 incubator.
Allometric scaling
The prediction of human clearance (CLh) from animal PKs was performed with several allometric approaches, including simple allometry, allometry with bile flow correction factor [10], allometry with the rule of exponent [11], allometry with unbound clearance approach [12], and fu-corrected intercept method [13]. The human distribution volume was predicted by simple allometry. The human bioavailability (F) was calculated employing the following equation:
where Fa, Fg, and Fh are fractions of orally administered drugs absorbed from the intestine, intestinal availability, and hepatic availability, respectively. Human Fa was assumed to be equivalent to rat Fa (0.64, which was calculated from a mass balance study in rats). Human Fg was assumed to be 1.0, because dersimelagon was very stable in human intestinal microsomes. Human Fh was calculated from the following equation:
where Rb (blood/plasma concentration ratio) was 0.6 (obtained by in vitro studies), and Qh (hepatic blood flow rate) was 1200 mL/h/kg. Based on these parameters, the plasma concentration–time profile at an oral dose of 100 mg in humans was simulated using 2-compartment model with 70 kg as the body weight and 1.0 h−1 as absorption rate constant, and the resultant Cmax and AUC values were obtained.
Results
Study participants
A total of 144 participants were randomized, of whom 143 completed the study. A total of 110 participants were treated with at least one dose of dersimelagon, and 34 participants were treated with a placebo. In parts A, D, F, and H, participants (n = 54) were exposed to single doses of dersimelagon ranging from 1 to 600 mg. In the MAD study (Part E), participants (n = 36) were treated with multiple doses of dersimelagon ranging from 30 to 450 mg. The baseline demographics of study participants are summarized in Table 1. All participants were male, except for eight female participants in Part D. Mean age, weight, and BMI were generally similar across treatment groups within each part of the study, with the exception of female participants, who had a slightly lower body weight than other participants. The baseline Fitzpatrick skin type of participants in the MAD study (Part E) is summarized in eTable 2. Of note, 88.9% of participants who received 450 mg of dersimelagon in the MAD study identified as Black, and all were Fitzpatrick skin type V, based on emerging pigmentation data obtained from previous cohorts in Part E.
Safety and tolerability
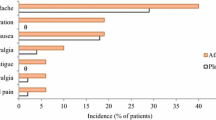
The TEAEs reported by at least two participants in any treatment group are summarized in Table 2. Overall, the incidence of TEAEs was relatively low, with most events occurring during Part A (SAD) and Part E (MAD) and the majority being mild to moderate in severity. No deaths or serious AEs were reported during any part of the study. Single oral doses of dersimelagon were generally well tolerated at levels of 1 to 600 mg. In Part A (SAD), 24 TEAEs were reported by 13 (31.0%) participants receiving dersimelagon, and three TEAEs were reported by three (21.4%) participants receiving placebo. The most common TEAEs experienced in Part A were headache and nausea, each reported in two (4.8%) participants, and contact dermatitis in three (7.1%) participants. Of these TEAEs, only headache and nausea were considered possibly related to study drug. In Part D (effect of sex), there was one TEAE experienced by one participant receiving placebo and none reported by those receiving dersimelagon. No TEAEs were reported during Parts F (effect of race) or H (effect of age). In Part E (MAD), 151 TEAEs were experienced by 34 (94.4%) participants receiving dersimelagon, and 10 TEAEs were experienced by four (33.3%) participants receiving placebo.
Overall, participants who received multiple doses (Part E) had a higher incidence of TEAEs than those who received a single dose (Parts A, D, F, and H). The most common TEAEs experienced in participants receiving multiple doses of dersimelagon were related to skin pigmentation, including lentigo (n = 20), skin hyperpigmentation (n = 19), and melanocytic naevus (n = 10). Two cases of melanocytic naevus reported by participants receiving 300 mg of dersimelagon were considered severe; however, both cases were confirmed to be nonmalignant. There were no safety concerns based on laboratory parameters, vital signs, ECG, and physical examination for any group during the study.
Pharmacokinetics of dersimelagon
Single ascending dose study (Part A)
Following single oral doses of 1, 3, 10, 30, 100, 300, and 600 mg, dersimelagon was rapidly absorbed, with median Tmax values generally similar at each dose, ranging from 1.99 to 5.00 h postdose (Table 3). After reaching Cmax, the plasma concentrations of dersimelagon appeared to decline in a biphasic manner (Fig. 1). The mean t½ of dersimelagon was generally similar across the 10- to 600-mg doses, with values ranging from 7.63 to 10.58 h. At the lower dose levels of 1 and 3 mg, the mean t½ was shorter, ranging between 5.14 to 6.43 h, due to the lack of point estimates in the terminal phase for the estimation of the elimination rate constant (kel). Dose-normalized plasma PK parameters are presented in eFig. 1, and analysis of dose proportionality is presented in eTable 3. The slope estimates (95% CI) from the regression analysis for AUC0-∞ and Cmax were 1.12 (1.07–1.17) and 1.05 (1.00–1.10), respectively, for dersimelagon. The lower limit of the 95% CI above unity indicated that the systemic exposure to dersimelagon in plasma, based on AUC0-∞ and Cmax values, appeared to increase in a slightly more than dose-proportional manner over the 1- to 600-mg single dose range (eTable 3).
Dersimelagon was rapidly metabolized to dersimelagon glucuronide, a major metabolite of dersimelagon, and demonstrated a similar PK profile to dersimelagon, with a median Tmax similar to dersimelagon across dose levels (between 1 and 5 h postdose); however, the systemic exposures to dersimelagon glucuronide based on Cmax and AUC0-∞ were extremely low compared with that of unchanged dersimelagon (ratio of Cmax or AUC0-∞ of dersimelagon glucuronide to that of unchanged dersimelagon: ≤ 0.05; data not shown).
Effect of sex (Part D), age (Part H), and race (Part F)
Following a single oral dose, 100 mg of dersimelagon was rapidly absorbed in all demographic subgroups, with Tmax occurring at similar times across comparator subgroups (Tmax = 3 vs 5 h in males vs females; 3 vs 2.6 h in participants ≤ 55 years vs participants ≥ 65 years; 3 vs 3.99 h in White vs Black participants; Table 3; eFig. 2). The mean t½ values for dersimelagon were also similar across comparator subgroups, indicating comparable elimination profiles regardless of demographics.
Both Cmax and AUC0-∞ were higher in female participants compared with those in males; however, only the difference in AUC0-∞ was significant based on the 90% CI of the ratio of female over male since 90% CIs did not include the value 1 (Table 4). In participants ≥ 65 years, geometric LS mean Cmax and AUC0-∞ were approximately 37% and 25% higher, respectively, compared with participants ≤ 55 years, but these differences were not statistically significant. Geometric LS mean Cmax and AUC0-∞ were similar in Black and White participants, and differences were not statistically significant.
Multiple ascending dose study (Part E)
Following multiple doses at 30, 150, 300, and 450 mg, dersimelagon was rapidly absorbed, with median Tmax values ranging from 4 to 5 h postdose on days 1 and 14. The mean t1/2 values ranged from 6.28 to 15.55 h on day 1 and 10.56 to 18.97 h on day 14 (Table 5). The day 14 slope estimates (95% CI) from the regression analysis for AUC0-τ and Cmax were 1.26 (1.14–1.39) and 1.25 (1.13–1.36), respectively, for dersimelagon. The lower limit of the 95% CIs of the slopes were over unity, indicating a slightly more than dose-proportional increase in the systemic exposure over the dose range of 30 to 450 mg (eTable 3; eFig. 3). There was a slight accumulation of dersimelagon following multiple dosing on day 14 compared to day 1, with mean ratio of accumulation (RA) values ranging from 1.14 to 1.82 across the 30- to 450-mg dose range while the mean linearity factor (LF) values were 1.07 to 1.53 over this dose range. The mean trough concentration ratios were over 0.95 after 5 days of multiple dosing at each dose level, suggesting that steady state was generally reached by day 5 of multiple dosing (eFig. 4). The PK profile of dersimelagon glucuronide followed a similar trend, with a median Tmax and mean t1/2 similar to dersimelagon across dose levels on days 1 and 14. However, as shown in Part A (SAD study), the systemic exposure to dersimelagon glucuronide was extremely low compared with that of unchanged dersimelagon (data not shown).
Pharmacodynamics of dersimelagon
No treatment-related effects on melanin density were observed following single doses of dersimelagon (Part A). In Part E, apparent treatment-related increases in melanin density during the treatment period were observed in participants receiving 150 and 300 mg of dersimelagon compared with those receiving placebo (Fig. 2). At day 15, mean changes from baseline in the average melanin density were 0.07%, 1.43%, 7.71%, 10.22%, and –2.11% in the placebo, 30-mg, 150-mg, 300-mg, and 450-mg dersimelagon groups, respectively, and did not reach a plateau during this time frame. The increases in melanin density were maintained in the 150- and 300-mg dersimelagon groups up to day 29, with signs of reversibility observed at day 57.
Mean percent change from baseline in average melanin density over time (Part E). Note: In participants receiving 300 mg of dersimelagon, 4 did not take study drug on day 14, and 2 did not take study drug on days 13 and 14. In participants receiving 450 mg of dersimelagon, all were Fitzpatrick skin type V, and 1 participant did not take study drug on days 12, 13, and 14
Pharmacokinetics in rats and monkeys
Dersimelagon was rapidly absorbed in rats and monkeys following oral administration. The bioavailability was 7.2% and 6.9% at 1 and 3 mg/kg in rats, respectively, and 31% in monkeys (eTable 4). The t1/2 was approximately 2 h in rats and 5 h in monkeys. Of note, Cmax and AUC0–last increased in a greater than dose-proportional manner between 0.3 and 1 mg/kg and tended to increase with doses between 1 and 3 mg/kg when assessed in rats.
Plasma protein binding of dersimelagon
The in vitro plasma protein binding of dersimelagon free base ([14C] dersimelagon free base) in rats, cynomolgus monkeys, and humans is shown in eTable 5. The plasma protein bindings of [14C] dersimelagon free base at concentrations of 0.1, 1, and 9 µg/mL were 98.3%, 98.2%, and 97.8% in rats; 97.2%, 96.7%, and 97.3% in cynomolgus monkeys; and 98.3%, 98.4%, and 98.2% in humans, respectively.
Interspecies scaling
The human Cmax and AUC at an oral dose of 100 mg of dersimelagon predicted from animal PK data are shown in Table 6 in comparison to actual results in humans. The predicted Cmax by several allometric methods was within threefold of actual Cmax, and the predicted AUC was generally estimated to be lower than the actual AUC, except for allometry with unbound clearance approach, which was almost equal to actual AUC.
Discussion
The present report describes the first-in-human SAD and MAD trial of oral dersimelagon conducted in healthy volunteers. Dersimelagon was generally well tolerated following single oral doses between 1 and 600 mg and multiple oral doses between 30 and 450 mg, including in female, Black, and older participants. The most commonly reported TEAEs in participants receiving multiple doses of dersimelagon (Part E) were related to skin pigmentation changes, including lentigo and skin hyperpigmentation. These TEAEs are similar to those previously reported in the phase 2 ENDEAVOR study [6], which investigated the safety and efficacy of dersimelagon in patients with EPP and XLP, with the most common TEAEs being nausea (27.9%), ephelides (23.5%), and skin hyperpigmentation (20.6%). These TEAEs related to changes in skin pigmentation may be attributable to the study drug based on the pharmacological effects of dersimelagon by virtue of its mechanism of action as a selective MC1R agonist.
The pharmacokinetics of dersimelagon in rats and monkeys following intravenous administration indicated a moderate volume of distribution, clearance, and half-life. Oral bioavailability was low in rats and moderate in monkeys. In the clinical trial, dersimelagon was rapidly absorbed following single oral doses, with exposure appearing to increase in a slightly more than dose-proportional manner, similar to that observed in rats following oral administration of dersimelagon. Further, similar PK properties of rapid absorption and high plasma protein binding were observed for dersimelagon in both humans and animals from the present study. In the drug discovery process, the prediction of human PK of a new chemical entity is routinely performed using animal PK data. In this report, the extent to which the predicted human PK calculated from animal PK data of dersimelagon was consistent with the actual human PK was retrospectively investigated. The predicted human Cmax values were generally in good agreement with the actual human Cmax and were within twofold of the actual Cmax except for the unbound clearance approach method. The predicted human AUC values ranged from one-third to one-fifth of actual AUC for 3 methods, but were within twofold of actual AUC for the other two methods. Overall, the usefulness of commonly used human PK prediction methods was demonstrated.
There were no statistically significant effects of age or race on the PK profile of dersimelagon; however, increased exposure was observed in females (vs males). This difference can most likely be attributed to differences in the body weight generally observed in male versus female participants. Our findings suggest that future development of a population PK model will be useful to evaluate the influence of factors such as body weight, sex, race, and ethnicity on the PK profile of dersimelagon. Furthermore, based on the mean trough concentration ratios, steady state was generally reached by 5 days of multiple dosing, which may be indicative of the time frame necessary to see any treatment effects of dersimelagon.
No treatment-related effects on melanin density were observed following single doses of dersimelagon (Part A). However, in the MAD study (Part E), treatment-related increases in melanin density were observed in the 150- and 300-mg groups compared with the placebo group during the treatment period. This is consistent with previous preclinical reports in which selective activation of MC1R by dersimelagon led to increases in skin pigmentation (eumelanin production) in both in vitro and in vivo animal studies [5]. To our knowledge, dersimelagon is the first orally available compound that has demonstrated increases in melanin density in humans. Of note, increases in melanin density were not observed in the 450-mg group. Only participants with Fitzpatrick skin type V were included in the 450-mg cohort, limiting comparison of PD effects of dersimelagon in this cohort. Taken together, the findings of this study suggest that dersimelagon may have the potential to increase pain-free light exposure in patients with EPP and XLP due to its potential photoprotective effects.
In a recently completed phase 2, randomized, multicenter, placebo-controlled clinical trial (ENDEAVOR), oral administration of dersimelagon to patients with EPP or XLP was shown to increase symptom-free light exposure with an acceptable safety and tolerability profile after 16 weeks of treatment [6]. Currently, the only approved pharmacological intervention indicated for use in patients with EPP is afamelanotide (an MC1R agonist) administered as a subcutaneous implant [4]. The availability of dersimelagon as an oral formulation will confer advantages, namely noninvasiveness and convenience, for the treatment of patients with EPP or XLP.
Conclusions
In this first-in-human phase 1 study, dersimelagon was generally well tolerated following oral administration and demonstrated a generally consistent PK profile across diverse groups of healthy participants. An effective and safe orally administered treatment will address an important unmet need for patients with EPP and XLP, especially for pediatric and adolescent patients who have had no approved pharmacological options to date. Treatment-related increases in melanin density following multiple doses of dersimelagon support further investigation into the photoprotective effects of dersimelagon. A recently completed phase 3 study (ClinicalTrials.gov ID: NCT04402489) evaluated the efficacy and safety of dersimelagon in adults and adolescents with EPP and XLP.
Data availability
The datasets generated during and/or analyzed in this study are available from the corresponding author upon reasonable request.
References
Erwin AL, Balwani M (2021) Porphyrias in the age of targeted therapies. Diagnostics 11:1795. https://doi.org/10.3390/diagnostics11101795
Balwani M (2019) Erythropoietic protoporphyria and X-linked protoporphyria: pathophysiology, genetics, clinical manifestations, and management. Mol Genet Metab 128:298–303. https://doi.org/10.1016/j.ymgme.2019.01.020
Puy H, Gouya L, Deybach JC (2010) Porphyrias Lancet 375:924–937. https://doi.org/10.1016/S0140-6736(09)61925-5
Scenesse [package insert] (2019) West Menlo Park (CA): Clinuvel, Inc
Suzuki T, Kawano Y, Matsumoto A, Kondo M, Funayama K, Tanemura S, Miyashiro M, Nishi A, Yamada K, Tsuda M, Sato A, Morokuma K, Yamamoto Y (2022) Melanogenic effect of dersimelagon (MT-7117), a novel oral melanocortin 1 receptor agonist. Skin Health Dis 2:e78. https://doi.org/10.1002/ski2.78
Balwani M, Bonkovsky HL, Belongie KJ, Anderson KE, Takahashi F, Irizarry A, Amster M, Bissell DM, Wang B, Hazan L, Parker CJ, Cordasco E, Levy C, Desnick RJ (2020) Erythropoietic protoporphyria: phase 2 clinical trial results evaluating the safety and effectiveness of dersimelagon (MT-7117), an oral MC1R agonist. Blood 136:s51. https://doi.org/10.1182/blood-2020-142467
Fitzpatrick TB (1988) The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol 124:869–871. https://doi.org/10.1001/archderm.124.6.869
Dwyer T, Muller HK, Blizzard L, Ashbolt R, Phillips G (1998) The use of spectrophotometry to estimate melanin density in Caucasians. Cancer Epidemiol Biomarkers Prev 7:203–206
Dwyer T, Blizzard L, Ashbolt R, Plumb J, Berwick M, Stankovich JM (2002) Cutaneous melanin density of Caucasians measured by spectrophotometry and risk of malignant melanoma, basal cell carcinoma, and squamous cell carcinoma of the skin. Am J Epidemiol 155:614–621. https://doi.org/10.1093/aje/155.7.614
Mahmood I (2005) Interspecies scaling of biliary excreted drugs: A comparison of several methods. J Pharm Sci 94:883–892. https://doi.org/10.1002/jps.20313
Mahmood I, Balian JD (1996) Interspecies scaling: predicting clearance of drugs in humans. Three different approaches. Xenobiotica 26:887–895. https://doi.org/10.3109/00498259609052491
Feng MR, Lou X, Brown RR, Hutchaleelaha A (2000) Allometric pharmacokinetic scaling: Towards the prediction of human oral pharmacokinetics. Pharm Res 17:410–418. https://doi.org/10.1023/A:1007520818956
Tang H, Mayersohn M (2005) A novel model for prediction of human drug clearance by allometric scaling. Drug Metab Dispos 33:1297–1303. https://doi.org/10.1124/dmd.105.004143
Acknowledgements
We wish to thank Takayuki Kifuji and Kazumi Hyoudou for designing the first-in-human study, and Akihide Tsujimoto and Shio Maruyama of Mitsubishi Tanabe Pharma Corporation for performing the pharmacokinetic animal studies. Medical writing assistance was provided under the direction of the authors by Rajgopal Yadavalli, PhD, and Brittany Eldridge, PhD, of Cadent Medical Communications, LLC, a Syneos Health® group company, and was supported by Mitsubishi Tanabe Pharma Corporation.
Funding
This study was sponsored by Mitsubishi Tanabe Pharma Corporation.
Author information
Authors and Affiliations
Contributions
TM contributed to the concept and design of the study; RI and YI are responsible for the acquisition of data. AO, KO, RI, and CF contributed to the analysis and interpretation of data; KO and SN performed the statistical analysis; and all authors were responsible for drafting and critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Prior to study initiation, the protocol and all other appropriate documents were reviewed and approved by an Independent Ethics Committee and local regulatory authorities. The study was conducted in accordance with the ethical principles stated in the Declaration of Helsinki, the International Conference on Harmonisation for Good Clinical Practice guidance, and all local and regional applicable laws and regulations. Prior to the performance of any study-related assessments and procedures, all participants signed a written informed consent form with details of the trial treatment, procedures, and potential risks.
Competing interests
All authors are employees of Mitsubishi Tanabe Pharma Corporation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ogasawara, A., Ogawa, K., Ide, R. et al. Results from a first-in-human study of dersimelagon, an investigational oral selective MC1R agonist. Eur J Clin Pharmacol 79, 801–813 (2023). https://doi.org/10.1007/s00228-023-03476-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03476-6